11.1 Antipsychotics
Schizophrenia
Introduction
Schizophrenia is quite a large topic, and one that is important for us as pharmacists to understand.
Schizophrenia is a mental illness that causes someone to have a perception of reality that is different to what everyone else around them knows to be objectively real. These different perceptions affect the person’s thoughts, behaviours, and ability to function at work and school. It also affects their ability to develop and sustain relationships with others.
Other characteristic features of schizophrenia include disturbances in speech, cognition, volition (willpower), and emotion. We discuss these in more detail in the lecture.
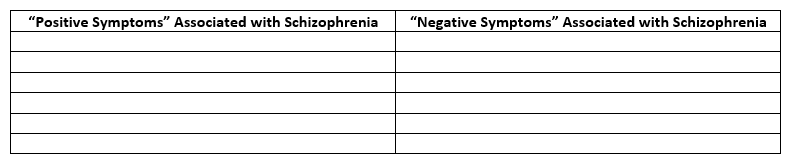
Watch the lecture recording (part 1), and then complete the table below. Use it as a study tool.
Schizoaffective disorder (SAD) differs from schizophrenia (SCZ) in that SAD has the core symptoms of SCZ as well as prominent symptoms of a mood disorder (e.g. episodes of elevated mood and/or episodes of depression). The management of SAD generally reflects the management of bipolar disorder.
It is currently thought that schizophrenia is caused by a combination of genetic and environmental factors.
Illicit drug use (particularly cannabis use) is thought to significantly increase the risk of a predisposed individual experiencing their first signs and symptoms of schizophrenia.
However, other factors such as an extremely stressful event in the person’s life can also precipitate the onset of symptoms in a person who is vulnerable to developing schizophrenia.
It is important to understand that there are many misconceptions surrounding schizophrenia.
- You must know that schizophrenic patients do not suffer from ‘split’ or multiple personalities. This would be a symptom of a spectrum of dissociative disorders.
- The vast majority of patients with stable schizophrenia are not violent or dangerous. In reality, they are sometimes at a higher risk of harm to themselves. We must understand this in order to help the patient by advocating for the most appropriate treatment option(s).
Watch the following video for one patient’s story and personal perspective of schizophrenia.
https://www.youtube.com/watch?v=BTHtqi4F1TM&feature=youtu.be
Click on the following link to learn more about a different patient’s story.
https://healthtalkaustralia.org/supported-decision-making/peoples-profiles/evan/
Pathogenesis of schizophrenia
Schizophrenia is the main psychotic disorder, which is considered to be a neurodevelopmental disorder. The pathophysiology of schizophrenia is complex and not completely understood but may involve both genetic (mutations in a number of genes have been described) and environmental factors (neuronal injuries in utero, aberrations in neurodevelopment, abuse of psychoactive substances…). Symptoms displayed by schizophrenia sufferers include delusions, hallucinations and irrationality (collectively known as positive symptoms); emotional flatness and socially withdrawn (negative symptoms). The sufferers also have poor memory and learning skills (cognitive dysfunction). These symptoms usually manifested in persons aged 15-25 years old, therefore schizophrenia is a very debilitating psychiatric disorder affecting young adults. At this stage, the brain is still developing and thus the link between schizophrenia and abnormal brain development. Abuse of psychoactive agents (e.g. cannabis – use during teenage years or exposure to in utero) has been strongly associated with an increased risk of developing schizophrenia.
Positive symptoms have been associated with excess dopamine neurotransmission in the mesolimbic pathway and negative symptoms with reduced dopamine neurotransmission in the mesocortical pathway.
Dopamine Theory and Schizophrenia
This theory proposes that there is hyperactivity of dopaminergic neurons in the mesolimbic tract, and hypoactivity of dopaminergic neurons in the frontal mesocortical tract in schizophrenia.
