2.20 Statins
John Smithson
Be able to:
- relate the mechanism of action of the statins to their cholesterol lowering effect
- understand the common and catastrophic side effects of the statins
HMG-CoA reductase inhibitors or statins include atorvastatin, fluvastatin, pravastatin, rosuvastatin and simvastatin. They all share a common suffix – ‘statin’, hence they are collectively referred to as ‘statins’. Statins are reversible competitive inhibitors of the enzyme HMG-CoA reductase. The enzyme HMG-CoA reductase is a rate limiting step in the conversion of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) to mevalonate which eventually is used in the synthesis of cholesterol. The conversion of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) to mevalonate is carried out in the liver and the statins block this conversion leading to reduced hepatic production.

Cholesterol is necessary for a broad range of physiological functions including the production of hormones, bile, cell membranes, catecholamines and other neurotransmitters. The supply of cholesterol is sourced via two main mechanisms (see figure below):
- Production of endogenous cholesterol by the liver and
- Dietary consumption of cholesterol.
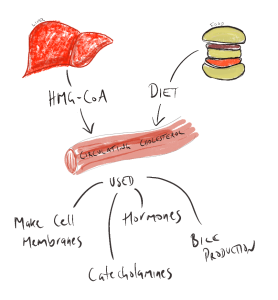
When dietary supply of cholesterol is in excess, statins can be used to reduce the endogenous (liver) production of cholesterol. Reduced liver production of cholesterol makes total blood cholesterol scarcer. More cholesterol is scavenged from the circulating blood thereby reducing circulating plasma cholesterol levels. Because there is less circulating cholesterol, there is a reduction of build-up of cholesterol containing fatty plaques is the arteries.
Common side effects of statins include myalgia, mild and transient GI symptoms, insomnia, nightmares, dizziness and elevated aminotransferase levels. Statins are associated with myalgia, myopathy and a particularly serious expression of myalgia – rhabdomyolysis.
Rhabdomyolysis is the breakdown of skeletal muscle fibers with the resultant degraded products released into the bloodstream. Symptoms of rhabdomyolysis included:
- severe unexplainable severe muscle pain – typically in the larger muscles
- muscle weakness
- dark brown or red urine.
This may be accompanied by reduced urine output. While rare, rhabdomyolysis is a serious condition and should be treated without delay.
Myopathy vs rhabdomyolysis
Comparative information – statins
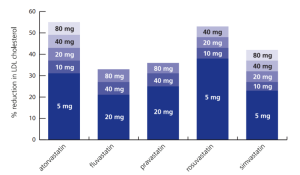
LDL Lowering Effects
- Atorvastatin, Rosuvastatin and Simvastatin are more potent than Fluvastatin or Pravastatin.
- Administration but the strongest cholesterol (LDL-C) lowering effect are to be found with atorvastatin and rosuvastatin.
- Shorter acting statins (fluvastatin, pravastatin and simvastatin) should be taken in the evening (Maximises levels when liver is most active in producing cholesterol), however – this is not too important if taking dose in the evening effects compliance.
- Nighttime dose is not necessary with longer acting stations (atorvastatin or rosuvastatin). Mainly beneficial for very short acting statins such as simvastatin and fluvastatin.
Dosage
📺 Watch video: Mechanism of action of statins. (11:21 min)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
