6.4 GLP-1 RA, T2DM Treatment Algorithm and Conclusion
GLP-1 RA, T2DM Treatment Algorithm and Conclusion
GLP-1 Receptor Agonists (GLP-1RA)
As we already know, GLP-1 has several beneficial effects in T2DM. GLP-1 receptor agonists imitate GLP-1 and bind to GLP-1 receptors (G-protein coupled) producing the physiological effects of endogenous GLP-1 including increased glucose dependent insulin release and delayed gastric emptying.
![GLP-1 Receptor Agonists bind to the G protein coupled GLP-1 receptor which activates cAMP ultimately leading to increased insulin release. Importantly, this requires glucose fuelled ATP formation to close ATP sensitive potassium channels (glucose dependent). Source: Williams J. Pancreapedia. Available online https://pancreapedia.org/molecules/glp-1-version-10 [accessed Aug 2024]](https://jcu.pressbooks.pub/app/uploads/sites/81/2024/06/38-GLP1-Insulin.jpg)
In the last few years, GLP-1 RAs have become widely used for both the management of T2DM and for weight loss. There has been a global shortage of GLP-1 RAs due to demand however this appears to be slowly resolving. The following medications in this class are available in Australia (pending supply shortages):
- Semaglutide
- Dulaglutide
- Liraglutide – nonPBS
Wegovy (semaglutide) and Saxenda (liraglutide) are the TGA approved weight loss formulations of these agents.
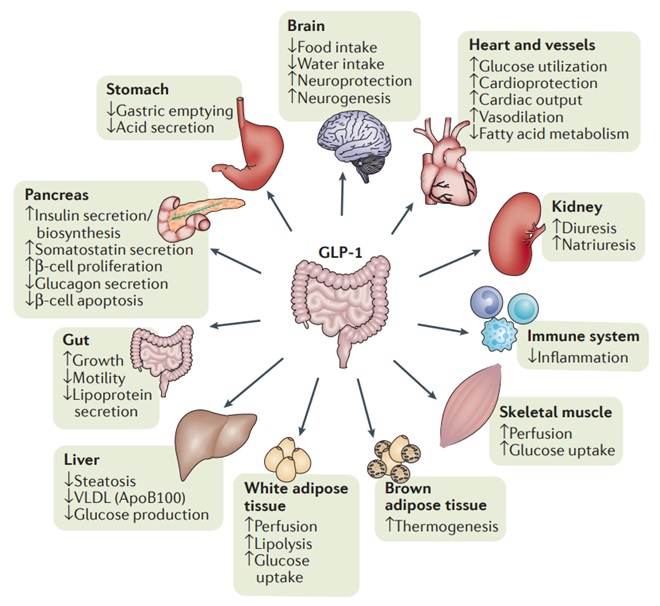
GLP-1RAs have shown several benefits compared to DPP-4 inhibitors. They reduce the risk of cardiovascular events, possess some reno-protective properties, produce weight loss (2-5kg) and produce larger HbA1c reductions (almost as good as insulin) – all very positive things for most T2DM patients.
For these reasons, GLP-1 RAs (when stock is available) are preferred to DPP-4 inhibitors. GLP-1RAs sit alongside SGLT-2 inhibitors as the standard add-on therapy to metformin in clinical guidelines.
The primary disadvantage is that currently in Australia, all GLP-1 RAs are only available as subcutaneous injections. This can impact on adherence for some patients and poses other challenges for some patients.
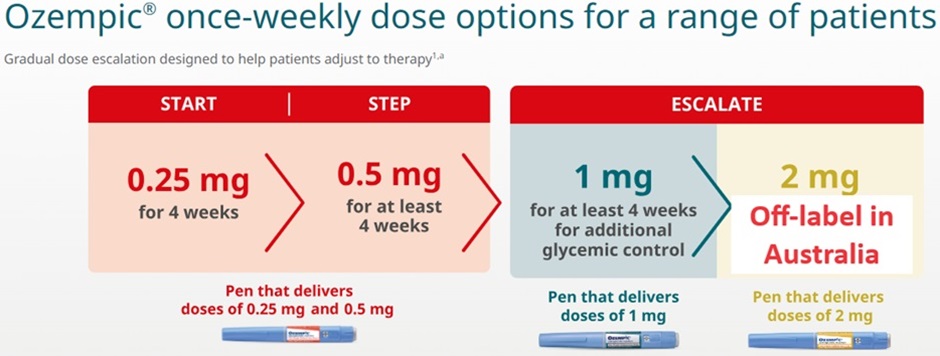
Semaglutide and liraglutide doses are titrated to the target dose over the course of several weeks to minimise gastrointestinal side effects.
