2.18 Introduction to Drug Use when Managing Dyslipidemia
John Smithson
Be able to:
- Understand the basic mechanisms by which the four main drug classes (statins, fibrates, ezetimibe, and PCSK9 inhibitors) reduce plasma cholesterol levels and their specific sites of action.
- Identify less commonly used pharmacological approaches for cholesterol reduction, including fish oil, bile acid binding resins, and nicotinic acid, and understand their roles and limitations.
- Recognize the significance of lifestyle changes in managing dyslipidaemia, including the impact of dietary modification, weight loss, smoking cessation, alcohol reduction, and physical activity on cholesterol levels.
- Develop a comprehensive understanding of the primary targets and strategies in lipid-modifying therapy, emphasizing the role of LDL-C reduction and the sequential use of statins, ezetimibe, PCSK9 inhibitors, and fibrates to achieve therapeutic goals.
There are 4 main drug classes that can reduce plasma cholesterol levels:
- Statins – reduce how much cholesterol is made in the liver.
- Fibrates – reduce triglyceride transport to the liver.
- Ezetimibe – a brush border enzyme inhibitor reduces how much cholesterol is absorbed from the diet via the small intestine.
- PSCK9 inhibitors – increase the amount of cholesterol removed from the blood by the liver.
Three less commonly used pharmacological approaches which are rarely used include:
- Fish oil
- Bile acid binding resins such as sequestrants and
- nicotinic acid.
The last 3 are either rarely (sooooo rarely as to say almost never) used (bile acid binding resins and nicotinic acid) or used only as a supplement (fish oil). Let’s get the pharmacology of these 3 drugs out of the way early. They are less important so your understanding of them can be suitably shallow.
Common drug classes used to lower blood cholesterol and how they are used
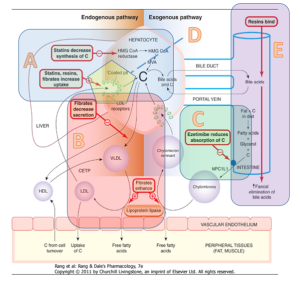
The figure below shows the site of action of the 4 most common classes of drug action for cholesterol reduction:
- Statins decrease the body’s internal production of cholesterol. (Refer to A in the figure below).
- Fibrates increase lipolysis in the tissues (Refer to B in the figure below).
- Ezetimibe inhibits brush border enzymes reducing the absorption of cholesterol (Refer to C in the figure below).
- PSCK-9 inhibitors decrease the breakdown of LDL receptors in the liver increasing scavenging of cholesterol from the blood.
Note that the 4 main drug classes, as they work in different ways, a combination of 2 or more of these medications can lower cholesterol more than one medicine alone.
Other drugs that lower cholesterol
- Bile acid binding resins bind to bile in the small intestine reducing its reabsorption. This increases the clearance of cholesterol and reduces recirculation of bile acids. Because less bile is being reabsorbed, the liver scavenges cholesterol from the plasma to make more bile. This lowers serum cholesterol levels. Bile acid binding resins can reduce LDL-C by 15-25% but may also increase triglycerides. The mechanism of action of the bile acid binding resins is shown at point E in the figure above.
- Nicotinic acid is rarely used and is thought to act by reducing VLDL and LDL production.
- Fish oil suppresses hepatic triglyceride and VLDL production. Fish oil is mainly used to treat hypertriglyceridaemia.
LDL-C Management in Lipid-Modifying Therapy – Pharmacotherapy
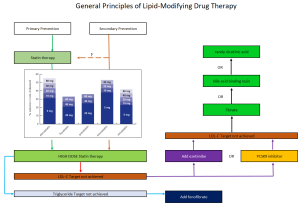
LDL-C (low-density lipoprotein cholesterol) is the primary target of lipid-modifying therapy due to its strong relationship with cardiovascular events. There is a continuous correlation between the extent of LDL-C reduction and the decrease in cardiovascular events, making it crucial to lower LDL-C levels. Although achieving target lipid levels can be challenging, any progress towards the target is beneficial.
Statins are typically the first-line treatment in addition to non-drug therapies, such as lifestyle changes. Potent statins like atorvastatin or rosuvastatin are commonly used. A low to mid-range dose of a statin can be initiated. For patients assessed at high risk or higher for cardiovascular disease (CVD), a high dose of a potent statin may be started.
The effect of the statin is evaluated after six weeks. If the target range is not achieved, ezetimibe or a PCSK9 inhibitor can be added. Ezetimibe is typically the next choice due to its efficacy and cost-effectiveness. If triglyceride levels are not within the target range, adding a fibrate may be considered.
📺 Watch video: Approach to drug management – hyperlipidaemia. (6:54 min)
Summary
- Hyperlipidemia and dyslipidemia are sometimes used interchangeably but this is technically incorrect. They both indicate a derangement of lipid profile. Dyslipidemia is a broader term accepted to cover elevations in plasma cholesterol
- Cholesterol is a major risk factor for CVD and stroke
- Cholesterol comes from two sources – the exogenous pathway absorbed from diet and the endogenous pathway – cholesterol produced by the liver
- There are three major lipids reported in lipid studies – LDL-C which is also known as bad cholesterol. It is responsible for transporting cholesterol to the peripheral tissues. HDL-C which is also known as good cholesterol which is responsible for transporting excess cholesterol from the peripheries to the liver for use or elimination and triglycerides – excess energy typically stored in adipose tissue. It is associated with liver dysfunction and pancreatitis.
- Approaches to cholesterol control is dependent on the patient’s risk of developing cardiovascular disease in the next 5 years. The higher the risk, the more aggressive the therapy approach.
- Non-drug therapy is critical to lowering elevated cholesterol. It is beneficial also when added to pharmacotherapy.
- There are 7 drug classes that reduce cholesterol. The most commonly used 4 classes are the statins (HMG-CoA reductase inhibitors), the fibrates, ezetimibe (a brush border enzyme inhibitor) and the PSCK-9 inhibitors.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.

