3.3 Management of Heart Failure (with Reduced Ejection Fraction)
Therapeutic Objectives
- Relieve symptoms
- Improve quality of life
- Slow disease progression
- Prevent acute exacerbations / hospitalisation
- Prolong active life.
Principles of Heart Failure Management
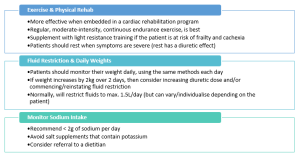
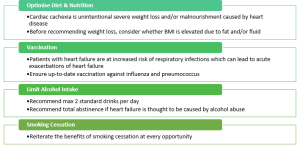
Non-Pharmacological Management
Non-pharmacological treatment strategies are an essential consideration. These are as important as pharmacological treatment for heart failure.
Pharmacological Management
Key Takeaways
- Angiotensin-Converting Enzyme (ACE) inhibitors or Angiotensin-Receptor Blockers (ARBs) *
- Aldosterone antagonists
- Beta-blockers (HF-specific)
- Sodium-glucose cotransporter 2 (SGLT2) inhibitors
We also have another class that is an angiotensin-receptor neprilysin inhibitor (ARNI). There is only one combination drug in this class, sacubitril with valsartan, brand name (Entresto(R)). According to current consensus guidelines, the ARNI may be started first line, without the need to transition from an ACEI or ARB. However, this is not often seen in practice, because of current PBS restrictions, to reduce the cost to the patient. At the time of writing, this ARNI is only PBS-subsidised as a second-line agent to be used in place of the ACEI or ARB if the patient was trialled on an ACEI or ARB and a beta blocker for a period of time with persistent symptoms despite this. It is essential that if the ARNI is started, the ACEI or ARB is ceased. And if swapping from an ACEI to the ARNI, there must be a 36-hour washout period.
Combination drug therapy with use of all 4 pillars (i.e., an ACEI or ARB or ARNI, plus a beta blocker, plus an aldosterone antagonist, plus an SGLT2 inhibitor), improves prognosis and controls symptoms of HFrEF better than use of any 1 drug class alone.
A Snippet of Current Guidelines
This is the current standard of care for every patient with heart failure with reduced ejection fraction (HFrEF) irrespective of disease severity.
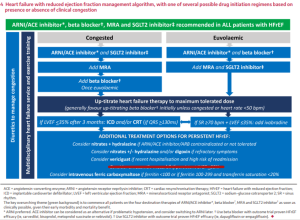
Already you can see that management of HfrEF is divided down the middle. It is split depending on whether the patient presents with overt signs and symptoms congestion or without any signs and symptoms of congestion (in which case they would be considered euvolaemic or ‘not fluid overloaded’). The main difference between the 2 is that beta blockers aren’t started if the patient is congested at the time of their diagnosis (beta blockers aren’t started until the patient is euvolaemic).
You can also see diuretics on the left spanning vertically across every row alongside the non-pharmacological recommendations. So, diuretics can be used whenever needed to help to manage congestion, on top of other maintenance therapies outlined in this figure.
You can see a strong recommendation for use of the 4 pillars at the top of this figure in the green box.
Then we up-titrate the doses of these heart failure therapies according to tolerability.
Later line treatment options are also suggested in these guidelines.
Dose Titrations
- If the ejection fraction recovers, the current recommendation is for neurohormonal antagonists (ACEI/ARB/or ARNI, and MRA, and beta blocker) to be continued long-term at target doses, unless the reversible cause of the heart failure has been identified and corrected.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
