10.2 Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Non-Steroidal Anti-inflammatory Drugs (NSAIDs)
Non-Steroidal Anti-inflammatory Drugs (NSAIDs) are a class of drugs that includes up to 50 drug agents globally. In Australia there are around 12 different NSAIDs available with common examples including:
- Aspirin
- Ibuprofen (Nurofen, Advil)
- Diclofenac (Voltaren)
- Naproxen (Naprosyn)
- Indometacin or indomethacin (Indocid)
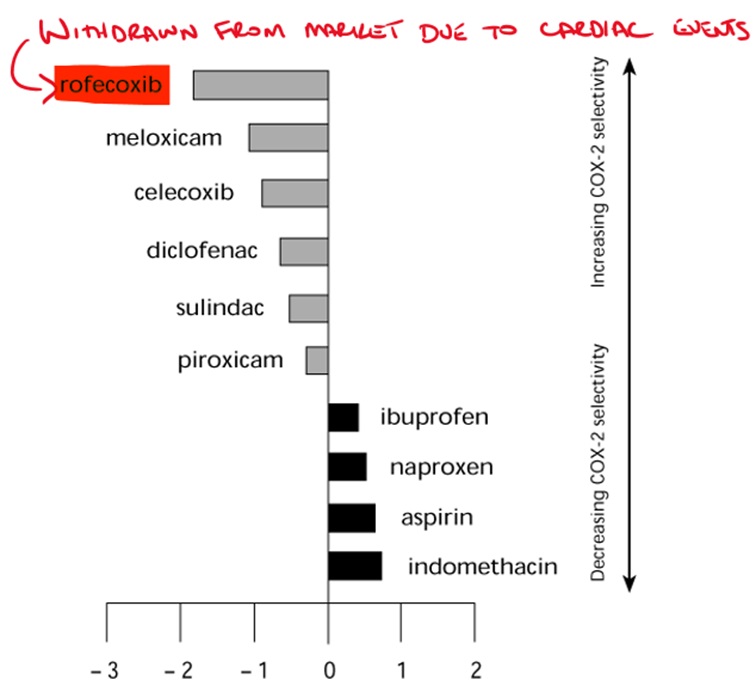
- Meloxicam (Mobic) – COX-2 selective at lower doses
- Celecoxib (Celebrex) – COX-2 selective
NSAIDs have analgesic, anti-inflammatory, and antipyretic properties.
About 60% of patients will respond to any NSAID; those who do not respond to one may respond to another.
Watch the following YouTube video on NSAIDs
NSAID Mechanism of Action
You will recall that NSAIDs have three primary therapeutic uses:
- Anti-inflammatory – decrease in prostaglandin E2 and prostacyclin reduces vasodilation. Reduced vasodilation leads to reduced oedema however inflammatory cells are not reduced.
- Analgesic – reduced prostaglandin levels lead to less sensitisation of nociceptors to inflammatory mediators including bradykinin and serotonin. Analgesia of headache may be related to reduced vasodilation.
- Antipyretic – prevent the formation of prostaglandins within the central nervous system that are responsible for elevating the hypothalamic temperature set point.
Thinking back to transduction within nociceptors at the sensory terminal of the 1st order neuron in response to noxious stimuli, you will recall that prostaglandins are one of many potential triggers/sensitisers for depolarisation. Prostaglandins are primarily sensitisers, assisting bradykinins, 5-HT, histamine and ATP to trigger depolarisation.
