3.4 Drugs for Heart Failure (with Reduced Ejection Fraction)
Diuretics
Diuretics are indicated to manage clinical signs and symptoms associated with heart failure.
There are no proven mortality benefits associated with the use of diuretics. However, they are still an essential consideration, because they do help patients prevent and treat congestion due to heart failure, and improve quality of life.
Sometimes, patients will be prescribed diuretics to take the same dose each day. Other times, patients might just need a dose every now and then (in which case PRN use is also appropriate).
Loop diuretics are better than thiazide diuretics in the context of heart failure management because they cause more free water clearance by the kidneys and have a faster onset of action too. Examples of loop diuretics include furosemide and bumetanide.
Refer to last week’s content to revise the pharmacology of diuretics.
The 4 Pillars
As discussed previously, patients with heart failure with reduced ejection fraction (HFrEF) should be prescribed one medication from each of the 4 pillars outlined below, for mortality benefits, unless contraindicated or not tolerated.
|
Angiotensin-Converting Enzyme Inhibitor (ACEI) OR Angiotensin Receptor Blocker (ARB) OR Angiotensin Receptor Neprilysin Inhibitor (ARNI) |
Mineralocorticoid Receptor Antagonists (MRAs) | Beta Blockers | SGLT2 Inhibitors |
|
An ACEI is recommended first line for all patients with HFrEF, unless contraindicated or not tolerated. ACEIs have been proven to decrease mortality and hospitalisations for patients with HFrEF. Angiotensin receptor blockers (ARBs) are recommended if ACEIs are contraindicated or not tolerated, e.g., due to cough. Morbidity and mortality benefits are the same for ARBs as they are for ACEIs. It is important to note that ACEIs and ARBs must never be used together, unless on the advice of a specialist cardiologist, but this is extremely rare! Refer to last week’s content to revise the pharmacology of ACEIs and ARBs. An Angiotensin Receptor Neprilysin Inhibitor (ARNI) is an alternative to ACEIs and ARBs. See below. |
Mineralocorticoid receptor antagonists (MRAs) are also known as aldosterone antagonists or potassium sparing diuretics. It is important to remember that although they can be referred to as diuretics, they are being used in HFrEF for their ability to antagonise aldosterone, not because of any additional diuretic effect. The 2 drugs in this class are spironolactone and eplerenone. Eplerenone has good evidence in heart failure that is secondary to a myocardial infarction, whereas spironolactone has more evidence in heart failure with reduced ejection fraction across the board (irrespective of the cause). Refer to last week’s content to revise the pharmacology of MRAs. |
Only 4 beta blockers (bisoprolol, carvedilol, controlled release metoprolol and nebivolol) have evidence supporting their use as part of the overall approach to treatment of heart failure with reduced ejection fraction. Patients with heart failure should not be prescribed any other beta blocker (e.g., atenolol). Historically, beta blockers were contraindicated in heart failure. But now, because of the pathophysiology we discussed earlier, beta blockers are part of standard therapy in HFrEF. Remember we need to ensure that the patient is stable (that they’re not experiencing an acute exacerbation and that they’ve got no signs/symptoms of congestion) before we start the beta blocker. |
New evidence is strongly supportive of using an SGLT2 inhibitor (dapagliflozin or empagliflozin) for all patients with HFrEF, even for those without diabetes. Mortality and morbidity benefits have been demonstrated. Upon initiation of a SGLT2 inhibitor, it is important to monitor the patient’s weight (to assess their fluid status), as SGLT2 inhibitors can have a mild diuretic effect. Euglycaemic ketoacidosis is an uncommon complication of SGLT2 inhibitor use. The risk of euglycaemic ketoacidosis is increased if the patient is fasting or unwell (dehyrated, vomiting, diarrhoea, etc.). Therefore, the SGLT2 inhibitor must be withheld in these instances. |
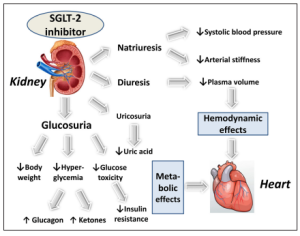
Sodium-Glucose Co-Transporter 2 Inhibitors (SGLT2 Inhibitors)
The pharmacology of SGLT2 inhibitors is discussed later with the diabetes content. However, the cardiovascular benefits of SGLT2 inhibitors are thought to be a result of their haemodynamic and metabolic effects. This is demonstrated in the figure below:
Angiotensin Receptor Neprilysin Inhibitor (ARNI)
This class of medication contains only a single combination drug option at this stage. That is sacubitril with valsartan (brand name Entresto®).
In practice, therapy is escalated to Entresto if the patient has persistently reduced ejection fraction < 40% despite having been on an ACEI or ARB plus a beta blocker for 3-6 months at the max tolerated maintenance dose of these medications.
It is absolutely critical that if we switch a person from an ACE inhibitor to Entresto®, there must be a 36-hour period between the last dose of the ACEI and the first dose of the Entresto®. An ACEI and Entresto must never be taken together.
The ARNI should be used with:
- A MRA (aldosterone antagonist), AND
- A heart failure – specific beta blocker, AND
- A SGLT2i and a beta blocker) for additional mortality benefits.
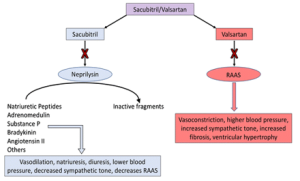
Contraindications, precautions, and adverse effects of sacubitril+valsartan are similar to those of ACE inhibitors.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
