1.7 Interprofessional Communication
Kimberlee Carter, Marie Rutherford, Connie Stevens (adapted by Brock Cook)
Learning Objectives
- recognise the role of interprofessional communication in healthcare settings
- describe the elements and goals of interprofessional communication
- explore behavioural practices influencing interprofessional care teams
- apply strategies for managing conflict within the context of interprofessional teams.
Introduction
Interprofessional communication occurs when health professionals communicate with each other, with patients, their families, and with the community in general. Multidisciplinary or interdisciplinary are terms used to describe the healthcare makeup of healthcare teams. Individuals from different healthcare disciplines approach a patient or care of a patient from their own perspective. The primary goal of these teams is to integrate expertise from separate disciplines into a single consultation to support patient care and outcomes. This encompassing care is often referred to using the short form IPC meaning interprofessional care.
Assessing What You Already Know
Consider your pre-existing knowledge surrounding interprofessional teams as you complete this activity
Role of Interprofessional Communication in Healthcare
As the nature of healthcare continues to evolve the more interwoven healthcare professionals are in coordinating care following an interprofessional-focused approach. In the past healthcare management was often physician or disease-focused. Recently, this foundation has since migrated to a robust team of health professionals working together for patient care and disease prevention. This seemingly harmonious approach will not occur without reflective practice, mindful effort, and an understanding of the importance of communication. Learning to function effectively within the interprofessional dynamic begins through the establishment of mutual respect and trust.
Establishing Trust-Interprofessional Practices
As a self-check consider the following definition and the reflective questions within the context of communication.
Trust (noun): Firm belief in the reliability, truth, or ability of someone or something; confidence or faith in a person or thing (Oxford English Dictionary; Oxford University Press, n.d.).
As in “good relationships are built on trust.”
Questions for reflection:
- Does my personal competence and follow-through establish trust with others?
- What experiences can I offer to support cooperation while working with others?
- How do I manage stressful communication-based situations with others?
Elements of Interprofessional Communication
Six interdependent competency domains have been identified to achieve the goal of interprofessional collaboration (Canadian Interprofessional Health Collaborative [CIHC], 2010, cited Lapum et al., 2020). These are defined as the “knowledge, skills, attitudes, and values that shape the judgements essential for interprofessional practice” (CIHC, 2010, cited in Lapum et al., 2020) and include:
- interprofessional communication
- patient/client/family/community-centred care
- role clarification
- team functioning
- interprofessional conflict resolution
- collaborative leadership.
Interprofessional Communication Competency
Explored in the 1.5 Professional Communication chapter, elements of effective communication apply relative to interprofessional communication.
Behavioural examples to strengthen interprofessional communication include the following:
- communicate clearly using terminology understood by the collaborative team, patients, and family
- ensure complete information is provided as directed
- be responsive to changing needs and circumstances
- provide information in a timely manner, avoid withholding sensitive information
- use recognised and accepted communication channels (checklists and templates are helpful)
- review updated information when it is available
- demonstrate respect with all members of the interprofessional team
- model and create an environment of mutual trust, respect for privacy and confidentiality, while maintaining patient dignity.
Patient/Client/Family/Community-Centred Care Competency
Patient-centred care encircles the foundational belief clients/patients and their families are partners in the design and development of care plans, all functioning as members of one team. Input is gathered collaboratively from team members to support engagement through each stage and process of care plan implementation.
Behavioural examples of patient-centred care involve:
- actively seeking clarification from patients, their families, and the interprofessional team when involved with the planning, coordination, and implementation of patient care plans
- support and encourage access to community resources and involvement
- promote access to preventative care measures by applying therapeutic communication strategies and information sharing.
Role Clarification Competency
This involves developing an understanding of your role and the role of all collaborative professionals on the team. The ability to apply this knowledge correctly achieves care goals for patients and supports the health of the community within the bigger picture. This understanding helps to identify gaps in care, addresses duplication of resources, and enhances the implementation of care plans. The healthcare administrator can model a variety of behaviours to support this.
Behavioural examples of role clarification include:
- demonstrate an understanding of your role as well as the roles of each member of the team
- consider the roles of members while respecting the diversity of the team members as they relate to patient care and team dynamics
- utilise professional development opportunities to expand knowledge of interprofessional educational practices
- practice self-awareness in view of one’s limitations and the need for consultation with other members of the healthcare team based on roles and professional scope.
Team Functioning Competency
When interprofessional healthcare teams form it is common practice to establish ground rules of how the team will work together.
