2.8 Calcium Channel Blockers
John Smithson
Calcium Channel Blockers (CCB)
In this topic we will look at the calcium antagonists also known as calcium channel blockers of which there are two main groups. We will learn about the different calcium channel blockers and explore their pharmacological effects on cardiac and smooth muscle.
Learning Outcomes
Be able to:
- List the two different groups of calcium channel blockers
- Explain the differences in how the two groups work and what they are used for clinically
- Describe the mechanism of action of calcium channel blockers on smooth muscle
- Explain the pharmacology of the two groups including side effects and interactions.
Introduction
Calcium Channel Blockers (CCB’s) are commonly used in the management of hypertension and angina. They act on calcium channels in myocardial and vascular smooth muscle to:
- reduce heart rate and contractility, and
- reduce vasoconstriction of vascular smooth muscle.
The CCB’s available in Australia include amlodipine, clevidipine, diltiazem, felodipine, lercanidipine, nifedipine, nimodipine and verapamil. Calcium channel blockers are commonly grouped into two main classes:
Non-dihydropyridine calcium channel blockers
The non-dihydropyridine CCBs act mainly on cardiac and arteriolar smooth muscle to reduce contractility, heart rate, conduction and arteriolar vessel constriction. Contractility of the cardiac muscle cell is reduced as CCB’s block the inward movement of calcium through L-type calcium channels in phase 0 and phase 2 of the cardiac action potential. As there is less calcium entering the cell and less calcium is released from the sarcoplasmic reticulum. As less calcium is available to interact with troponin-C and less myocin heads are able to bind with the actin, contraction of the myocardial tissue is reduced.
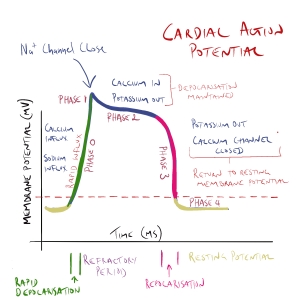
In sinoatrial (SA) and atrioventricular (AV) junction node tissue, non-dihydropyridine CCB’s decrease automaticity by blocking the inward flow of calcium ions into the cell slowing depolarization in phase 0 of the cycle (remember –depolarization of nodal tissue is normally triggered by the inward flow of calcium into the cell – not sodium as in heart and skeletal muscle cells). Blocking the influx of calcium decreases the rate of depolarization depressing automaticity. This increases refractory time and decreases heart rate.
Dihydropyridine calcium channel blockers
These act mainly of arteriolar smooth muscle. The dihydropyridine CCBs share a common suffix ‘ipine’, (amlodipine, clevidipine, felodipine, lercanidipine, nifedipine and nimodipine) which makes them easy to spot in a crowd.
Like the non-dihydropyridine CCBs, they block the inward flow of calcium into the coronary arteries and arterioles in the peripheral circulation. The functional effect is the dilatation of arterioles and coronary arteries is to reduce peripheral vascular resistance and increase nutrient and oxygen supply to the heart. The following video briefly shows the effect of reduced calcium influx into the arteriolar smooth muscle cell and its negative effect on the activation of the myosin-actin complex.
📺 Watch: For a video explanation of how calcium channel blockers reduce smooth muscle contraction in the arterioles watch the following video: Mechanism of action for Calcium Channel Antagonists (0:44 minutes)
While the non-dihydropyridine CCB’s affect both arteriolar smooth muscle and cardiac nodal and cardiac muscle cells, they have a much more pronounced negative central cardiovascular effect. That is they have greater negative chronotropic and ionotropic effect compared with the dihydropyridine CCBs which act mainly on arteriolar smooth muscle. Of the two non-dihydropyridine CCBs, verapamil has the greatest effect on contractility and automaticity and cannot be used with other drugs that also reduce contractility or heart rate (such as the beta-blocking drugs). The table below (Table 1) provides a comparison of the cardiovascular effects of calcium channel-blocking drugs available in Australia.
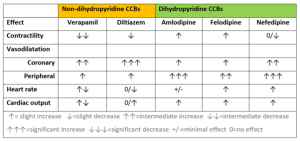
From the table above, you can see the calcium channel blockers can have different effects depending on the agent and sub-class. This is because unlike many other drug classes – CCBs have fairly diverse chemical structures.
The trends worth noting are:
- non-dihydropyridine CCBs reduce contractility of the heart
- all produce some degree of coronary artery or peripheral artery vasodilatation
- they have mixed effect on heart rate and
- they all trend towards increasing cardiac output.
Amlodipine has a long half-life and is typically given once a day. The other CCBs typically have a shorter active half-life and are either given more than once a day or are formulated in control release tablets. A large number of drugs interact with CCBs as they are primarily metabolized by CYP3A4 (which is affected by a number of drugs) (all undergo hepatic metabolism).
Probably the best-known drug interaction is between beta-adrenergic blocking drugs and verapamil. As both drugs reduce cardiac rate and contractility, the additive effect risks heart block and severe bradycardia. Common adverse effects include constipation, bradycardia, hypotension, dizziness, skin flushing and rash, dry mouth and oedema of the ankles. CCBs can also cause gingival hyperplasia (not heard of gingival hyperplasia before? Why not look it up on the web?).
📺 Watch the following short video explaining the pharmacology of calcium channel blockers. (20.59 min)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