- Medications that block dopamine from binding to the D2 receptor –> fewer positive (psychotic) symptoms
- Medications that increase dopamine levels –> positive (psychotic) symptom flares
- Decreased dopamine release in the frontal cortex (mesocortical tract) –> negative symptoms of schizophrenia
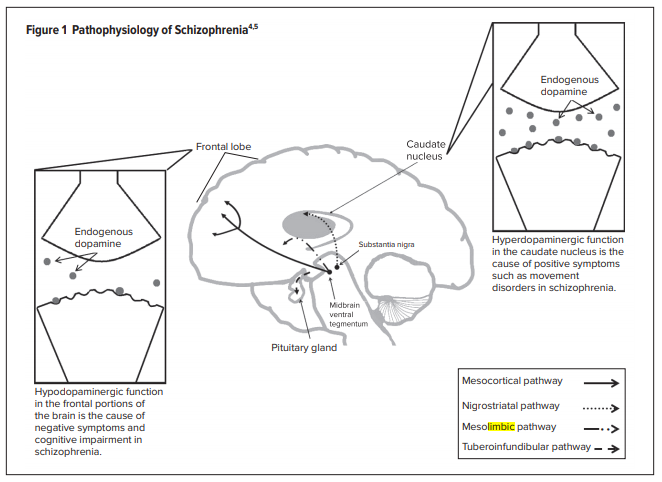
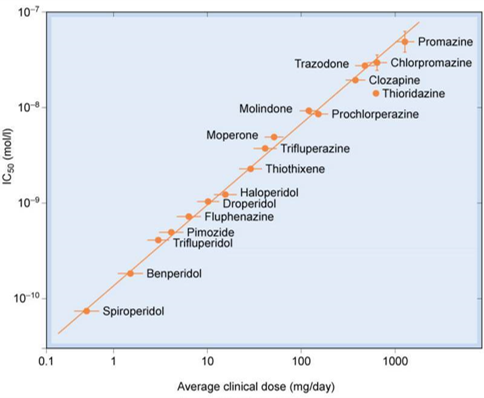
This is based on pharmacological evidence that therapeutic agents for the treatment of schizophrenia are mainly dopamine D2 receptor antagonists (neuroleptics = high affinity D2 receptor antagonists), and that D2 receptor agonists and those which increase brain dopamine level can cause schizophrenia-like psychosis. In addition, the binding affinities of a variety of D2 receptor antagonists correlate with their clinical efficacies (higher affinity = higher clinical efficacy = lower dosage required).
This theory nevertheless does not completely address some anomalies:
- Delay in the manifestation of clinical benefit (i.e. requires weeks of drug treatment).
- Some patients are not responsive to treatment with neuroleptics (treatment resistance).
- High affinity D2 receptor antagonists are only effective for alleviating positive symptoms.
- Newer atypical agents have low affinity for D2 receptors.
- Chronic treatment with antipsychotics increases D2 receptor expression (a contradiction in relation to clinical efficacy, i.e. more receptors = more stimulation?!?) and thus the increased risk of psychosis when ceasing medication abruptly.
Other theories
The NMDA theory
The glutamate NMDA receptor antagonists (ketamine and phencyclidine – “angel dust”) are hallucinogenic. Glutamate theory is further supported by studies showing the reductions of glutamate concentrations and glutamate receptor densities in post-mortem schizophrenic brains, and a recent publication showing anomalies in the genes involved in the glutamatergic neurotransmission.
- Glutamate is a major excitatory neurotransmitter in the brain
- This theory suggests that there is reduced glutamatergic neurotransmission in patients with schizophrenia
- NMDA receptor inactivity in schizophrenia –> enhanced activity of dopaminergic neurons in the mesolimbic tract –> positive symptoms of schizophrenia
- NMDA receptor inactivity in schizophrenia –> reduced activity of dopaminergic neurons in the mesocortical tract –> negative symptoms of schizophrenia
Serotonin theory
This is also based on the observations that 5-HT2 receptor agonists (psilocybin from “magic mushroom” and mescaline – a psychedelic alkaloid from cactus) The involvement of 5-HT is further supported by:
- High affinity 5-HT2 receptor antagonism in atypical antipsychotics are effective in alleviating both positive and negative symptoms.
- Agents with 5-HT2 antagonism are useful for those who do not benefit from the older high affinity D2 receptor antagonists, and they produce less adverse effects attributable to D2 receptor antagonism (e.g. extrapyrimidal side effects – EPS and hyperprolactinaemia).
👁️🎧 Listen & Watch part 1 of Antipsychotic Lecture (20 minutes)
Pharmacology of Antipsychotics
The pathophysiology of schizophrenia can be used to understand the pharmacology of our available treatment options. Antipsychotic drugs alter neurotransmitter levels at these different CNS pathways.
