1.2 Types of Acetylcholine Receptors and Drugs that commonly interact with Murcarinic Receptors (M-AChR)
John Smithson
Overview
In the parasympathetic nervous system, you now know acetylcholine (ACh) interacts with two main types of receptors: nicotinic receptors and muscarinic receptors. These receptors are distinct in their location, structure, and function:
- Nicotinic Acetylcholine Receptors (nAChRs):
- Location: Nicotinic receptors are primarily found at the synapse between preganglionic and postganglionic neurons within autonomic ganglia. They are also present in the neuromuscular junctions of the somatic nervous system.
- Structure: Nicotinic receptors are ionotropic receptors, which means they are ligand-gated ion channels. When acetylcholine binds to these receptors, they open to allow the influx of sodium (Na+) ions and the efflux of potassium (K+) ions, leading to depolarization and excitation of the postsynaptic neuron.
- Function: In the parasympathetic nervous system, the activation of nicotinic receptors by acetylcholine released from preganglionic neurons triggers an excitatory response in postganglionic neurons, propagating the parasympathetic signal.
- Muscarinic Acetylcholine Receptors (mAChRs):
- Location: Muscarinic receptors are primarily located on the target organs innervated by postganglionic parasympathetic neurons, such as the heart, smooth muscles, and glands.
- Structure: Muscarinic receptors are metabotropic receptors, meaning they are G protein-coupled receptors (GPCRs). When acetylcholine binds to these receptors, it activates G proteins, which then modulate various intracellular signalling pathways.
- Function: Muscarinic receptors mediate various parasympathetic effects depending on the target organ:
- M1 receptors: Found in the central nervous system and gastric parietal cells, they play a role in cognitive functions and stimulate gastric acid secretion.
- M2 receptors: Located primarily in the heart, they reduce heart rate and contractility, contributing to the “rest and digest” effects.
- M3 receptors: Found in smooth muscles and glands, they mediate smooth muscle contraction (e.g., bronchoconstriction, increased gastrointestinal motility) and stimulate glandular secretions (e.g., saliva, mucus).
- M4 and M5 receptors: These receptors are less well characterized but are found in the central nervous system and may play roles in modulating neural activity.
From a pharmacological perspective when targeting the parasympathetic nervous system, we mostly aim to modify acetylcholine interaction with M1, M2 and M3 (M-AChR) receptors. Together, nicotinic and muscarinic acetylcholine receptors enable the parasympathetic nervous system to exert its effects on various organs, contributing to the maintenance of homeostasis and promoting “rest and digest” activities.
Learning Outcomes
Be able to:
- Describe the common uses of relevant anticholinergic and parasympathomimetic drugs.
- Describe the pharmacology of anticholinergic agents as a class.
- Describe the pharmacology and relationship between acetylcholine and the parasympathomimetic drugs.
- Apply knowledge of the parasympathetic nervous system and pharmacology of anticholinergic drugs to predict effect and side effect of these commonly used agents.
Introduction
Post-ganglionic muscarinic receptors are commonly used and are very useful targets for drugs. Normally, these receptors interact with released endogenous acetylcholine to produce a range of homeostatic effects. The two main groups of drugs that interact with post-ganglionic muscarinic receptors are muscarinic antagonists (commonly referred to as anticholinergic agents (or sometimes antimuscarinic agents) and muscarinic agonists (also known as parasympathomimetics). Effectively, anticholinergic agents block the effect of acetylcholine at the M-AChR and muscarinic agonist replicate the effect of acetylcholine at the M-AChR. As you will remember from the previous module, there are 5 main subtypes of muscarinic receptors: M1, M2, M3, M4, M5. Muscarinic receptors M1 to M3 are the most clinically relevant.
The effect of the stimulation of post-ganglionic muscarinic receptors depends on the organ on which the receptor is located. As a generalisation, stimulation of the various subtypes of muscarinic receptors by acetylcholine cause:
Increased pupil constriction and contraction of the ciliary muscle of the eye promoting the flow of aqueous humour and allowing for near focus by the lens (M3).
Bronchoconstriction of the major airways
- Constriction of the smooth muscle in the bronchi causing bronchoconstriction. (M3)
- Increase in respiratory secretions. (M3)
Decreased heart rate and cardiac output
- Decrease in heart rate (negative chronotropic effect), decreased contractility (negative ionotropic effect) and decrease in conduction velocity (negative dromotropic effect). (M2)
- All mediated by the stimulation of the M2 receptor.