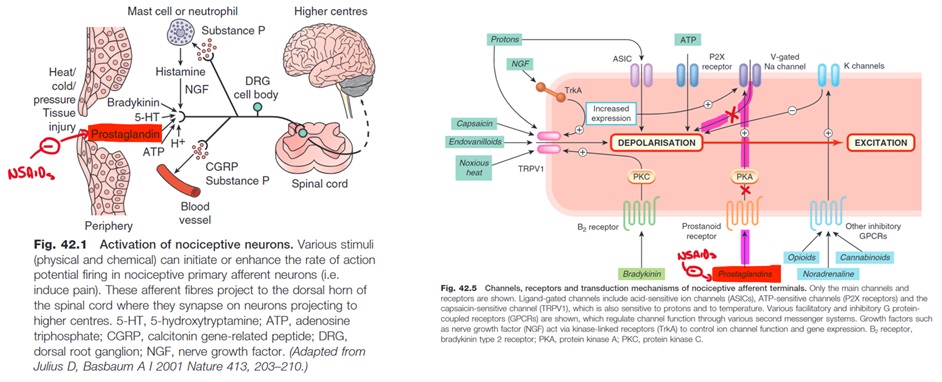
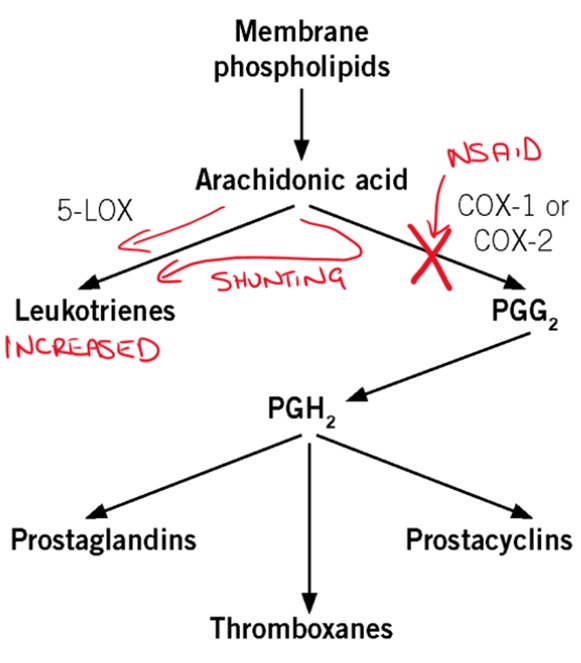
Arachidonic acid is converted by cyclo-oxygenase (COX) into prostaglandins. NSAIDs inhibit the action of COX and therefore prevent the formation of prostaglandins.
You may recall that there are two main types of COX enzymes, COX-1 and COX-2:
- COX-1 is thought to be primarily involved in ‘normal’ physiological processes
- gastric mucosal production
- renal function
- platelet function
- COX-2 is induced by tissue injury and inflammation
Most NSAIDs are non-selective – they inhibit both COX-1 and COX-2.
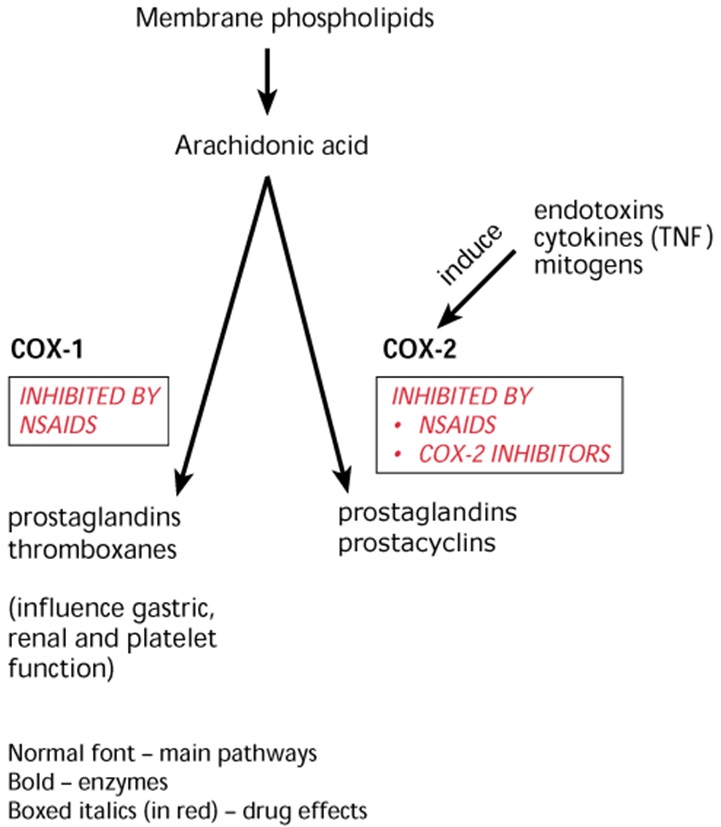
COX-2 selective NSAIDs (COX-2 Inhibitors) were created to minimise the common gastrointestinal side effects associated with non-selective NSAIDs.
In the short term (eg 6 weeks) COX-2 Inhibitors produce less gastrointestinal ulcers and bleeding than non-selective NSAIDs. Unfortunately, COX-2 Inhibitors have been associated with an increase in cardiovascular events and possess the same negative renal effects as non-selective NSAIDs. Additionally, the gastrointestinal benefits diminish with long term use or if used in combination with low dose aspirin.
Side effects of NSAIDs
There are numerous side effects associated with NSAID use. Many of the side effects are directly linked to COX inhibition.
Gastrointestinal impacts of NSAIDs
Gastrointestinal side effects are particularly common with non-selective NSAIDs however they still occur with COX-2 Inhibitors. The risk of GI complications are increased with higher doses and longer duration of use.
