2.3 What is Hypertension?
John Smithson
Hypertension
Hypertension is the term for high blood pressure over a long period of time. The current guidelines define hypertension as a sustained blood pressure that is greater than or equal to a systolic pressure of 140mmHg and/or a diastolic pressure of 90mmHg, though the definition of hypertension is arbitrary. This is because we know that there is a continuous relationship between increasing blood pressure and the incidence of complications associated with high blood pressure.
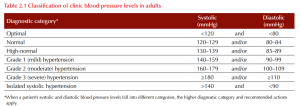
The Heart Foundation Guideline for the diagnosis and management of hypertension in adults 2016 classifies blood pressure into 7 categories:
Consequences of persistent elevated blood pressure
The pathophysiology and perpetuation of the hypertensive state involves structural changes, remodeling, and development of atherosclerosis in arterioles. Endothelial injury hastens the progression of atherosclerotic plaque development, leading to some of the known complications of untreated hypertension that include:
- Coronary artery disease
- Stroke
- Peripheral artery disease.
Non-ischaemic complications of hypertension are often attributable to increased myocardial workload or damage to the fragile microcirculation of the kidneys and eyes. Such complications include:
- Heart failure
- Arrhythmias
- Chronic kidney disease
- Retinopathy
Hence, blood pressure cut-offs for treatment of hypertension may be lower than 140/90 for people with comorbidities that increase their risk of complications associated with hypertension, and/or for people with a high absolute CV risk.
Key Takeaways
Hypertension and cardiovascular risk
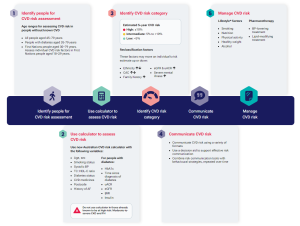
Patients should have their cardiovascular risk calculated to identify appropriate treatment. The Australian guideline and calculator for assessing and managing cardiovascular disease risk identifies 5 steps in the process:
Activity
Now you have looked at your own cardiovascular risk – I hope it is low, let’s have a look at mine…
John’s CV risk
John is:
- A 50-year-old male
- Never smoked
- Systolic BP is 135 mmHg
- Cholesterol
- Total cholesterol 5 mmol/L
- HDL 1.1 mmol/L
- Takes no medicines
- No history of AF
- Lives in postcode 4812
- Does not have diabetes
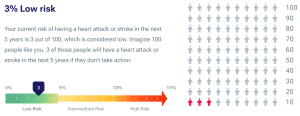
John has a low (3%) risk of a cardiovascular event in the next 5 years. (Well done me!)
This means I have a 3 in 100 chance of having a heart attack or stroke in the next 5 years.
Remember CV risk assessment may be inappropriate if:
- There is known CVD (= automatically high risk)
- Persistently elevated BP ≥ 180/110mmHg (= automatically high risk)
- There is evidence of target organ damage at the time of initial presentation (= automatically high risk)
- The patient is ineligible for CV risk assessment using the calculators because they are too young (the calculator has not been validated for patients aged less than 30 years (if Aboriginal or Torres Strait Islander) or other patients aged less than 45 years).
Next, let’s look at the epidemiology of high blood pressure in Australia.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
