10.5 Adjuvants for Neuropathic Pain
Antidepressants for Neuropathic Pain
Tricyclic antidepressants (TCAs) and serotonin/noradrenaline reuptake inhibitors (SNRIs) are used in the management of neuropathic pain. Common examples include the TCAs amitriptyline and nortriptyline and SNRIs duloxetine and venlafaxine. Similar to their use in depression, the analgesic effects may take several weeks to develop.
TCAs and SNRIs are not known to have significant direct effects on opioid receptors or prostaglandin production however they lead to increased concentrations of serotonin and noradrenaline in the synapses of neurons in the descending pain pathway (and other sites). As you will recall, the descending pain pathway neurons are serotonergic (RVM) and noradrenergic (LC).
Increased concentrations of these monoamines lead to increased descending output to the dorsal horn and inhibition of the afferent pain pathway. TCAs also demonstrate inhibition of sodium channels, N-type calcium channels amongst others which may contribute to clinical effects.
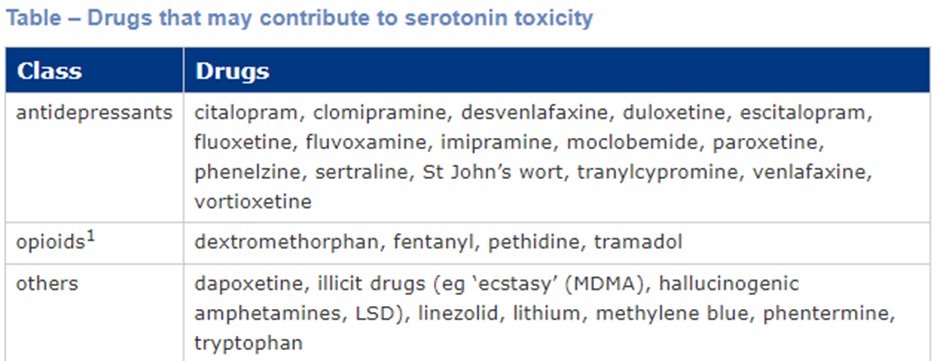
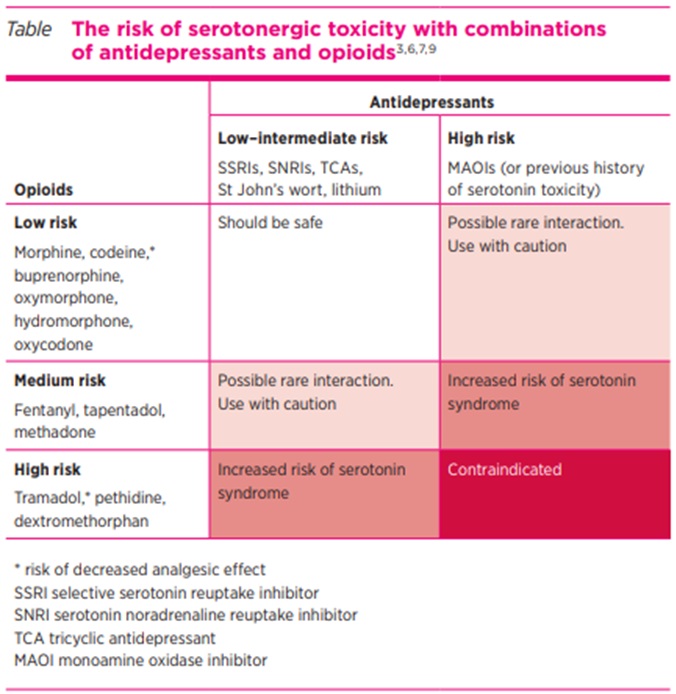
Caution is required when combining TCAs with opioids due to the risk of sedation and respiratory impairment. SNRIs and tramadol have been shown to contribute to serotonin toxicity especially if used in combination with serotonergic agents (including some opioids).
Refer to last week’s content for additional information regarding side effects and precautions to the use of TCAs and SNRIs.
Gabapentinoids for Neuropathic Pain
Alongside TCAs and SNRIs, gabapentinoids are effective in the management of neuropathic pain. Gabapentin and pregabalin are the two medications in this class.
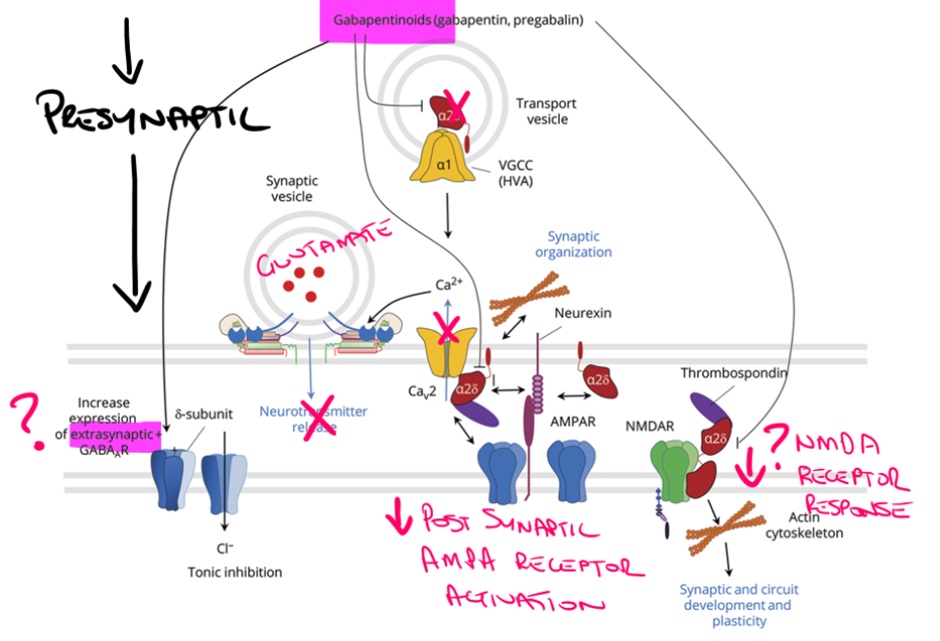
Reduced expression of presynaptic calcium channels leads to reduced calcium influx and subsequently reduced exocytosis of excitatory glutamate at the synapse. Additionally, gabapentinoids also appear to stabilise excitatory NMDA receptor on the post-synaptic neuron and potentially lead to increased inhibitory GABA receptors in higher centres.
Unlike TCAs and SNRIs, the effects of gabapentinoids develop more quickly and for this reason they are often preferred to the antidepressants during acute neuropathic pain however the high risk of side effects and abuse potential can limit gabapentinoid use. TCAs have also demonstrated better efficacy in many studies.
Gabapentinoids are frequently associated with dizziness and balance problems. Weight gain secondary to increased appetite or peripheral oedema is also relatively common.
Euphoria is experienced in approximately 10% of patients and may be more likely with pregabalin than gabapentin due to pregabalins more rapid absorption leading to higher serum concentrations. Antiepileptics, including gabapentinoids, have been associated with a small increase in suicidal thoughts and behaviours.
Gabapentinoids are known to potentiate the effects of opioids and are commonly misused to increase effects of opioids including methadone and buprenorphine (both used in opioid treatment programs) or to gain a ‘high’ while abstaining from opioids for urine drug screening.
Concerningly, combined use of gabapentinoids and opioids is associated with an increase in opioid-related deaths, probably via increased opioid-induced ventilatory impairment.
🎥 Watch this video
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