You will recall from gastrointestinal pharmacology that prostaglandin E2 (PGE2) plays an important role in stimulating protective mucous and bicarbonate production in the stomach while also reducing acid generation. Inhibition of COX-1 blocks these beneficial effects leading to dyspepsia, nausea, vomiting, gastric ulceration, duodenal ulceration, GI bleeding and possible perforation of ulcers.
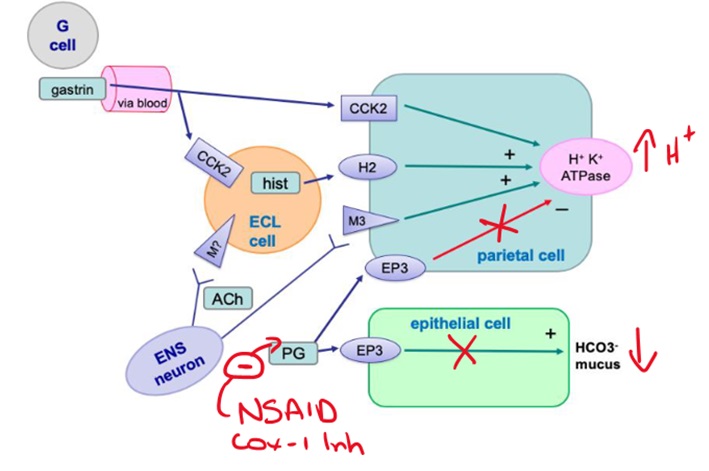
As already discussed, NSAIDs with COX-2 selectivity produce less GI side effects (eg celecoxib). Of the non-selective agents, diclofenac and ibuprofen appear to have lower risk while ketoprofen and piroxicam are associated with the highest risk of GI complications. Although piroxicam demonstrates a marginal COX-2 preference, it retains significant COX-1 inhibition and has a particularly long half life that increases the risk of GI complications.
The risk of peptic ulcers is increased when other risk factors are present.
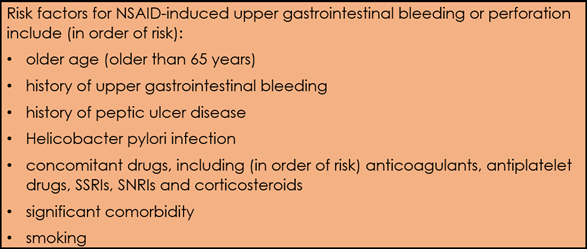
Minimising the dose and duration of NSAID, prophylactic proton pump inhibitor use, and other risk factor modification (eg smoking cessation) can reduce the risk.
Cardiovascular impacts of NSAIDs
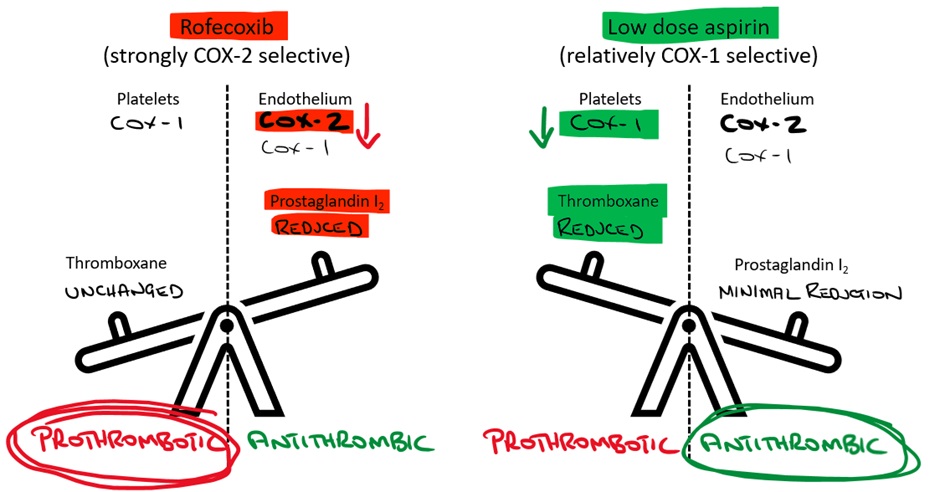
As you will recall from cardiovascular pharmacology, COX-1 is responsible for producing thromboxane-A2, which stimulates platelet aggregation. Non-selective NSAIDs that block COX-1 will therefore reduce platelet adhesion and lead to an increased risk of bleeding and bruising. This is used therapeutically in patients with ischaemic heart disease. Aspirin irreversibly inhibits COX-1 whereas the other non-selective NSAIDS produce reversible platelet inhibition.