Increased motility and gastric secretions of the gut
- Dilatation of the sphincters in the GIT. (M3)
- Increased muscle tone and longitudinal peristaltic waves of the gut resulting in increased motility. (M3)
- Increased acid (M1) and mucus secretion. (M3)
- Increased secretion of the salivary glands. (M3)
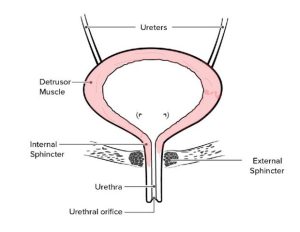
Promotes bladder contraction and urinary sphincter relaxation
- Stimulation of the M3 receptor relaxes the urinary sphincter and increases tone of the detrusor muscles in the bladder.
📺 Watch the vodcast on parasympathetic effect on target organs (2:53 min).
So now we know the effect of acetylcholine, we can predict the effect of both muscarinic receptor agonists and antagonists. Let’s start with the commonly used muscarinic receptor antagonists (anticholinergic drugs): atropine, hyoscine (butylbromide), tiotropium, ipratropium and oxybutynin. The anticholinergic drugs share structural similarities with acetylcholine so are able to interact with the receptor but 1) don’t activate the receptor and 2) block the action of acetylcholine at the M-Ach-R receptor. That makes them drug antagonists at the muscarinic receptor.
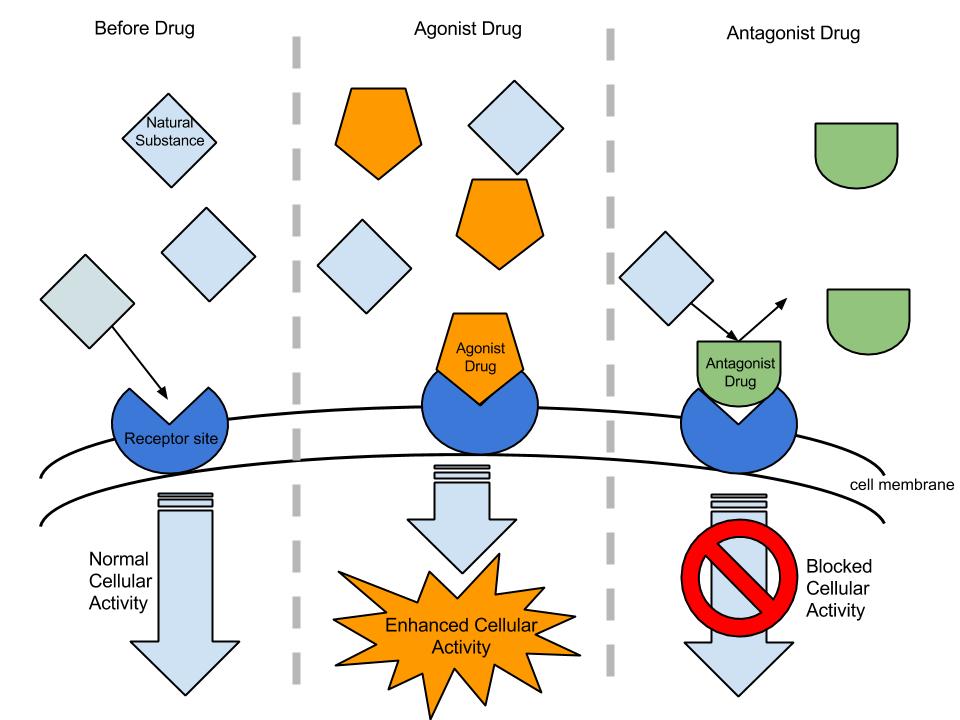
🔑 Concept check – drug agonists and antagonists
Agonist:
An agonist is a substance that binds to a receptor and activates it, mimicking the action of a naturally occurring substance in the body, such as a neurotransmitter or hormone. Agonists stimulate a physiological response by binding to and activating receptors. There are two types of agonists: full agonists and partial agonists. Full agonists bind to and fully activate the receptor, producing a maximum biological response, while partial agonists bind to and partially activate the receptor, resulting in a sub-maximal response compared to a full agonist.
For example, morphine is a full agonist at opioid receptors, producing analgesia, whereas buprenorphine is a partial agonist at opioid receptors, used in pain management and opioid addiction treatment.
