3.8 Management of Stable Angina – Secondary Prevention
John Smithson
Secondary Prevention of Atherosclerotic Cardiovascular Events
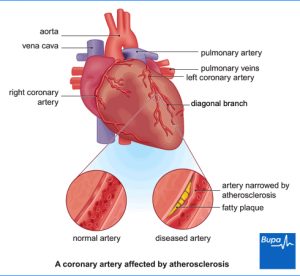
Managing patients with atherosclerotic cardiovascular disease (ASCVD), including those with stable angina, requires a comprehensive approach to secondary prevention. This strategy aims to prevent the recurrence of cardiovascular events and reduce overall mortality.
Non-Pharmacological Interventions
Non-drug management plays a crucial role in secondary prevention and includes several lifestyle modifications. Weight reduction, smoking cessation, dietary changes, alcohol reduction, and increased physical activity are all highly beneficial. Smoking cessation alone has been shown to reduce the risk of all-cause mortality by approximately 36% in patients with ASCVD. These lifestyle changes not only improve cardiovascular health but also enhance overall well-being and longevity. The information below lists the common modifiable risk factors for all CVD.
Pharmacological Interventions for Secondary Prevention of Angina
Secondary prevention typically involves a combination of medications aimed at reducing cholesterol, high blood pressure and reduce the risk of clot formation. Statins are commonly prescribed to lower cholesterol levels, stabilize atherosclerotic plaques, and in some cases, reduce the size of existing plaques. Antiplatelet drugs, such as aspirin or clopidogrel, or a combination of aspirin and rivaroxaban, are used to prevent thrombosis, thereby reducing the incidence of myocardial infarction and death.
The two most commonly used antiplatelet drugs for the prevention of platelet plugs around atherosclerotic plaques are aspirin or clopidogrel (if aspirin is not tolerated). Less commonly, aspirin plus rivaroxaban is used.

Low-dose (100-150 mg) enteric-coated aspirin is a common, effective and cost-effective antiplatelet option. The tablet is enteric coated to reduce the risk of gastric irritation and is given at a low dose reducing the risk of other side effects.
If patients cannot tolerate aspirin, clopidogrel (75 mg once daily) serves as a viable alternative.
Rivaroxaban may be beneficial in patients with poly-vascular disease when added to aspirin, although it increases the risk of gastrointestinal bleeding.
Blood Pressure Management
Another critical aspect of secondary prevention is blood pressure management. Effective control of hypertension is essential in reducing cardiovascular risk. Angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), and dihydropyridine calcium channel blockers are typically recommended for managing high blood pressure. Reviewing the previous chapter on blood pressure management is important for optimizing treatment strategies.
In summary, secondary prevention of atherosclerotic cardiovascular events involves a multifaceted approach that includes both lifestyle modifications and pharmacological treatments. Implementing these strategies effectively can significantly reduce the risk of recurrent cardiovascular events and improve patient outcomes.
Mechanism of Action of Antiplatelet Drugs in Secondary Prevention of Atherosclerotic Cardiovascular Events
In the context of secondary prevention for atherosclerotic cardiovascular events, understanding the role of antiplatelet drugs is essential. These medications are designed to reduce the risk of blood clot formation by interfering with the platelet activation and aggregation processes, which are critical early steps in clot formation.
Platelet Adhesion and the Cascade of Events
During blood clot formation, platelet adhesion is an early and crucial step. When atherosclerotic plaques in coronary arteries rupture or when there is significant turbulence due to narrowing of the vessel, it leads to the exposure of collagen and von Willebrand factor (vWF). This exposure triggers platelet adhesion and secretion, initiating the clotting cascade. Collagen and vWF act together as adhesive proteins that bind platelets to the site of vascular injury. They also activate the platelet to recruit other platlets.
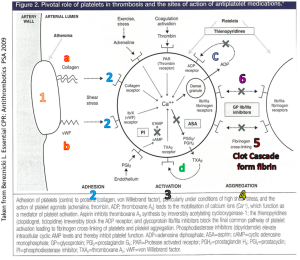
Role of Thromboxane A2
Once platelets adhere to the damaged vessel wall, they produce thromboxane A2 under the influence of the enzyme cyclooxygenase-1 (COX-1). Thromboxane A2 plays a pivotal role in platelet aggregation and causes vasoconstriction by inducing contraction of vascular and respiratory smooth muscles. In the context of angina, thromboxane A2 contributes to the narrowing of the coronary artery, further exacerbating the condition by increasing platelet aggregation and formation of a platelet plug. It also causes the release of factors that recruit other platelets to the area of damage.
Aspirin’s Mechanism
Aspirin is a widely used antiplatelet drug that functions as a non-specific COX enzyme inhibitor. By inhibiting COX-1, aspirin effectively reduces the production of thromboxane A2 in platelets. This inhibition decreases platelet aggregation and minimizes vasoconstriction, thereby reducing the risk of clot formation in narrowed coronary arteries. The therapeutic use of aspirin is particularly beneficial in secondary prevention to prevent further thrombotic events in patients with existing coronary artery disease.
Clopidogrel’s Mechanism
Clopidogrel, another key antiplatelet agent, is a P2Y12 receptor antagonist. It works by blocking the action of adenosine diphosphate (ADP) at the P2Y12 receptor on platelets. This inhibition prevents ADP from activating platelets, thereby reducing their ability to aggregate. Clopidogrel is often used as an alternative to aspirin, especially in patients who are intolerant to aspirin or require additional antiplatelet therapy.
Both aspirin and clopidogrel play crucial roles in the secondary prevention of atherosclerotic cardiovascular events by targeting different mechanisms in the platelet activation and aggregation pathways. Aspirin inhibits COX-1 to reduce thromboxane A2 production, while clopidogrel blocks ADP-induced platelet activation. Understanding these mechanisms helps in effectively managing patients at risk of recurrent cardiovascular events.
📺 Watch the vodcast on the mechanism of action of antiplatelet drugs for secondary prevention in angina. (7:05 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
