8.2 Pharmacology of Gastric Acid Suppression
Mechanisms of gastric acid secretion & the pharmacological agents for gastric acid suppression
In this first part of the gastrointestinal pharmacology series, we will look at the mechanisms of gastric acid production, common gastric acid disorders and the pharmacotherapy of dyspepsia, GORD and PUD. The gastrointestinal drugs we will learn about include H2 receptor antagonists and proton pump inhibitors.
Learning Outcomes
By the end of this module, students should be able to demonstrate and apply knowledge of:
- Mechanisms of gastric acid production
- Common gastric acid disorders- dyspepsia, GORD and PUD
- Pharmacological agents for acid suppression- H2 antagonists, proton pump inhibitors.
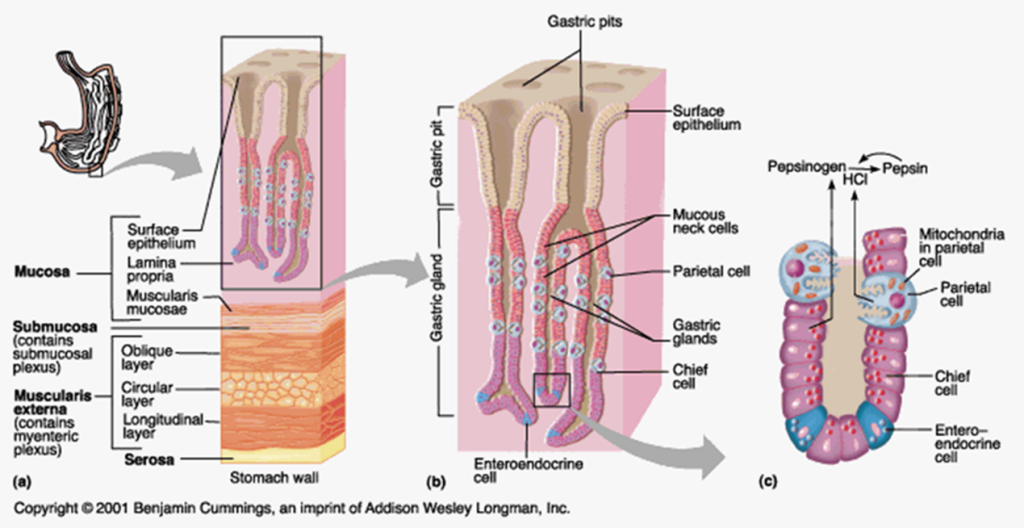
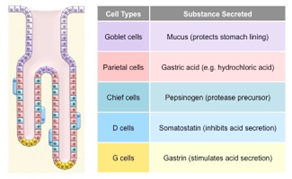
The stomach produces enzymes and acid to aid digestion
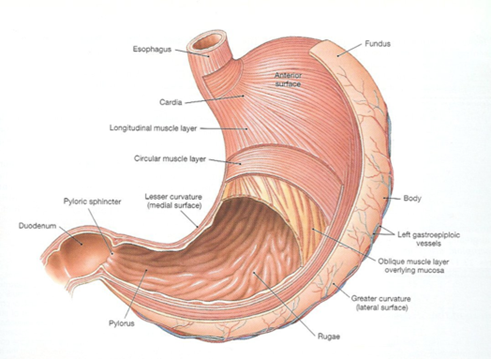
The stomach has four regions. It is divided into the fundic, cardiac, body, and pyloric regions.
The stomach is the site of common pathologies
Dyspepsia: Chronic or recurrent pain, burning or discomfort centred in the upper abdomen.
GORD: Gastro-oesophageal reflux disease (GORD) is present if symptoms are frequent (2 or more episodes per week) or severe enough to significantly impair quality of life, or if complications of gastro-oesophageal reflux are present.
Peptic Ulcer Disease: Peptic ulcer disease (PUD) includes gastric and duodenal ulcers. PUD is mostly caused by Helicobacter pylori (H. pylori) infection or nonsteroidal anti-inflammatory drug (NSAID) use. In a small number of patients with peptic ulcer disease, neither risk factor is present.
