2.16 Treatment for Elevated Cholesterol is now based on Patients AusCVD Risk
John Smithson
Be able to:
- determine whether to treat elevated cholesterol levels in patients based on their individual cardiovascular risk, and identify the appropriate cholesterol-lowering targets for high, intermediate, and low-risk patients.
- assess cardiovascular risk using the AusCVDRisk tool, which includes factors such as age, gender, smoking status, cholesterol ratio, systolic blood pressure, diabetes, medication use, history of atrial fibrillation, and socioeconomic status, and apply intensive lifestyle advice and pharmacotherapy accordingly.
Case Study: Alf Landerman
Alf is a 55-year-old Indigenous man well known to you who presents for a well man check-up. Alf works for the Cairns Airport as an air traffic controller. He lives with his wife Cynthia and one child.
Patient: Alf Landerman, 55-year-old Indigenous male
Medical History:
- Quit smoking 5 years ago
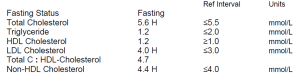
- Systolic blood pressure: 145 mmHg
- Total cholesterol: 5.5 mmol/L
- HDL cholesterol: 1.2 mmol/L
- Currently takes ramipril 10mg OD in the morning for elevated blood pressure
- No history of atrial fibrillation (AF), diabetes, kidney disease, or familial hypercholesterolemia
Location: Cairns, QLD 4870

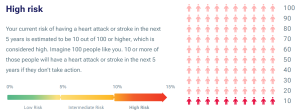
Alf has a intermediate risk of CVD in the next 5 years, but as he is an Indigenous man, his risk has been elevated by one category to high risk.
…. So the question is – do we treat Alf’s elevated cholesterol levels and if so, what are our agreed cholesterol lowering targets and how do we reduce his cholesterol and monitor progress?
Let’s leave the how and monitoring for a later section. Let’s focus on the ‘do we treat’ and ‘what are the targets’ part of the problem.
The approach to cholesterol lowering is based on the individual’s CV risk
The risk of the individual patient developing cardiovascular disease in the next 5 years directs the therapeutic approach to the management of diabetes. Adults without established cardiovascular disease who are 45 years or older (or 30 years or older if Aboriginal and Torres Strait Islander) should have their CV risk calculated.
Patients with established cardiovascular disease do not need their risk calculated as they are at high risk by virtue of having established CV disease. These people will benefit from an absolute risk reduction strategy as they will be in the high risk (or very high) category. Remember that we are providing secondary prevention in these patients and the associated treatment targets are often lower (more aggressive treatment) compared to primary prevention.
Back to primary prevention – CV risk in Australia is calculated using the AusCVDRisk tool. This tool considers:
- Age
- Gender
- Smoking status
- Cholesterol ratio
- Systolic blood pressure
- Diabetes
- Use of medication
- History of atrial fibrillation
- Socioeconomic status.
Presented as a 5-year risk as a percentage. It calculates the risk and stratifies the risk into 3 categories: high risk, intermediate risk and low risk.
Patients with a high risk of CV disease in the next 5 years
Based on Alf’s high risk of cardiovascular risk in the next 5 years (let’s assume 10%), he is at high risk of developing cardiovascular disease in the next 5 years. Patients in the high risk group should be provided intensive lifestyle advice aimed at lowering cholesterol and blood pressure as well as pharmacotherapy for cholesterol and blood pressure.
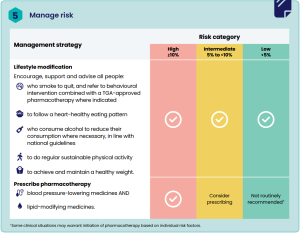
Patients with an intermediate risk of CV disease in the next 5 years
Patients with an intermediate risk should be considered for reclassification as either low or high risk. If after consideration they remain at intermediate risk, they should be provided with intensive lifestyle advice and considered for pharmacotherapy considering overall CV risk, patient preferences and benefits and risks.
Patients with a low risk of CV disease in the next 5 years
Patients with elevated cholesterol with a low absolute risk of developing cardiovascular disease in the next 5 years should be provided lifestyle advice to reduce lipid levels naturally and repeat the lipids every 5 years. Lifestyle modifications known to reduce cholesterol include:
- Weight reduction – a 2.3kg loss in body weight can double the lipid lowering effect of dietary modification alone, it also reduces the rate of production of VLDL (and thus LDL), decrease triglyceride levels and slightly increase HDL cholesterol. The target BMI should be > 25.
- Dietary modification – intensive dietary intervention can decrease total cholesterol and LDL cholesterol by up to 30%. The general aim of dietary modification is to decrease the intake of saturated fat and cholesterol containing foods and increase the proportion of polyunsaturated and monounsaturated fat, consume moderate amounts of lean meats, fish, eggs, tofu, nuts and seeds, dairy such as milk, yoghurt and cheese, moderate amounts of fruit and a larger proportion of vegetables, legumes and beans and larger proportion of grains and cereals. Dietary modification can also enhance the effects of lipid lowering drugs. Visit the following link to review the Australian Guide to Healthy Eating.
- Alcohol reduction or elimination – there is a linear relationship between serum triglyceride levels and increased alcohol consumption. The effect of alcohol upon HDL cholesterol is less certain with some patients experiencing an increase in HDL-C and some a reduction in HDL-C.
- Physical exercise – exercise elevates HDL-C levels
- Smoking cessation – smoking increases plasma cholesterol levels with an association between each cigarette and a subsequent increase in plasma cholesterol levels.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