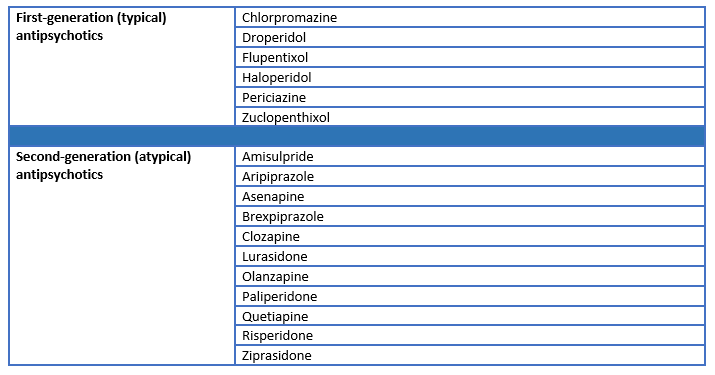
“Typical” antipsychotics – Neuroleptics (haloperidol, chlorpromazine)
These are high affinity D2 receptor antagonists effective for alleviating positive symptoms only. They are effective in approximately 70% of schizophrenia sufferers. Adverse effects include dysphoria, sedation, EPS (involuntary movement: acute dystonias – occurs at the beginning of treatment due to blockade of D2 receptors in nigrostriatal pathway and reversible with treatment withdrawal; tardive dyskinesia – develops after chronic drug treatment, symptoms worsen with treatment withdrawal), and hyperprolactinaemia. They also have antagonist activity at α1-adrenoceptors (producing postural hypotension, impotence…), muscarinic receptors (dry mouth, dry eyes and others), H1-receptors (sedation) and 5-HT2 receptors (weight gain – but less than atypical agents). They are also more likely to cause Neuroleptic Malignant Syndrome (NMS).
“Atypical” antipsychotics or Second-Generation Antipsychotics (SGAs)
Clozapine (not first choice due to serious adverse effects)
This agent is a high affinity D4 receptor antagonist and has low affinity for D2 receptors. It also has antagonist activity at α1, muscarinic, H1 and 5-HT2 receptors. It is effective for both positive and negative symptoms and for those not responding to typical antipsychotics. The clinical use of clozapine is limited (reserved for those not benefit from other agents) as it can cause agranulocytosis (low white blood cell count). Therefore, a complete blood count (WBC) is performed before the treatment and frequently during the treatment. This adverse event is reversible with the withdrawal of clozapine.
Others:
- Risperidone – which has high affinity for 5-HT2 receptors.
- Olanzapine – also has high affinity for 5-HT2 receptors (5-HT2A>H1>D4>D2>α1>D1).
- Aripiprazole – D2=5-HT2A>D4>α1=H1 >>D1.
- Aripiprazole is a partial agonist at D2 and 5-HT1A receptors (studies has shown that stimulation of 5-HT1A receptors can increase dopamine release in the prefrontal cortex, thus correcting for the lack of dopamine neurotransmission in mesocortical pathway – alleviating negative symptoms). As a D2 receptor partial agonist, it can behave as an antagonist in brain areas with high dopamine neurotransmission (mesolimbic – it competes with the endogenous full agonist i.e. dopamine for binding sites, thus reducing receptor activation) or as an agonist in areas with low dopamine neurotransmission (mesocortical – binds D2 and stimulates the receptor). It also displays antagonism at α1, H1, 5-HT2 receptors, and has lower incidence of adverse effects compared to typical antipsychotics.
In general, 5-HT2 receptor antagonism = weight gain, a problem with the use of some atypical agents such as olanzapine and clozapine, which can lead to the development of diabetes.
Adverse effects – a comparison
In general, common side effects of antipsychotics include:
- Extrapyramidal side effects (EPSEs)
- Tardive dyskinesias
- Neuroleptic malignant syndrome (NMS)
- Metabolic disturbances and weight gain
- Endocrine disturbances
- Sedation
- Hypotension
- Sexual dysfunction
- Anticholinergic effects
However, due to their different receptor binding properties, different antipsychotics have different comparative adverse effect profiles.
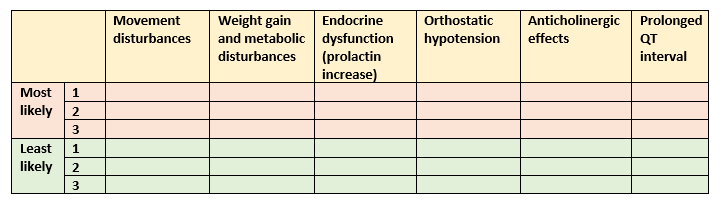
Watch the lecture recording (part 2) and then complete the table below. Use it as a study tool to be able to list the antipsychotics that are most- and least likely to cause the following adverse effects.
👁️🎧 Listen & Watch part 2 of Antipsychotic Lecture (20 minutes)
Interesting Update
Did you hear about Clobenfy? Approved on 26 September 2024 by FDA for the treatment of Schizophrenia.
Clobenfy – a combination of xanomeline and trospium chloride capsules targeting cholinergic receptors (NOT dopamine receptors!)
Read more from:
Lecture Material:
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
