Chapter 2: Defining and engaging with communities of place
The approach to place-based health planning described in these guidelines focuses on community engagement in planning within a ‘community of place’. A community of place refers to a specific geographic area where a local society, defined by its structures, organisations, and processes, functions to facilitate collective action.[1] A town could be a community of place and defined by geographic town locality, or by administrative boundaries such as local government area (LGA), for example. A community of place could also be a series of localities in close proximity to each other that fall into the same Health Service catchment, or tend to work together due to geography, and shared resources or services such as visiting health professionals.
Identification of a need to undertake health planning may have various origins. For example, there may be a need for planning identified within a local community by individuals, groups or organisations. Larger organisations with responsibilities for health across a geographic region, such as a PHN or HHS, may identify a need to take a deep dive into the health and service needs of particular communities. Regardless, defining the ‘community of place’ is essential to inform the extent of context mapping, engagement activities and anticipated project outcomes.
Once the community, or place, has been defined, if the work is being driven by a party external to the place, such as a university, or urban-based unit within a HHS, or PHN, early engagement and consultation with local key stakeholders is required to determine interest in undertaking such work and establish buy in. Local interest in the work, at the current time, is essential, or encouraging participation will be very challenging.

Defining and prioritising a community of place for place-based health planning for the project
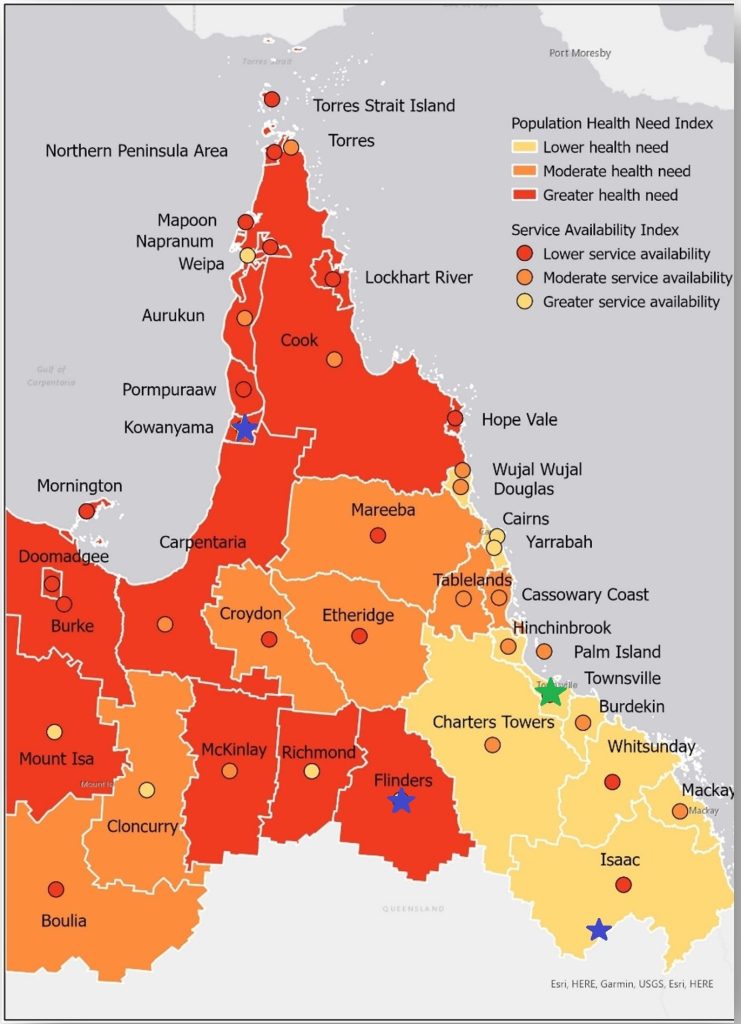
Through the project, a broad approach was undertaken, defining a community of place at the level of local government. LGAs across the five northern HHS districts were ranked in order of unmet need using planning tools that were developed – the Northern Queensland Health Atlas and a gap analysis assessing unmet need. Initially, the Northern Queensland Health Atlas was compiled bringing together data about communities across the region, to help make data more accessible and to inform planning and decision making.