Antagonist:
An antagonist is a substance that binds to a receptor but does not activate it. Instead, it blocks or dampens the action of agonists, including endogenous agonists, or prevents them from binding. Antagonists inhibit or block a physiological response by preventing agonists from binding to receptors. There are two types of antagonists: competitive antagonists and non-competitive antagonists. Competitive antagonists compete with agonists for the same binding site on the receptor, and their effects can be overcome by increasing the concentration of the agonist. Non-competitive antagonists bind to a different site on the receptor or irreversibly bind to the agonist site, and their effects cannot be easily reversed by increasing the concentration of the agonist.
For instance, naloxone is a competitive antagonist at opioid receptors, used to reverse opioid overdoses, while ketamine is a non-competitive antagonist at NMDA receptors, used as an anesthetic and for pain management. Another example where agonists are used therapeutically to block the effect of acetylcholine is ipratropium bromide. Ipratropium (you may know it as Atrovent) is an muscarinic antagonist (blocker) at the M3 receptor. It blocks the effect of acetylcholine reducing the normal effect of acetylcholine on the smooth muscle of the airway.
Antagonists are used therapeutically to block or reduce the effects of endogenous or exogenous agonists.
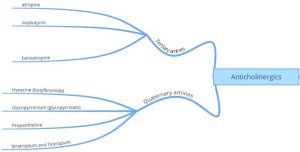
Anticholinergics – Muscarinic Receptor (M-AChR) Antagonists
Anticholinergics are often broken up structurally into tertiary amines – which are more lipid soluble molecules and quaternary amines – which are more water-soluble compounds. This is an important distinction as the two groups can differ in absorption, effect and side effect. The diagram below categorises the two groups of anticholinergic drugs via their structure. Let’s explore these drugs further.
📺 Watch the vodcast on categorisation of anticholinergic agents (3:16 min).
Atropine:
Atropine is a non-selective and competitive anticholinergic agent that blocks the effect of acetylcholine at muscarinic receptors both centrally and peripherally. It is used for 3 main purposes:
- Treat bradycardia
- Dry oral and respiratory secretions prior to induction of anaesthesia
- (sometimes, rarely) treat organophosphate poisoning
Atropines clinical effect on the heart is to block parasympathetic (cholinergic) innervation of myocardial tissue reducing bradycardia and to dry unwanted oral and respiratory secretions, as a typical example of the class, it displays all the common anticholinergic side effects:
- Eyes: Mydraisis, blurred vision, dry eyes
- GIT: dry mouth, constipation
- Urinary system: urinary retention
- CNS: (unusual) restlessness, agitation, disorientation
Because it is a tertiary ammonia compound, it is able to cross the blood brain barrier causing the unwanted CNS side effects.

📺 Watch the vodcast on atropine and its multi-organ effect (4:47 min).
Knowledge check
Ipratropium and tiotropium:
Ipratropium, and its longer acting partner – tiotropium – block the effects of acetylcholine at the muscarinic receptor in the smooth muscle of the airway. They are typically used to treat COPD (Chronic Obstructive Pulmonary Disease) and sometimes asthma.
Normally, the vagus nerve influences the patency of the bronchioles through the release of acetylcholine locally at the smooth muscle fibres that surround the bronchioles in the airways. The released acetylcholine interacts with the M3 receptor (remember, a G-coupled receptor) and causes the release of Phospholipase C which causes the release of inositol phosphate 3 (IP3). IP3 causes the release of calcium from the endoplasmic reticulum which directly results in the contraction of the smooth muscle leading to bronchoconstriction. Ipratropium and tiotropium (and the other anticholinergic drugs used to treat asthma and COPD) block the effect of acetylcholine at the M3 receptor thereby interrupting this process. So, the inhibition of acetylcholine at the M3 receptor on the smooth muscle of the bronchioles reduces bronchomotor tone, dilating the airway and relieving airway constriction. It also reduces respiratory secretions in the lungs. Then net effect is to relieve bronchoconstriction in patients suffering COPD.
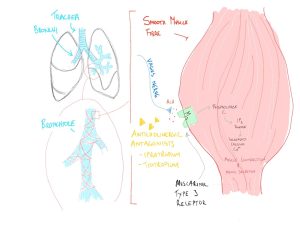
Tiotropium has a much longer duration of action at the receptor than ipratropium (~24 hours vs 6 hours) as tiotropium has a much higher affinity for the muscarinic receptor (around 10x the affinity) compared with ipratropium. This means it blocks the receptor for a much longer duration – increasing its effect.
