1.4 Neuromuscular Blocking Drugs
John Smithson
Learning Outcomes
Be able to:
- Describe the typical uses for the neuromuscular blocking agents in practice
- Differentiate between the action of depolarizing and non-depolarizing neuromuscular blocking agents at the motor end plate
- Group the neuromuscular blocking agents by metabolic process for deactivation
- Describe the major risks and side effects associated with the two types of neuromuscular blocking agents
There are two types of neuromuscular blocking agents
Neuromuscular blocking agents are used to cause muscle paralysis during surgery. When we consider neuromuscular blocking agents, we have two basic subdivisions: the depolarizing neuromuscular blocking agents and the non-depolarising neuromuscular blocking agents.
The two main groups work in paradoxical ways to achieve the same outcome. The neuromuscular blocking agents are organized by sub-group in the Table 1.4.1 below:
| Non-depolarising | Depolarising |
| Atracurium | Suxamethonium |
| Cisatracurium | |
| Mivacurium | (Acetylcholine (Ach) normal neurotransmitter) |
| Pancuronium | |
| Rocuronium | |
| Vecuronium |
Note the suffix of the neuromuscular blocking agents: either ‘curium’ or ‘onium’. That may help identification later.
Muscle contraction is initiated by the release of acetylcholine by the somatic neuron at the motor end plate of the sarcolemma
The neuromuscular blocking agents act at the neuromuscular junction – the intersection of the nerve and muscle, or to be precise, it innervates the sarcolemma – the sheath of muscle fibres that surround the individual muscle fibres which passes that signal to the individual muscle fibres. The efferent nerve (part of the somatic (motor) division of the peripheral nervous system) releases acetylcholine into the synaptic cleft, which interacts with post-synaptic nicotinic acetylcholine (ACh) receptors (which you will remember are ligand gated ion channels) at the motor end plate. In response to the attachment of ACh, the ion channel opens, allowing sodium (Na+) to enter the cell causing the generation of an action potential in the sarcolemma. This is passed onto the individual muscle fibres surrounded by the sarcolemma and causes muscle contraction.
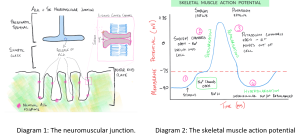
Revision: The skeletal muscle action potential. If you need to brush up on the skeletal muscle action potential or need a more detailed explanation of Diagram 2, watch this brief vodcast.
📺 Watch the vodcast on Neuromuscular blocking agents overview (3:44 min).
Suxamethonium – the single depolarizing neuromuscular blocking agent
The only depolarising nicotinic acetylcholine receptor (nAChR) agonist is suxamethonium (also sometimes known as succinylcholine) sometimes abbreviated to ‘sux’. Suxamethonium is often used during the induction of anesthesia where very brief muscle paralysis is required (for example, during intubation prior to surgery). Suxamethonium interacts with the (nAChR) nicotinic acetylcholine receptor as an agonist and mimics the effect of acetylcholine at the receptor. Interaction of suxamethonium at the receptor causes an influx of sodium into the sarcolemma of the muscle. This initially causes was known as the phenomenon of fasciculation – a cycle of involuntary small local muscle contractions and relaxation which is often visible under the skin. The following video shows muscle fasciculations in potassium channelopathy. It is a useful demonstration of the phenomenon of fasciculation seen with suxamethonium.
📺 Watch video: Muscle fasciculations in potassium channelopathy
Normally, after activation of the nAChR, ACh dissociates from the receptor and is hydrolyzed by AChE (inactivating the ACh). The sarcolemma is then able to repolarize in preparation for the next release of ACh. The duration of the effect of AChE is incredibly short – in the range of milliseconds. In contrast, suxamethonium has a much longer duration of effect, it is not hydrolyzed by AChE and therefore maintains the membrane potential of the sarcolemma above threshold – preventing repolarization and preventing activation by a subsequent signal. The result is a 3-5 minute paralysis of (mainly) skeletal, abdominal and respiratory muscles. As the duration of the effect of suxamethonium is extended it is available to interact with the nAChR and thus prevents repolarization (see phase 3 in the skeletal muscle action potential diagram). This means the sarcolemma is not responsive to subsequent exposure to acetylcholine for the duration that pharmacologically useful levels of suxamethonium are present at the neuromuscular junction. The result is temporary paralysis of the muscle.