Behavioural examples of team functioning include:
- Recognise and share with the interprofessional team individual and systemic power discrepancies and gaps expressed by patients and their families.
- Participate in the development of team values and goals.
- Support team psychological safety to establish a sense of confidence that the team will not embarrass, reject or punish someone for speaking up.
- Advocate against and avoid harmful behaviour to a team i.e. gossip, destructive comments rumours that impact team morale and development.
Interprofessional Conflict Competency
Conflict is a natural event occurring when groups or teams are working together. Joan Wagner (2018) provided this insight from the publication Leadership and Influencing Change in Nursing: for centuries, people accepted adversarial disputes and harsh conflict as a by-product of human nature. This acceptance caused people to analyse only how conflict could be resolved, that is, how they could make it go away (Wagner, 2018).
Conflicts and disagreements are inevitable in interpersonal communication. Several factors that influence conflict can include, role boundary concerns, accountability and the scope of practice of those involved in the communication stream. Recognising and managing conflict effectively supports therapeutic communication goals.
Types of Conflict
Categorising and understanding the types of conflict arising assists with framing resolutions. Here are four types of common conflict occurring within interprofessional teams (Wagner, 2018):
- Data/Information. These encompass elements inclusive of, lack of information, interpretation of information, incomplete information, and differing assessment procedures.
- Values. Conflicts related to day-to-day values and self-definition.
- Relationship. These conflicts stem from stereotypes, misperceptions, and poor communication efforts.
- Structural. Conflicts relate to how a situation occurs, who is involved in the decision-making, and unequal power and authority (Wagner, 2018).
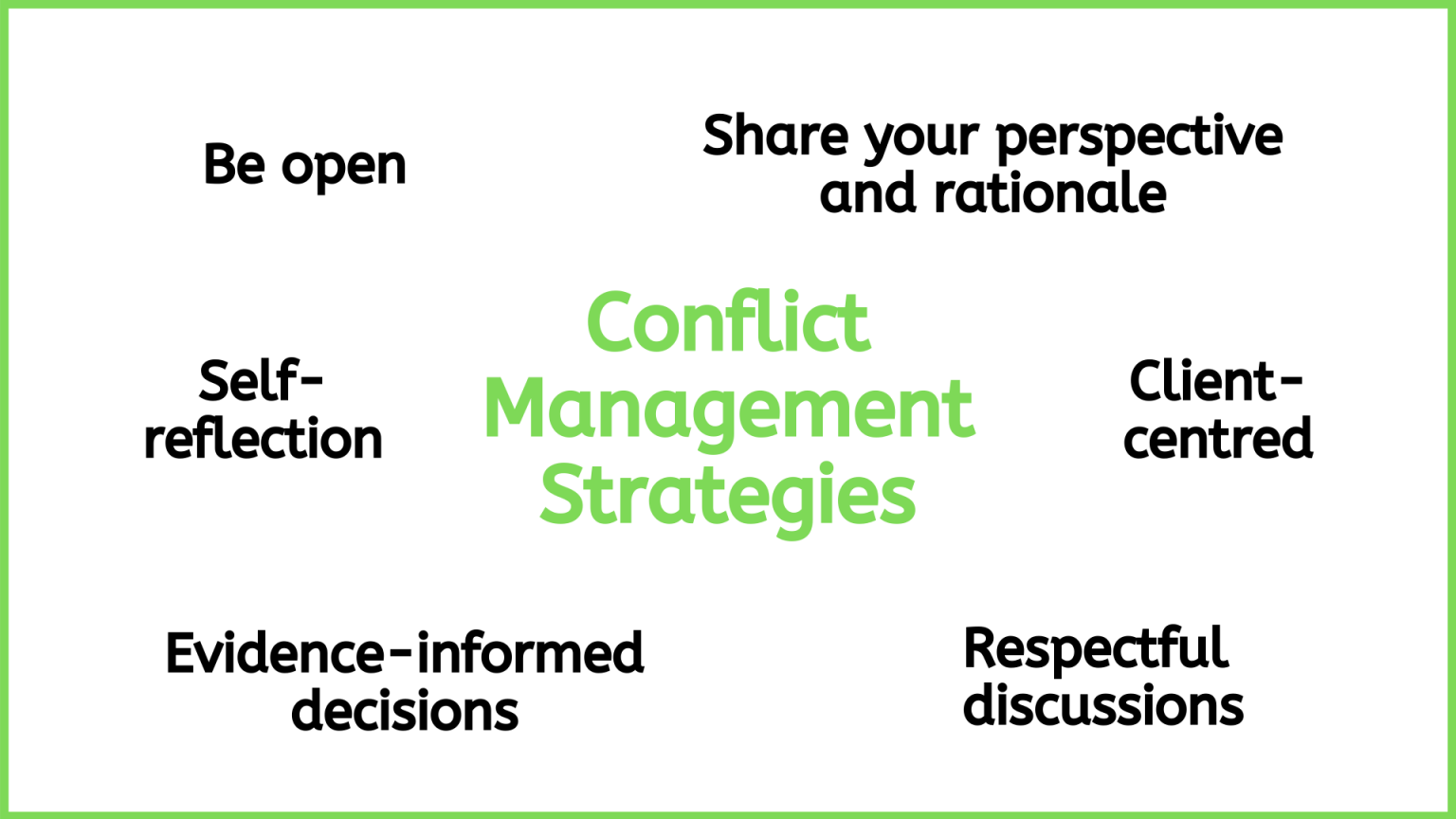
Behaviour examples of interprofessional conflict resolution and management include:
- constructively address potential areas for conflict arising
- seek out solutions to support the resolution or to prevent conflicts
- support mutually agreed solutions in an appreciative manner
- keep an open mind with differing views.