Side effects of GLP-1RA
The most prominent side effect with GLP-1 RAs is nausea and gastrointestinal upset likely related to delayed gastric emptying. This can be severe and lead patients to discontinue treatment.
Clinical trials using semaglutide showed an increased risk of retinopathy complications. Patients with retinopathy should be closely monitored if commenced on GLP-1 RAs.
Most patients will also experience a small increase in heart rate of 2-3 beats per minute but this does not appear clinically significant. Other side effects are broadly similar to DPP4 inhibitors including precautions relating to pancreatitis.
GLP-1RAs cause a significant reduction in gastric emptying. There is emerging evidence that this can increase the risk of aspiration during surgery if patients are not adequately fasted prior to general anaesthesia.
Check your understanding:
- More effective than DPP-4 inhibitors.
- Reduce the risk of cardiovascular events and renal disease.
- Produce beneficial weight loss and relatively large HbA1c improvements (compared to other non-insulin agents).
- Nausea and GI upset is a significant side effect that is often managed with dose titration.
- Becoming the standard add-on therapy to metformin (like SGLT-2 inhibitors).
Watch this video – GLP-1 Receptor Agonists ‘glutide’
Treatment algorithms for T2DM
Due to the fact many patients with T2DM are asymptomatic, screening plays an important role in diagnosis and early intervention to prevent the complications of diabetes. The AUSDRISK tool can be used to help identify the risk of a patient developing T2DM over the next 5 years.
Depending on the patient’s diabetes risk, HbA1c or BGL screening should be undertaken at appropriate intervals. The box below shows the thresholds for diagnosis of T2DM in asymptomatic patients.
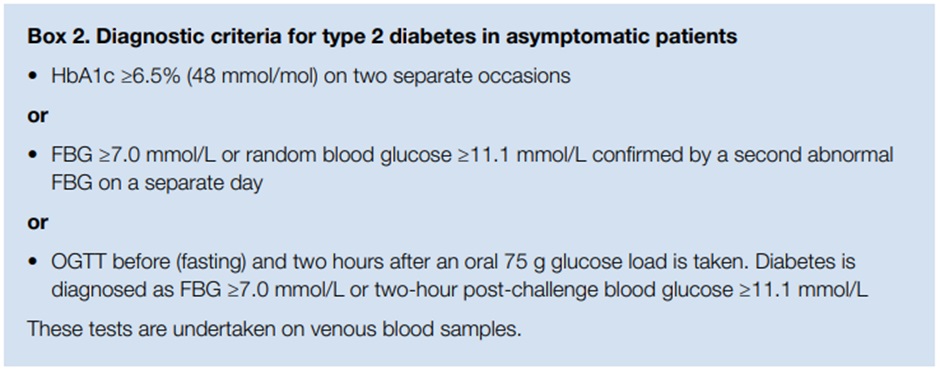
Patients with symptoms suggestive of diabetes, only require a single BGL or HbA1c reading above threshold.
Non-pharmacological advice including healthy lifestyle measures, healthy diet, exercise recommendations and weight management should be provided to all patients.
