3.6 Introduction to Stable Angina
John Smithson
Introduction and symptoms of stable angina
Stable angina (also known as angina pectoris) is one of the common coronary ischaemic syndromes. Other more serious coronary syndromes include acute coronary syndromes S-T elevation myocardial infarction (a form of heart attack), non-ST elevation acute coronary syndrome (another form but less serious form of heart attack) and unstable angina. Stable angina differs from the other forms of coronary ischaemic syndromes as it is:
- constant in duration and severity;
- is predictable in onset – often brought about by exertion, emotional stress or cold temperatures, but predictably so;
- does not involve any myocardial ischaemia;
- does not involve any changes on ECG; and
- does not involve elevation of cardiac markers.
The symptoms of stable angina have consistent features which include the onset of retrosternal chest discomfort that lasts for 10 minutes or less, subsides with prompt rest and the pattern of onset and symptoms is predictable and remains the same. In comparison, unstable angina can involve low level myocardial ischaemia that does not produce the cardiac biomarkers that would indicate myocardial damage, symptoms that occur at rest, symptoms that change from the normal pattern of angina (more severe pain, longer duration of pain) and may not respond to nitroglycerin.
Cause of stable angina
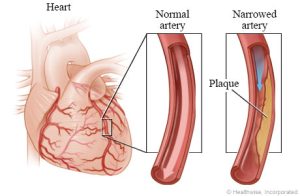
Angina indicates a myocardial oxygen supply / demand imbalance. It is typically caused by some form of artherosclerotic obstruction of the coronary arteries, commonly cholesterol plaque obstruction, limiting the supply of blood to myocardial tissue. The imbalance in supply causes a temporary deficit of oxygen in the myocardial tissue and subsequent build-up of lactic acid from the metabolism of sugars to maintain energy supply (the heart typically uses aerobic metabolism for the production of energy, rarely the use of glucose or glycogen in anaerobic metabolism).
While stable angina is not associated with myocardial tissue damage, it can progress onto unstable angina or a myocardial infarction (STEMI or non-STEMI) if not treated appropriately.
Types of stable angina
There are three types of angina plus unstable angina. They differentiate in cause mostly. Explore the pathophysiology of the three types of angina below:
The treatment of these different types of angina overlap. For the purpose of this module, we will concentrate on the management of stable angina as it is by far the most common type.
📺 Watch the vodcast on the Introduction to Stable Angina. (12:51 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