- avoid blaming, and judging for optimal patient outcomes
- communicate with empathy:
- listen without interrupting
- be available for communication opportunities
- demonstrate support
- use a client-centred approach to frame discussions
- use an evidence-informed approach to make decisions
- be open to hearing varying disciplinary perspectives
- engage in self-reflection
- engage in respectful discussions
- reflect on the perspectives of all team members
- share your perspective and rationale (Lapum et al., 2020).
Collaborative Leadership
Collaborative leadership transpires when interprofessionals work together with patients and families, to provide as well as assess, the care and the services provided. Each professional understands their role and accountability all with the goal of promoting healthy outcomes.
Behavioural examples of collaborative leadership include:
- encourage participation in the coordination of planning care to achieve care goals
- designate accountability, recognise and address role overlap
- respectfully acknowledge appropriate expertise when needed in order to help guide patient/client needs
- advocate for patients, clients, and their families to facilitate the integration of care.
Collaborating with Interprofessional Teams to Support Patient Outcomes
Collaboration is especially significant in the healthcare environment to meet the increasingly complex demands of patients with multiple comorbidities. Collaboration pools resources to facilitate improvements in cost, availability, and quality of care (Tsakitzidis et al., 2016).
Scenario
Social media can be used to create virtual communities in healthcare environments. Many individuals also engage in social media outside of their professional practice. Typically, you do not have members of your organisation on your personal social media platforms. Today, a friend of yours mentioned she saw a personal post by a member of your team which stated: “I have never met a more difficult group of HCA’s in our organisation”
Reflecting on this. Consider these questions:
- What would you do?
- How can this be effectively handled? Should it be handled?
Check Your Understanding
Apply your knowledge from the chapter as you complete this review activity.
Key Takeaways
In this chapter, you have:
- explored the elements involved in interprofessional communication
- reviewed the six domains of interprofessional competency framework as applied within the healthcare environment
- highlighted the behaviours to support conflict resolution when arises within the team and focused on areas of collaborative opportunities to improve care outcomes richly available through interprofessional teams.
References
Lapum, J., St-Amant, O., Hughes, M., Garmaise-Yee. J., & Lee, C. (2020). Introduction to communication in nursing. Toronto Metropolitan University. https://openlibrary.ecampusontario.ca/catalogue/item/?id=04e7dd2-8ba)-4be5-87c8-8cda40433a8
Oxford University Press. (n.d.). Trust. In Oxford English dictionary. https://doi.org/10.1093/OED/5777528687
Tsakitzidis, G., Timmermans, O., Callewaert, N., Verhoeven, V., Lopez-Hartmann, M., Truijen, S., Meulemans, H., & Van Royen, P. (2016). Outcome indicators on interprofessional collaboration interventions for elderly. International Journal of Integrated Care, 16(2), 5. https://doi.org/10.5334/ijic.2017
Wagner, J. (2018). Leadership and influencing change in nursing. University of Regina Press. https://openlibrary.ecampusontario.ca/catalogue/item/?id=00e26b2d-3c99-4955-9173-fe6dee00a840
Attribution Statement
Carter, K., Rutherford, M., & Stevens, C. (2022). Therapeutic communication for health care administrators. Conestoga College. https://ecampusontario.pressbooks.pub/therapeuticcommunicationforhealthofficeadministrators/. Used under a CC BY-NC-SA 4.0 licence.