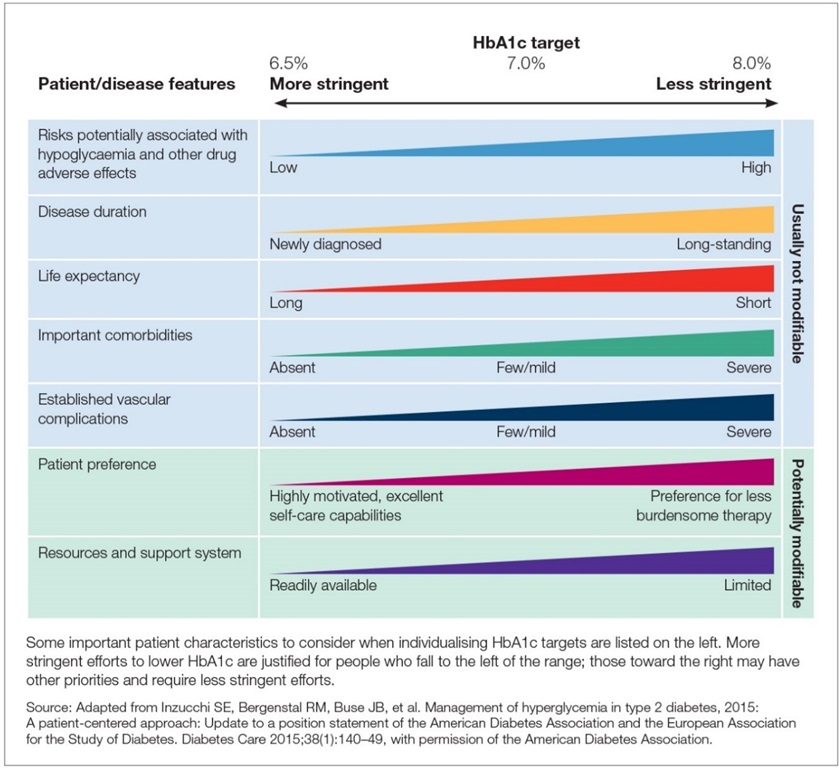
Each patient should have a target HbA1c established. For most patients this will be HbA1c <7% however the target should be individualised for each patient.
Some patients may benefit from tighter control especially if they are diagnosed early and have not yet developed any vascular complications of diabetes and have a low risk of hypoglycaemia. Alternatively, patients with longstanding diabetes, established vascular disease, limited life-expectancy or high risk of hypoglycaemia are likely to require a higher HbA1c target. Patient preference, access to care, costs and comorbidities should all be considered when determining a patient’s HbA1c target.
![Source: Management of type 2 diabetes: A handbook for general practice. [accessed Aug 2024]](https://jcu.pressbooks.pub/app/uploads/sites/81/2024/06/43-HbA1c-Subgroups.jpg)
All patients with T2DM should be commenced on metformin (unless contraindicated/unable to tolerate) in addition to lifestyle interventions.
Patients who have particularly high HbA1c levels at diagnosis and those with established cardiovascular or renal complications may also be commenced on an SGLT-2 inhibitor or GLP-1RA at diagnosis (PBS rules may limit this).
After 3 months of treatment, HbA1c should be re-tested, and treatment changes made based on this result. Treatment should be escalated if not at target. Due to their proven cardiovascular and renal benefits, SGLT-2 inhibitors and GLP-1 RAs are recommended to be added to metformin monotherapy if HbA1c is not yet at target.
Many patients will require metformin + SGLT-2 inhibitor or GLP-1 RA + insulin to adequately control their HbA1c (PBS currently precludes combined use of SGLT-2 inhibitors and GLP-1 RAs).
DPP-4 inhibitors are mostly used when GLP-1 RAs are inappropriate, unavailable, or precluded by PBS restrictions. DPP-4 inhibitors are not combined with GLP-1 RAs.
Insulin is commonly added for patients where a significant HbA1c reduction is desired and in those who are not achieving their target despite 2-3 other therapies.
Sulfonylureas are an alternative agent when other therapies are not tolerated (or have inadequate response). Sulfonylureas lack cardiovascular benefit and may worsen cardiovascular outcomes if used instead of an agent with proven benefits. Therefore, they are now largely reserved for use when the other alternatives are inappropriate.
