2.7 ACE Inhibitors and Angiotensin II Receptors
John Smithson
ACE Inhibitors and Angiotensin II Receptors
Learning Outcomes
Be able to:
- Describe the Renin-angiotensin-aldosterone system in terms of its role in blood pressure regulation.
- Apply knowledge of the pharmacology of ACE inhibitors and angiotensin II receptors (A2RB’s) in the control of blood pressure.
- Apply knowledge of the pharmacology and its effect on the physiology to predict common and catastrophic side effects.
- Describe strategies to maximise the benefits of ACE inhibitors and A2RBs in clinical practice.
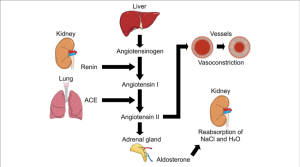
Angiotensin Converting Enzyme Inhibitors (ACE inhibitors) and Angiotensin II receptor blockers (A2RBs) work on different parts of the same system – the Renin-Angiotensin-Aldosterone system (RAAS). Understanding the RAAS will help in understanding how the ACE Inhibitors and A2RB’s work so let’s look at this first.
The Renin-Angiotensin-Aldosterone System (RAAS)
RAAS is a hormonal system that controls blood pressure and fluid balance. The diagram in the figure below gives an overview.
What happens in the RAAS?
📺 Watch the following short video explaining the Renin-angiotensin-aldosterone system and the connection between this and fluid volume increase and elevated blood pressure. (7.02 min)
Introduction to ACE inhibitors and A2RB’s
ACE inhibitors are used to manage common conditions like hypertension, chronic heart failure, diabetic neuropathy and prevention of progressive renal failure in patients with diabetes or persistent proteinuria (not sure what proteinuria is? Why not find a description in the pharmacology for healthcare professionals textbook or search the web).
Similarly, A2RBs are indicated in the treatment of hypertension and chronic heart failure. ACE inhibitors and A2RB’s share many similarities in terms of therapeutic outcomes but have slightly different side effect profiles. But first, how do they work?
How do ACE inhibitors work?
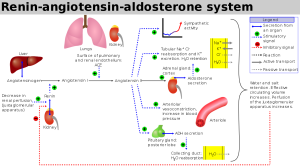
ACE inhibitors competitively block the action of Angiotensin Converting Enzyme (ACE) which is responsible for the conversion of Angiotensin I (a weak vasoconstrictor) to Angiotensin II (a potent vasoconstrictor). A thorough understanding of the RAAS is critical to understanding the action and side effect profile of ACE inhibitors and A2R-blockers. Figure 3 below shows where ACE Inhibitors and A2RB’s act on the RAAS.
Renin Angiotensin Inhibitors, Source: https://www.lecturio.com/concepts/renin-angiotensin-aldosterone-system-inhibitors/
When the ACE inhibitors competitively bind to the enzyme ACE and reduce the conversion of inactive Angiotensin I to the potent active vasoconstrictor Angiotensin II (AT-II) it causes:
- A decrease in vascular tone reducing blood pressure (less AT-II)
- Less aldosterone release from the adrenal cortex, reducing sodium and water reabsorption from the distal convoluted tubule and collecting duct – reducing blood volume (Less AT-II)
- Increased release of renin due to loss of negative feedback on the juxtaglomerular cells in the kidney
- Increased bradykinin levels (bradykinin is a vasodilator and is noteworthy from a side effect perspective) due to inhibition of ACE.
How do Angiotensin-II Receptor Blockers (A2RB’s) work?
Similar to ACE inhibitors, Angiotensin-2 receptor blockers (A2RB’s) are used in the management of hypertension and heart failure where ACE inhibitors are not tolerated (see below for major side -effects of ACE inhibitors). A2RB’s block the action of angiotensin II at the angiotensin II type-1 receptor, thereby mediating the action of angiotensin II on blood vessels and aldosterone release. The benefit of targeting the angiotensin II type-1 receptor is that bradykinin breakdown is not interrupted and there is less chance of hyperkalemia.
The A2RB’s undergo a range of uncommon metabolic pathways. Some are metabolized by CYP-450 UDP-glucuronosyltransferases, some are excreted unchanged in the kidney. Other side effects and drug interactions are shared between ACE inhibitors and A2RBs.
Let’s explore the ACE Inhibitor and A2RB Drugs in more detail
ACE inhibitors include the drugs: captopril (the first ACE inhibitor), enalapril, fosinopril, Lisinopril, perindopril, quinapril, ramapril and trandolapril. Like some other drug classes – they share a suffix that gives a clue to their drug class. In the case of ACE inhibitors, they share a suffix of ‘pril’.
Angiotensin II receptor blockers (A2RBs) include the drugs candesartan, eprosartan, irbesartan, losartan, olmersartan, telmisartan and valsartan. They also share a common suffix aiding class identity: ‘sartan’. This explains why this group of drugs is also known as the ‘sartan’s’.
📺 Watch the vodcast on the pharmacology of ACE inhibitors and A2RBs. (11:09minutes)
Side Effects of ACE Inhibitors
Hypotension: especially early dose postural hypotension is common, particularly in the elderly. Other class-related side effects of note include dizziness, fatigue, nausea, headache and renal impairment. Three significant side effects of ACE inhibitors are hyperkalemia, cough and angioedema.
Hyperkalemia: as a result of decreased circulating AT2, a reduced amount of aldosterone is secreted from the adrenal cortex. Aldosterone influences the excretion of potassium and reabsorption of sodium in the distal convoluted tubule and collecting ducts. Therefore, reduced levels of circulating AT2 result in decreased secretion of aldosterone and therefore increased levels of serum potassium – leading to hyperkalemia.
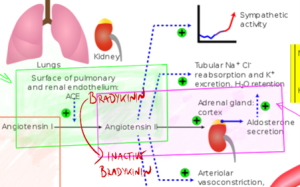
Cough: One famous side effect of ACE inhibitors (and probably the major driver for the development of A2RBs) is the propensity for ACE inhibitors to cause cough in some patients. The cough is caused by the accumulation of bradykinin. Under normal circumstances angiotensin converting enzyme converts angiotensin I to angiotensin II but is also inactivates bradykinin (bradykinin is a vasodilator and pro-tussive agent). The inactivation of ACE produces elevated levels of bradykinin. The accumulation of bradykinin stimulates the cough reflex and produces a dry cough in around 5-10% of patients. The figure below shows the normal pathway of bradykinin inactivation by ACE.
Angioedema
In worst cases outcomes, the swelling of the subcutaneous or submucosal tissue and tissues in the throat which can cause asphyxiation and death (see figure part a and b below). As angioedema is life threatening, urgent medial referral is appropriate.

Dosing and drug interactions
Most ACE inhibitors have a sufficiently long half-life to allow for single daily dosing with the exception of captopril which is commonly given twice a day. All ACE inhibitors (with the exception of captopril and lisinopril) are pro-drugs. They are converted to their active metabolite by hepatic esterases. Drug interactions of note include:
- Potassium sparing diuretics – risk additive effect on accumulation of serum potassium (we will explore the diuretic drugs in a separate topic).
- Loop diuretics which can cause first dose hypotension due to the loop diuretics reasonably powerful diuretic effect (we will explore the diuretic drugs in a separate topic).
- Non-Steroidal Anti-inflammatory Drugs (NSAIDs) – which can increase the risk of hyperkalemia and reduce ACE (and A2RB) effect.
- Lithium – decreased renal clearance of lithium.
📺 Watch the vodcast on the side effects of ACE inhibitors and A2RBs. (8:16 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.