Suxamethonium
- Rapid onset and short duration nAChR agonist – resulting in muscle paralysis.
- Mimics the effect of acetylcholine at the nAChR at the motor end plate – because it has extended action at the motor end plate, it depolarizes then because of its extended action prevents repolarization of the muscle fibres
- Results in short term paralysis of skeletal, abdominal and respiratory muscles. Patient (usually) spontaneously recovers from paralysis within 3-5 minutes.
- Major side effects include muscle pain (fasciculations), hyperkaliemia, bradycardia, raised intraocular pressure. In rare cases, patients can experience a syndrome called malignant hyperthermia. Some patients have a genetic mutation that results in much lower expression of the enzyme plasma pseudo cholinesterase (aka plasma cholinesterase). This extends the duration of action in these patients to 2-3 hours.
📺 Watch the vodcast on Suxamethonium (8:41 min).
The rest of the anaesthetic muscle relaxants are non-depolarising neuromuscular blocking agents
The non-depolarising neuromuscular blocking agents include atracurium, cisatracurium, mivacurium, pancuronium, rocuronium and vecuronium. These agents act as antagonists at the nAChR preventing ACh interacting with the nAChR. The result is similar to suxamethonium – muscle paralysis although there are two important differences – the onset of action is typically slightly longer than suxamethonium and the duration of action is much longer – between 15 minutes and 2 hours. Compare this with suxamethonium which is typically 3-5 minutes.
The extended duration of the non-depolarising neuromuscular blocking agents is particularly useful where prolonged paralysis of muscle is required (for example, during orthopaedic or abdominal surgery). There are a range of typically seen side effects with the use of the non-depolarising blocking agents. The two most common ones are the release of histamine (common with atracurium, mivacurium & rocuronium) and tachycardia (rocuronium & pancuronium). The most commonly used non-depolarising neuromuscular blocking agent is probably vecuronium. It has no effect on the release of histamine nor does it affect heart rate. Rocuronium is typically used where a rapid onset of paralysis is required but suxamethonium is contraindicated.
Reversal of the non-depolarising neuromuscular blocking agents
The non-depolarising neuromuscular blocking agents can be reversed by the application of neostigmine (an acetylcholinesterase inhibitor) or sugammadex (for rocuronium and vecuronium only). Neostigmine is able to reverse paralysis caused by the non-depolarising neuromuscular blocking agents as it reduces the breakdown of acetylcholine at the motor end plate. This makes more ACh available and because the non-depolarising neuromuscular blocking agents are competitive antagonists, acetylcholine can outcompete the non-depolarising neuromuscular blocking agents at the nicotinic receptor. However, the reverse is true. Where very high doses of neuromuscular blocking agents are given, neostigmine can be ineffective in reversing paralysis. It is important to note neostigmine not only increases concentrations of Ach at the motor end plate but also at muscarinic receptors – leading to unwanted effects of bronchospasm, increased salivation and other secretions, bradycardia and increased GI motility. To offset the increased muscarinic activation, atropine or glycopyrrolate is often administered with neostigmine.
Sugammadex provides a complete and rapid reversal of paralysis caused by rocuronium and vecuronium. Where neostigmine has an indirect effect in the reversal of paralysis – sugammadex binds with free rocuronium or vecuronium making them unavailable for interaction with the nicotinic receptor. Sugammadex has no effect on muscarinic receptors and therefore has none of the undesired muscarinic effects seen with neostigmine.
📺 Watch the vodcast on Non-depolarising muscle relaxants (6:49min).
Summary
- Two types of neuromuscular blocking agents – depolarizing and non-depolarizing
- Both are used to paralyze muscles during long-term intubation or surgery
- Suxamethonium (depolarizing agent) has rapid onset and short duration
- Mimics the effect of acetylcholine at the nAChR at the motor end plate
- Metabolised by plasma cholinesterase
- Kinetics independent of renal and hepatic function
- Depolarising NM blocking agents have slower onset and much longer duration of action
- Atracurium, cisatracurium, mivacurium, pancuronium, rocuronium, vecuronium
- Block the action of Ach at the nAChR
- Metabolized by a range of processes
- The different agents differ
- Onset of action
- Duration of action
- Mechanism of metabolism and excretion
- Side effects
- Neuromuscular blocking agents do not cause sedation – only paralysis.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