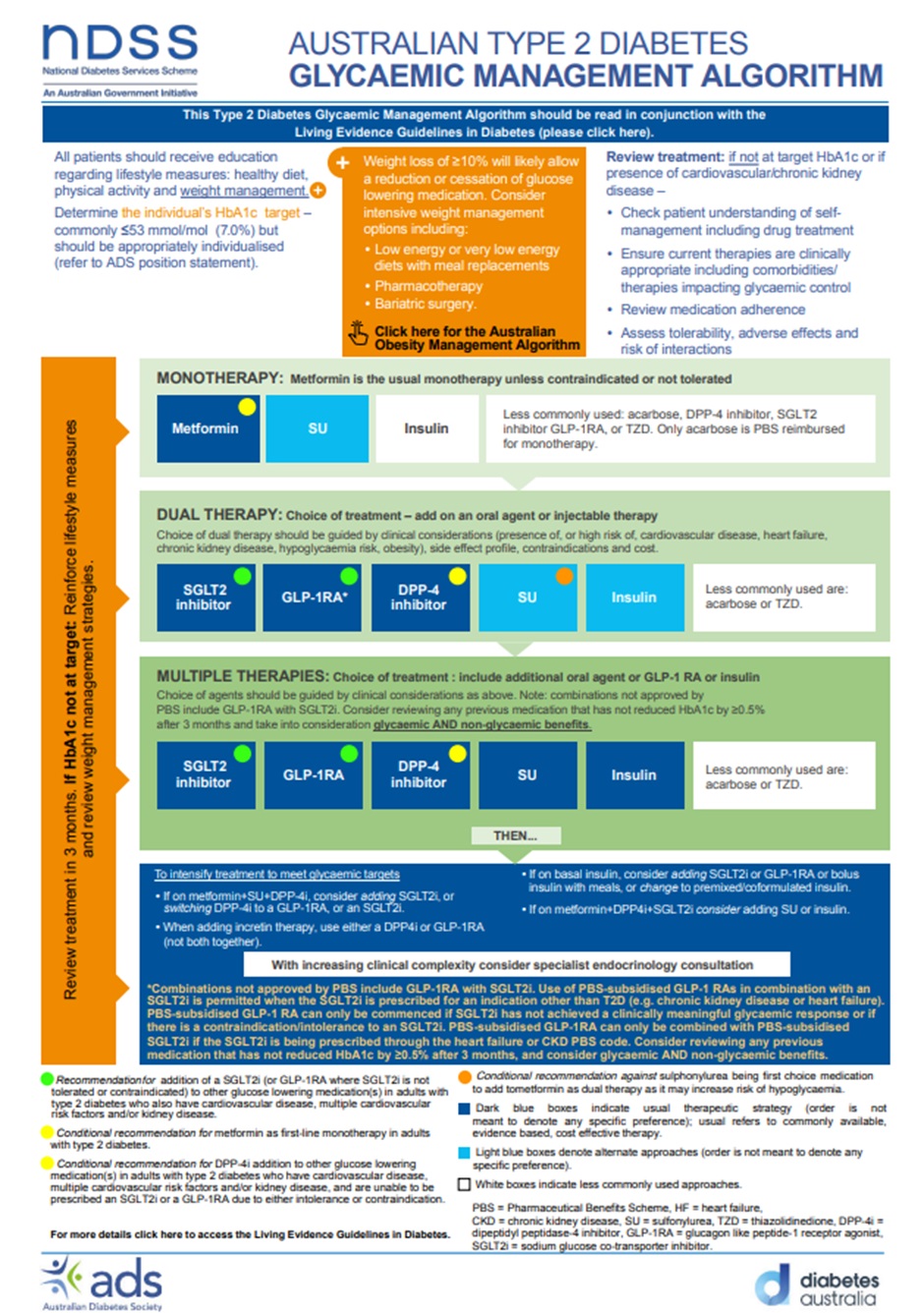
Explore and familiarise yourself with the NDSS Australian T2DM Glycaemic Management Algorithm and the eTG Algorithm for antihyperglycaemic treatment for adults with type 2 diabetes.
Check your understanding:
Summary
- Diabetes risk assessment and screening is important to identify diabetes in patients.
- Lifestyle interventions and metformin should be provided to all patients.
- Preferentially use SGLT-2 inhibitors or GLP-1 RAs as add-on therapy to metformin due to their cardiac and renal benefits.
- Choice between SGLT-2 inhibitors and GLP-1 RAs is largely based on patient comorbidities and preferences.
- Insulin can be used at any stage but usually only when large HbA1c reductions are desired or inadequate response to 2-3 other therapies.
- PBS funding arrangements can limit the choice/combination of therapy.
Watch this video – Treatment Overview
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
