12.4 Neurological Drugs – Migraine
Migraine
Migraine is a neurological disorder characterized by recurrent, moderate to severe headaches, often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light or sound (photophobia and phonophobia). The pain typically affects one side of the head (unilateral) and is throbbing or pulsating in nature. A migraine attack can last from 4 to 72 hours and may include premonitory symptoms (prodrome) and, in some cases, visual or sensory disturbances (aura) before the headache phase. Migraines are more common in women than men, and while the exact cause is unknown, genetic, environmental, and hormonal factors play a role.
Pathophysiology of Migraine
The pathophysiology of migraine is not fully understood, complex and multifactorial, involving both central and peripheral mechanisms. Key theories/hypotheses include:
The vascular hypothesis
- Probably the simplest of the hypotheses regarding the pathophysiology of migraine.
- Considers that the migraines are caused by the dilation of cranial blood vessels.
- Based on observations that vasoconstrictors can improve the symptoms of migraines, and that (conversely) vasodilators can bring on migraines.
- However, it is generally accepted now that this hypothesis is not true. Instead, it has been shown that specific receptor site activation is more important than simply generalised vasodilation.
Aura – “the aura is the primary initiator of the migraine attack”
- States that cortical spreading depolarisation (previously known as cortical spreading depression) is the physiological explanation for the signs and symptoms of an aura, and that this cortical spreading depolarisation is also what activates pain signalling pathways.
- Arguments against this theory claim that aura is not necessary or sufficient for the headache. Specifically, they claim that:
- Most migraines are not actually associated with an aura at all
- Migraine aura can occur without headache
Trigeminal Nerve Activation – neuropeptides as mediators of migraines
- Considers serum concentrations of calcitonin gene-related peptide (CGRP) and argues that this CGRP is both a mediator of migraines and an important therapeutic target.
- Notes that:
- Serum concentrations increase during a migraine attack
- Concentration normalises during treatment with commonly used drugs (e.g. triptans)
5-HT – “migraine is a syndrome of chronically low serotonin (5HT) levels in the brain”
- Resembles the vascular hypothesis, but does focus on vasoconstriction mediated by serotonin (i.e., 5HT) receptors specifically.
- Serotonin binds to postsynaptic 5HT1 receptors –> vasoconstriction of the nerve endings and blood vessels —> reduced pain
- This hypothesis is supported by the fact that drugs commonly used for migraines (e.g. triptans) are agonists at the 5HT1 receptor.
Treatment Options
The following table may prove to be the start of a useful study aid. However, you should first seek to expand on these points significantly.
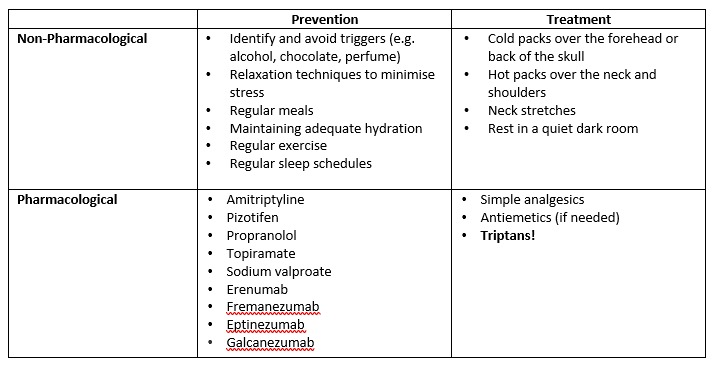
The management of migraine focuses on both acute (abortive) and preventive (prophylactic) treatments. Acute treatments are aimed at stopping an ongoing attack, while preventive treatments aim to reduce the frequency and severity of attacks.
- Acute (Abortive) Treatment: These treatments are most effective when taken early in the course of a migraine attack. They include:
-
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Drugs like ibuprofen and aspirin are first-line treatments for mild to moderate migraines.
-
- Triptans: Sumatriptan, rizatriptan, naratriptan and zolmitriptan are commonly used for moderate to severe migraine attacks. Triptans are serotonin (5-HT1B/1D) receptor agonists. Their primary action is vasoconstriction of dilated cranial blood vessels, which relieves headache. They also inhibit the release of CGRP and other neuropeptides that contribute to neurogenic inflammation.
All except naratriptan have recently been down scheduled to S3 pharmacist only products, in certain strengths and quantities as per the SUSMP.
Pharmacist-only OTC provision of triptans is only suitable if all of the following criteria are met:
- Migraine has been formally diagnosed by their medical practitioner previously
- Symptoms are consistent with migraine (generally)
- Symptoms are consistent with the patient’s previous migraine experience(s), i.e., there has been no change in the patient’s headache symptoms
- Migraine does not persist or interfere with daily life despite treatment
- The patient is not experiencing increased frequency of migraine attacks or requiring increasing frequency of triptan use
- The patient is not needing to use triptans on more than 10 days per month
- The patient has no other precautions or contraindications to triptan treatment
Triptans are most effective when the headache is just beginning to develop. If taken early, triptans are effective in about two-thirds of patients, with symptom relief usually expected to begin within about half an hour to an hour of oral administration. Triptans also improve symptoms associated with migraine, such as nausea, vomiting, photophobia and phonophobia.