📚 Read/Explore
Read: “Gastric secretions” and “Drugs that neutralise or inhibit gastric acid secretion” in Chapter 16 Drugs Affecting the Upper and Lower Gastrointestinal Tract (pages 325-332) in Pharmacology for Health Professionals 6th Ed.
📺 Watch the following lecture on the mechanisms of gastric acid secretion (19 minutes)
Treatment options – Dyspepsia, GORD, PUD
The treatment of disorders relating to gastric acid secretion can be targeted in several ways. The drugs that are used act to inhibit the action of secretagogues. This may be by any of the following mechanisms:
- Neutralizing gastric acid: the use of basic salts to increase PH: Antacids
- Forming a protective barrier, coating ulcers and limiting acid diffusion: Cyto-protective agents (Sucralfate, bismuth)
- Increasing protective mucus, bicarbonate and prostaglandin: Cyto-protective agents and Misoprostol
- Reducing gastric acid secretion: H2 receptor antagonists, PPIs, Misoprostol
Our main focus will be the mechanisms of action of H2 receptor antagonists and Proton Pump Inhibitors.
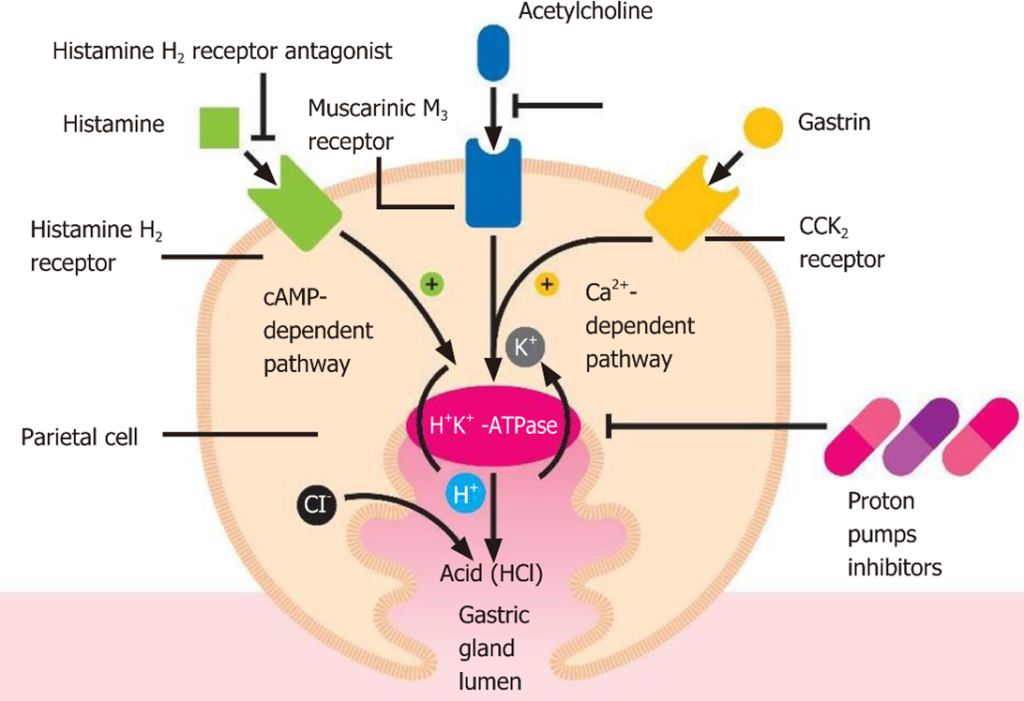
- H2 receptor antagonists block the effects of Histamine
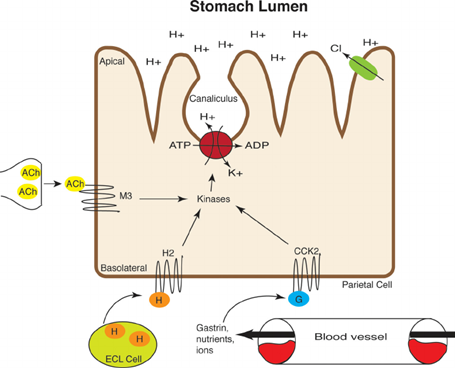
- PPIs inhibit proton pump activation by mediators Histamine, ACH and Gastrin
Other treatment considerations include testing for and treating H.pylori; cessation of causative agents (eg: NSAIDs) and several lifestyle modifications.