The Atlas is an interactive online platform that presents data on population, health status and behaviours, hospital use, workforce, health service provision, and service locations through detailed maps. It enables users to overlay various data types to compare and explore differences across North Queensland communities, helping to build a deeper understanding of each place. This planning tool supports the identification of service gaps, underserved areas, and potential inefficiencies caused by service duplication. The Atlas features more than 200 data layers and is complemented by a Data Sources and Information Booklet that outlines the origins and details of the included data. Challenges experienced by the team in accessing data have been published elsewhere (Figure 2.1).
- Project Technical Reference Group
- TAAHC Board (including HHS Executives)
- TAAHC Clinical Leadership Group
- Better Health NQ Health Needs Assessment / Local Areas Needs Assessment working group
- Other individual stakeholders (e.g. key HHS staff).
Other criteria were also considered in prioritisation, including assessing whether there was actually interest among the local community stakeholders in participating in place-based planning at the current time; and for the particular purposes of the project, we wanted coverage of a range of different community types and regions to maximise learnings. Once the communities were prioritised, further consultation was undertaken with key stakeholders in each community to determine if there was interest in participating in the project at the current time.

Northern Queensland Health Atlas. Available at: https://arcg.is/5a4Xq
A Gap Analysis of Health Needs and Services in the Northern Queensland Region June 2022. Available under project resources at: https://www.taahc.org.au/research/integrating-health-care-planning-for-health-and-prosperity-in-north-queensland/
Topp, S. M., Thompson, F., Johnston, K., Smith, D., Edelman, A., Whittaker, M., Rouen, C., Moodley, N., McDonald, M., Barker, R., & Larkins, S. (2023). Democratising data to address health system inequities in Australia. BMJ Global Health, 8, Article e012094. https://doi.org/10.1136/bmjgh-2023-012094
.

How to start early engagement with a community to confirm interest
A key requirement for effective place-based health planning is ensuring that the local community has both the interest and capacity to participate in planning activities. It’s also important to consider the timing of engagement in relation to other ongoing initiatives and events.
In northern Queensland, a Council is the governing body of a local area, tasked with managing local affairs, including planning for community needs and providing public services for the local community. The Mayor and Councillors are elected to represent the community and make decisions on their behalf. As a leader and representative of the local community, the Mayor in each community was contacted to discuss the project and what it involved, and to ascertain whether there may be interest, capacity, and it being the ‘right time’ on behalf of the broader community (Figure 2.3).
Local and regional health service managers should ideally play a key role in prioritising locations. In some cases, early engagement with local health service managers, including Aboriginal and Torres Strait Islander Community Controlled Health Organisations/Services, may be necessary in the lead up to the work, to establish relationships and secure their support. Taking proactive steps in this regard can help ensure a well-coordinated approach.
Processes and approval requirements may vary in different communities, especially Aboriginal and Torres Strait Islander communities. In the remote Aboriginal community of Kowanyama, the local Council outlines processes for external stakeholders to make contact on its website.

- Taylor J., Braunack-Mayer A., Cargo M., Larkins S., & Preston R. (2013). A role for communities in primary prevention of chronic illness? Case studies in regional Australia. Qualitative Health Research, 23(8), 1103-13. https://doi.org/10.1177/1049732313494482 ↵
- Impact Co. (2018) North Western Melbourne Primary Health Network - After hours primary health care: Gap analysis and recommendations. https://nwmphn.org.au/wp-content/uploads/2019/03/181219-NWMPHN-After-Hours-Gap-Analysis-Final-Report-FINAL.pdf ↵
Primary Health Network
Hospital and Health Service
Local Government Area
Tropical Australian Academic Health Centre
North Queensland

