3.9 Management of Stable Angina – Drug Management
John Smithson
Medical management of stable angina
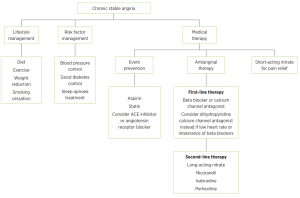
There are three main components to the medical management of angina:
Prevention of angina by reducing the chance of worsening of the atherosclerotic occlusion using antiplatelet drug therapy (low dose aspirin or clopidogrel) and stabilizing and reducing the size of coronary artery plaques by lowering circulating blood cholesterol levels (statins). Blood pressure should also be managed using an angiotensin converting enzyme (ACE) inhibitor or an Angiotensin-2 receptor blocker (A2RB).
Acute symptom relief via the use of short acting sub-lingual nitrates such as nitrolingual spray.
📺 Watch the vodcast on the Management of acute angina with a nitrate. (3:13 minutes)
and Antianginal therapy with
- First line – beta blockers such as metoprolol or atenolol,
- Second line – calcium channel blockers (dihydropyridine and non-dihydropyridine CCBs)
- A combination of the above (noting interactions) or the addition of long-acting nitrate therapy
- Use of other last-line agents such as nicorandil, ivabradine or perhexiline.
Antianginal therapy
Managing stable angina over the long term requires careful medication management to balance oxygen supply and demand, thereby alleviating symptoms and preventing progression of the disease. Beta-blockers and calcium channel blockers are central to this strategy.
The figure below describes the comprehensive management of stable angina.
Beta-Blockers: First-line therapy for stable angina typically involves beta-blockers such as metoprolol or atenolol. These medications work by reducing the heart rate and the force of contraction, which lowers the heart’s oxygen demand. This is particularly beneficial during episodes of angina, as it helps prevent the imbalance between oxygen supply and demand that causes chest pain. Beta-blockers are cardioselective, meaning they specifically target beta-1 receptors in the heart, which helps reduce the risk of adverse effects on other parts of the body. Metoprolol and atenolol are preferred due to their selectivity and effectiveness in managing chronic angina. They not only help in controlling symptoms but also have proven benefits in reducing the risk of heart attacks and improving overall cardiovascular outcomes.
Calcium Channel Blockers: When beta-blockers are not tolerated, are contraindicated, or if additional symptom control is needed, calcium channel blockers (CCBs) become an important part of the treatment regimen. These drugs are categorized into two main groups: dihydropyridine and non-dihydropyridine CCBs.
- Non-Dihydropyridine CCBs: Drugs such as diltiazem and verapamil fall into this category. They work by reducing heart rate and myocardial contractility, which helps decrease oxygen demand. Additionally, they have a vasodilatory effect that reduces the workload on the heart by lowering blood pressure and decreasing the heart’s oxygen requirements. Non-dihydropyridine CCBs are particularly useful in patients who cannot tolerate beta-blockers or when additional control of heart rate is needed.
- Dihydropyridine CCBs: Medications like amlodipine and modified-release nifedipine belong to this group. They primarily work by relaxing blood vessels, which lowers blood pressure and reduces the heart’s workload. While they are effective in managing angina by improving coronary blood flow, they are generally used in combination with other antianginal agents, such as beta-blockers, for a more comprehensive approach to symptom control.
Combination Therapy: In cases where monotherapy with beta-blockers or calcium channel blockers is insufficient, a combination of these drugs may be employed. For instance, combining a beta-blocker with a dihydropyridine CCB can provide enhanced control of angina symptoms while minimizing the risk of adverse effects associated with higher doses of a single class of medication. It’s crucial to monitor for potential interactions and side effects, such as hypotension or bradycardia, especially when combining medications.
Long-Acting Nitrates: If angina remains inadequately controlled despite the use of beta-blockers and calcium channel blockers, long-acting nitrates like transdermal glyceryl trinitrate or modified-release isosorbide mononitrate may be added. These agents help to further alleviate symptoms by dilating blood vessels and reducing myocardial oxygen demand.
Effective long-term management of stable angina involves a tailored approach using beta-blockers and calcium channel blockers, either alone or in combination, to address the specific needs of the patient. By carefully adjusting these medications, healthcare providers can help manage symptoms, reduce the risk of cardiovascular events, and improve the overall quality of life for individuals with stable angina.
📺 Watch the vodcast on the Medical Management of Stable Angina. (17:37 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
