2.9 Diuretics
John Smithson
Diuretics
For this topic you will need to revise the anatomy and physiology of the renal system as you will need this knowledge to understand the focus this week which is on diuretics and their uses in clinical practice.
Learning Outcomes
Be able to:
- List the different types of diuretics and their uses in the clinical setting
- Explain the mechanism of action for each type of diuretic
- Describe common side effects and the implications for patients taking these drugs.
Revision of Anatomy and Physiology of the Renal System
An understanding of renal anatomy and physiology is critical to your understanding of the action of drugs that affect the renal system such as diuretics. You are already familiar with this system but as you progress through this week’s work, you may want to refer back to the following sections to ensure you have a good understanding. The most important renal system anatomical and physiological concepts you may want to revise from your anatomy and physiology text [Tortora, GJ., Derrickson, B., Burkett, B., Peoples, G., Dye, D., Cooke, J., et al. Principles of anatomy and physiology. Second Asia-Pacific ed. Queensland, Australia: John Wiley & Sons; 2019] are:
- Blood and nerve supply of the kidneys (Page 1459–1461 of above text)
- The nephron (Page 1461-1467 of above text)
- Glomerular Filtration Rate (P1470-1473 of above text)
- Renalautoregulation of GFR.
- Neuralregulation of GFR.
- Hormonalregulation of GFR.
- Principles of tubular reabsorption and secretion. (Page 1473-1476 of above text)
- Reabsorption and secretion in the proximal convoluted tubule. (Page 1476-1479 of above text)
- Reabsorption in the nephron loop. (Page 1479-1481
- Reabsorption in the early distal convoluted tubule. (Page 1481 of above text)
- Reabsorption and secretion in the late distal convoluted tubule and collecting duct. (Page1481 of above text)
- Homeostatic regulation of tubular reabsorption and tubular secretion. (Page 1481-1485 of above text)
- Production of dilute and concentrated urine. (Page 1485-1491 of above text)
Introduction to Diuretics
There are four main classes of diuretics:
- Loop diuretics such as frusemide, bumetanide and etacrynic acid.
- Thiazide diuretics such as hydrochlorothiazide and indapamide
- Potassium-sparing diuretics such as amiloride and spironolactone and lastly
- Osmotic diuretics such as mannitol.
Of the four types, osmotic diuretics such as mannitol are the most potent and one of the least commonly used. The two most commonly used diuretic classes in Australia are loop diuretics (i.e. frusemide) and thiazide diuretics (hydroclorothiazide). Diuretics are used for hypertension and a broad range of conditions that require fluid load reduction such as cirrhosis, partial renal failure and oedema, symptomatic management of congestive heart failure and other conditions that result in peripheral oedema.
All diuretics modify renal function to reduce the reabsorption of water from the filtrate via the common mechanism of increasing sodium excretion in the filtrate.
🎧👁️ Watch the Lecture Video on an Introduction to Diuretics (9:33 minutes)
Loop Diuretics
Of the 3 available loop diuretics frusemide, bumetanide and etacrynic acid – frusemide is the most commonly used agent. Loop diuretics are a moderately potent diuretic second only to osmotic diuretics. They are all relatively short acting lasting about 4-6 hours. Their potency results from their site of action on the nephron – that site being the thick ascending loop of Henle. Loop diuretics are used for conditions that require fluid load reduction but unlike thiazide diuretics are not used in the management of hypertension.
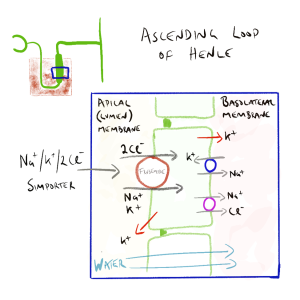
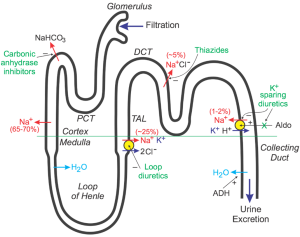
Loop diuretics are actively secreted into the lumen via the proximal tubule. In the Loop of Henle, they inhibit the Na+/K+/2Cl– cotransporter reducing sodium reabsorption (see figure below). As water follows sodium, the increased sodium concentration in the filtrate reduces the osmotic gradient reducing water movement back into the interstitial space surrounding the nephron (and eventually the blood). Loop diuretics are so potent because the Loop of Henle is the major site of sodium reabsorption – accounting for between 15-25% of sodium and chloride reabsorption normally.