COX-2 produces prostaglandin-I2 (PGI2 or prostacyclin) which causes vasodilation and inhibition of platelet aggregation. Selective COX-2 inhibitors prevent the formation of prostaglandin-I2 while they do not inhibit thromboxane formation. As such, selective COX-2 inhibitors are associated with prothrombic activity (reduced PGI2 to offset thromboxane), a higher risk of myocardial infarction and stroke and should be avoided in patients at high risk of these events.
NSAIDs exhibit additional cardiovascular impacts on blood pressure via their renal effects.
Renal impacts of NSAIDs
COX-1 and COX-2 are present within the kidneys and have an important physiological role in the regulation of renal perfusion and blood pressure control. We have already discussed that PGI2 (prostacyclin) is an important vasodilator, as is PGE2.
In the kidney, PGE2 and PGI2 cause vasodilation of the afferent arteriole. NSAIDs inhibit the production of these prostaglandins resulting in vasoconstriction of the afferent arteriole. This leads to a reduction in renal perfusion. Prostaglandins contribute to a variety of other functions within the renal medulla that are not discussed in this module.
In response to reduced renal perfusion, compensatory mechanisms are activated including sodium and water retention. Sodium and water retention leads to an increase in blood pressure (3-6mmHg) and can contribute to development of oedema. Patient with heart failure, hypertension and other cardiovascular conditions are therefore typically advised to avoid NSAIDs (except low dose aspirin) where possible.
The use of NSAIDs should be avoided in patients with risk factors for acute kidney injury (AKI) including dehydration, the elderly and those with chronic kidney disease/previous AKI or taking other medications that may place them at risk.
Of particular importance is the ‘Triple Whammy’ where the combination of a diuretic (eg loop diuretic) or dehydration, NSAID and an ACE-Inhibitor or ARB lead may lead to a significant AKI.
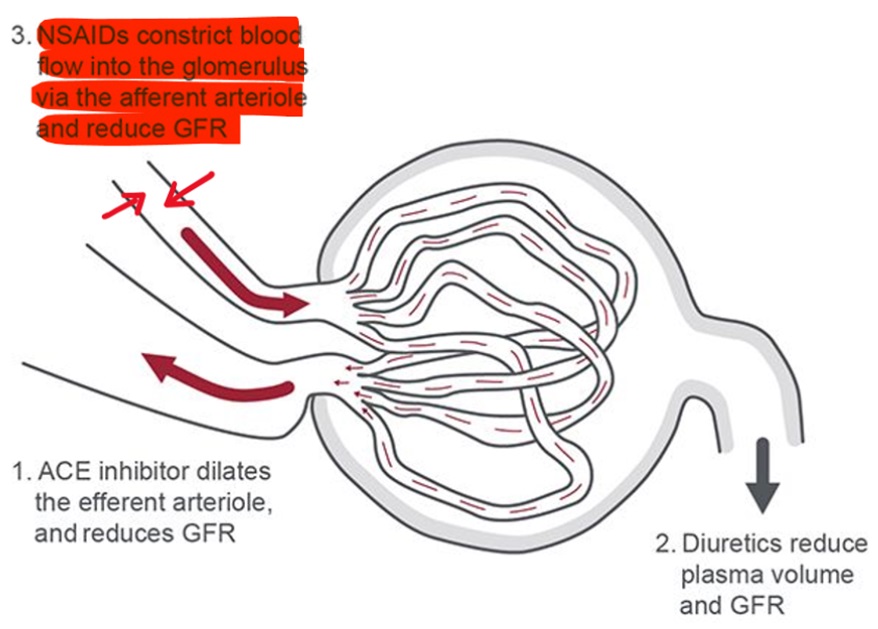
Due to the relative COX-1 selectivity of low dose aspirin, the renal impacts of other NSAIDs are not observed with low dose aspirin <150mg/day but at higher analgesic doses aspirin exhibits the same renal effects as other NSAIDs.
Respiratory impacts of NSAIDs
NSAIDs are associated with bronchospasm in some patients. The risk is higher in patients with asthma and it is sometimes termed aspirin-sensitive asthma (but can occur with any NSAID). Between 8-20% of asthmatic patients may suffer bronchospasm with NSAID use and in rare cases this can lead to death.
Inhibition of COX leads to shunting of arachidonic acid breakdown via 5-lipoxygenase (5-LOX). This results in increased levels of leukotrienes which can produce bronchospasm in susceptible people. This effect is greater with non-selective NSAIDs but has also been reported with COX-2 inhibitors.
🎥 Watch this video
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