Some patients might have recurrence of their migraine headache. In that case, one repeat of the triptan dose might be indicated. However, if no relief was experienced after the first dose, a repeat dose is not recommended. The interval between the first and second triptan dose depends on the specific triptan (refer to your AMH or product information).
When prescribing a triptan, it’s also important to consider the available formulations. For example, we’ve got wafers or subcutaneous dosage forms that might be preferred for patients with nausea.
-
- Ergotamines: Ergotamine and dihydroergotamine are older migraine medications that also cause vasoconstriction and are used in patients who do not respond to triptans.
-
- Antiemetics: Metoclopramide or prochlorperazine may be used to control nausea and vomiting associated with migraine.
- Preventive (Prophylactic) Treatment: Prophylactic treatments are prescribed for individuals with frequent or debilitating migraines. Common options include:
-
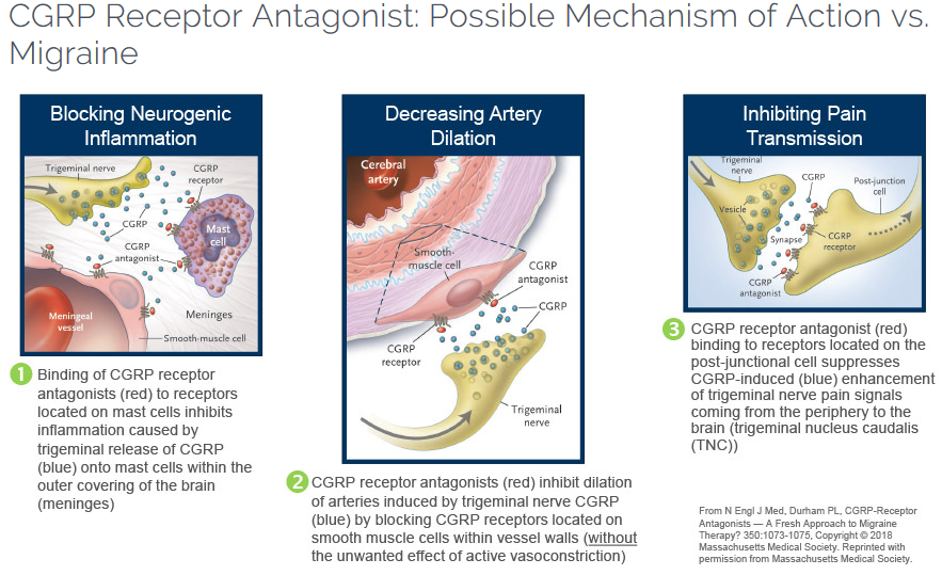
- CGRP Inhibitors: Monoclonal antibodies targeting calcitonin gene-related peptide (CGRP) or its receptor (e.g., erenumab, fremanezumab, galcanezumab) are a newer class of preventive treatments that inhibit CGRP’s effects in migraine pathophysiology. CGRP plays a central role in migraine pathophysiology by promoting vasodilation and inflammation. The sensory trigeminal nerves release CGRP which contributes to pain transmission, neurogenic inflammation, intracranial artery dilation. CGRP inhibitors block the action of this peptide, either by binding directly to CGRP or by blocking its receptor, thus reducing the frequency and severity of migraines. CGRP inhibitors can be self-administered as subcutaneous injections. Some common adverse effects include pain and erythema at injection site, dizziness; rare hypersensitivity reactions.
-
- Botulinum Toxin (onabotulinumtoxinA)
Botulinum toxins are very potent neurotoxins, which are injected intramuscularly. The toxin causes paralysis by blocking presynaptic release of acetylcholine (i.e., blocks exocytosis of Ach) at the neuromuscular junction, with reversible chemical denervation of the muscle fibre, thereby inducing partial paralysis and atrophy. These toxins have many indications like cervical dystonia, blepharospasm, hemifacial spasm, urinary incontinence etc
Botulinum toxin named can be indicated as prophylaxis of chronic migraine – some trials showed that botulinum toxin was slightly more effective than placebo in preventing headache in patients with headache on >15 days/month. However, other trials showed it was ineffective in patients with headache on <15 days/month.
Some adverse effects include injection site pain, neck pain, muscle weakness, eyelid ptosis, paraesthesia.
-
- Beta-Blockers: Drugs like propranolol and metoprolol help reduce the frequency of migraines by stabilizing blood vessels and influencing neurovascular mechanisms.
-
- Antiepileptics: Topiramate and valproate have been shown to reduce migraine frequency by modulating neuronal excitability.
-
- Antidepressants: Tricyclic antidepressants (e.g., amitriptyline) and serotonin-norepinephrine reuptake inhibitors (e.g., venlafaxine) are sometimes used for their effects on pain modulation.
Migraine Lecture
 Watch the following lecture on Migraine and it’s treatment (16 minutes)
Watch the following lecture on Migraine and it’s treatment (16 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