Loop diuretics are also sometimes called potassium-wasting diuretics. This is because of the nature of the symporter the loop diuretics block and the normal movement of ions (sodium and potassium) from the filtrate to the blood. When frusemide (or other loop diuretics) block the Na+/K+/Cl– symporter, water reabsorption is reduced and the excretion of sodium is increased. So too is the loss of potassium in the filtrate.
Loop diuretics are well absorbed from the GIT and have good oral bioavailability. They are commonly given by mouth but can also be administered in IV form.
Side Effects of Loop Diuretics
Frusemide and other loop diuretics can cause electrolyte disturbances (calcium, potassium, sodium, chloride, magnesium loss) though this is dose related. Other common side effects include postural hypotension, dehydration, dizziness, rash and metabolic alkalosis (H+ is lost in the filtrate also due to loop diuretic effect). They can also precipitate gout (they decrease excretion of uric acid) and cause ototoxicity. Ototoxicity is uncommon in normal doses but can occur when administered with other ototoxic drugs.
Unlike other diuretics, loop diuretics are high-ceiling diuretics. This means they are effective over a very broad range of doses and the greater the dose given, the greater the effect. This is useful in renal impairment. Though like all drugs, the higher the dose, the higher the risk of side effects – particularly sodium and potassium loss and ototoxicity.
📚 Read/Explore
-
- Loop diuretics in Chapter 30 The kidney and urinary system (page 389-399) in the 9th edition Rang and Dale’s Pharmacology.
🎧👁️ Watch the Lecture Video on an overview of Loop Diuretics (5:18 minutes)
Thiazide diuretics
Thiazide diuretics are commonly used to induce diuresis and as an adjunct therapy for hypertension. Examples of thiazide diuretics include:
- Chlorthialidone
- indapamide
- hydrochlorothiazide.
Like loop diuretics, thiazide diuretics are actively secreted into the filtrate via the proximal tubule. They are transported to the distal convoluted tubule in the filtrate where they block the action of the Na+ /Cl-symporter, reducing sodium and chloride reabsorption. Because the distal convoluted tubule is only responsible for about 5% of the sodium reabsorption, they are much less potent compared with loop diuretics. The sodium concentration of the filtrate is elevated when it arrives in the collecting duct. Here, sodium is transported back into the cells of the collecting duct in exchange for potassium which is transported from the blood to the filtrate (urine). This explains the loss of potassium with thiazide diuretics which is unrelated to its action in the distal convoluted tubule. In addition to sodium, chloride and potassium, thiazide diuretics also cause the excretion of magnesium.
📺 Watch the Youtube video on Thiazidediuretics (6:08 minutes)
Thiazide diuretics are low ceiling diuretics. Their effect on diuresis increases with dose up to a maximum ceiling which in the case of hydrochlorothiazide is about 50mg. They have similar side effects to those of loop diuretics: electrolyte disturbances, orthostatic hypotension, dizziness, rash, incontinence, precipitation of gout, blood glucose derangement. The risk of hypokalaemia for thiazide diuretics and loop diuretics is dose related and increased when given with other drugs that cause potassium wasting.
🎧👁️ Watch the Lecture Video on an overview of Thiazide Diuretics (3:39 minutes)
Other diuretics: osmotic diuretics & potassium-sparing diuretics
Osmotic diuretics such as mannitol increase the osmotic concentration of the filtrate, thereby causing significant diuresis. Spironolactone, triamterene and amiloride are potassium-sparing diuretics. Spironolactone acts on the aldosterone receptor reducing the water-reabsorbing effects of aldosterone. Amiloride and triamterene inhibit sodium reabsorption in the distal tubule by blocking the sodium channels. They block the exchange of sodium and potassium and therefore preserve serum potassium levels. Due to the location of action, spironolactone, amiloride and triamterene are considered weak diuretics.
🎧👁️ Watch the Lecture Video on an overview of Other Diuretics (4:09 minutes)
🔑 Learning Activity
Revise the renal system and have a good understanding of the different types of diuretics and how they work.
- Describe the four types of diuretics and their clinical uses.
- Understand and be able to explain the mechanism of action for thiazide diuretics.
- Describe the pharmacology and side effects of diuretics and what to watch out for in practice.
It may help to put the 4 different types of diuretics in a table to compare/contrast the pharmacology, mechanism of action, side effects and practice points etc.
Example:
| Loop Diuretics | Thiazide Diuretics | Potassium-Sparing Diuretics | Osmotic Diuretics | |
|---|---|---|---|---|
| Mechanism of action | ||||
| Site of action | ||||
| Potency | ||||
| Effect on
Electrolytes |
||||
| Side effects | ||||
| Clinical uses | ||||
| Practice Points |
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.