📺 Watch the vodcast on ipratropium and tiotropium affect on the airways (5:13 min).
Knowledge check
Hyoscine butylbromide:
Like atropine, hyoscine butylbromide is a non-selective and competitive anticholinergic agent that blocks the effect of acetylcholine in the gut. It affects M1, M2 and M3 (important for stomach cramp) cholinergic receptors. It is commonly used to relieve cramps in the intestine and contraction of the bladder.

Unlike atropine, it is a quaternary ammonia compound meaning it is less lipid soluble. We see many of the peripheral side effects, but hyoscine butylbromide is less likely to cause the CNS side effects at normal doses. The common side effects of hyoscine butylbromide include:
- Dry mouth
- Constipation
- Blurred vision (blocks miosis causing mydraisis)
- Drowsiness (less common as it is poorly lipid soluble)
- Dizziness
- Increased heart rate (tachycardia)
- Difficulty in urination (urinary retention – see below).
If we think about the side effects – they are all associated with the blockade of acetylcholine at other organs (it is administered orally and so can affect the whole body).
Oxybutynin:
Oxybutynin is a M3 receptor antagonist used to treat urinary urge incontinence. Under normal circumstances, the release of acetylcholine from parasympathetic nerves and from non-neuronal cells within the urothelium (specialised epithelium lining of the lower urinary tract) cause contraction of the detrusor smooth muscle in the bladder. Oxybutynin acts to reduce bladder muscle contractility and increase bladder capacity. The intracellular mechanism that causes the contraction of the detrusor muscle is similar to that of ipratropium.
📺 Watch the vodcast on oxybutynin (1:35 min).
Pilocarpine – a muscarinic agonist:
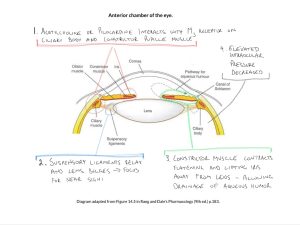
Muscarinic agonists such as carbachol (not currently used in Australia) and pilocarpine are agonists at the muscarinic receptor. When applied to the eye, acetylcholine-like stimulation of the M3 receptor causes contraction of the circular muscle that controls pupil size resulting in pupil constriction. It is therefore useful in the treatment of glaucoma where the contraction of the iris and constriction of the pupil increases outflow of aqueous humour, thus decreasing intraocular pressure.
The constrictor pupillae muscle runs circumferentially around the iris controlling the pupil diameter. The ciliary muscle is responsible for changing the focus (accommodation) of the lens. Both muscles contract in response to acetylcholine stimulation of the M3 receptor on the surface of these tissues. In the case of the ciliary muscle, it pull up and outward relaxing the suspensory ligaments that attach to the lens – causing the lens to bulge. This action changes the shape of the lens and accommodates for close focus.
The activation of the constrictor pupillae (muscle) of the iris constricts the iris with the effect of flattening out the folds of the iris increasing the gap near the canal of Schlemm. This facilitates outflow of aqueous humour and maintains healthy intraocular pressure. The figure below shows the anterior chamber of the eye and demonstrates the pathway for secretion and drainage of the aqueous humour.
Given this class of drug mimics the effect of stimulation of the parasympathetic nervous system, the potential side effects are fairly predictable: decreased heart rate and contractility, increased peristaltic activity in the gut and colicky pain, increased bladder and airway smooth muscle tone.
📺 Watch the vodcast on pilocarpine and its effect on the eye (4:52 min).
Summary
- The effects of anticholinergics and parasympathomimetic drugs are predictable if you understand the autonomic nervous system well.
- Kinetic differences between quaternary and tertiary ammonia compounds in a large way dictate the ability to transit the blood-brain barrier and exhibit CNS side effects
- Common uses of anticholinergics include:
- Bradycardia and heart block
- Drying oral and respiratory secretions prior to induction of anesthetics
- COPD and Asthma
- Urinary incontinence
- Single relevant parasympathomimetic (pilocarpine) used to treat glaucoma
- Understanding of parasympathetic nervous system is critical to understanding drug action and side effects of anticholinergic drugs (which are commonly used).
- Common anticholinergic side effects are shared with many drugs and include blurred vision, constipation, urinary retention, skin flushing (endothelium-dependent vasodilatation), dry eyes, mouth and skin.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