1. H2 Receptor Antagonists
H2 receptor antagonists competitively and reversibly block endogenous histamine from binding to the H2 receptor on parietal cells. Consequently, there is a reduction in cAMP dependent protein kinase which is involved in the transport of H+/K+ ATPase from the cytoplasm to the cell membrane. H2 receptor antagonists reduce gastric acid production by ~70% and are used to treat dyspepsia, GORD and PUD. Their duration of action is 12 hours, meaning dosing is twice daily. The drug names end in the suffix -tidine and examples include famotidine and nizatidine.
2. Proton Pump Inhibitors
Proton pump inhibitors irreversibly bind to and inactivate the H+/K+ ATPase enzyme. Both basal and meal-stimulated gastric acid secretion is reduced. PPIs are the most potent inhibitors of acid secretion (reduced by ~85%) as they affect the terminal step in the acid secretory pathway.
Degrade rapidly in low pH (the stomach) so enteric coating allows absorption from the small intestine into the blood then the drug accumulates in the parietal cell canaliculi where it is activated to the metabolite- a thiophilic sulphenamide. The active metabolite interacts covalently with the H+/K+ ATPase pump involved in H+ ion transport.
PPIs have a long duration of action and a single daily dose of PPI can affect acid secretion for 2-3 days. This is because they bind irreversibly therefore a new H+/K+ ATPase must be synthesised.
The drug names of PPIs end in the suffix -razole and examples include esomeprazole, lansoprazole, omeprazole, pantoprazole and rabeprazole.
PPIs are generally well tolerated and adverse effects include headache and diarrhoea, hypomagnesaemia, reduced vitamin B12 absorption and less commonly, interstitial nephritis.
Triple Therapy for Helicobacter pylori
H.pylori infection is prevalent in about 30% of adult Australians. H.pylori is a causal agent in the development of numerous conditions- duodenal and gastric ulcers, chronic gastritis and gastric cancer
It is diagnosed from a urea breath test. Diagnosis by urea breath test: patient given 13C-urea orally, the urease in H.pylori metabolises it to release 13CO2 and NH3, the amount of CO2 in the expired air is measure to confirm diagnosis. Diagnosis may also involve antibody testing, endoscopy or biopsy
Eradication of H.pylori involves triple therapy with two antibacterials and a PPI as the first line of treatment. Usually, this is amoxicillin + clarithromycin + PPI for 7- 14 days. In people who are hypersensitive to penicillin, amoxicillin is replaced by metronidazole.
The image below shows the contents of Nexium HP7 and was sourced from the NPS Medicinewise website. It can be found at https://www.nps.org.au/medicine-finder/nexium-hp7-combination-pack
Let’s compare the difference in effectiveness of H2 receptor antagonists and PPIs. The image below shows the effects of H2 receptor antagonists and proton pump inhibitors on the acid secretion pathway in parietal cells. H2 receptor antagonists only block 1 of 3 pathways in which the production of gastric acid is stimulated. PPIs block the terminal step in the acid secretory pathway, making them more effective.
📚 Read/Explore
Read: “Drugs used to inhibit or neutralise gastric acid secretion” in Chapter 31 The Gastrointestinal Tract (pages 397-399) in Rang and Dale’s Pharmacology 9th Ed.
📺 Watch the following lecture on the pharmacological agents for gastric acid suppression (18 minutes)
Lecture Notes:
Summary
- Acetylcholine, histamine and gastrin bind to their respective receptors on the parietal cells to stimulate gastric acid production.
- Common pathologies associated with gastric acid include dyspepsia, GORD and PUD.
- H2 receptor antagonists block histamine from binding to the H2 receptor on the parietal cell and are able to inhibit some secretion of gastric acid.
- PPIs irreversibly bind to and inactive the proton pump and are able to inhibit almost all gastric acid secretion.
✍️Let’s do an activity
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.