8.3 Pharmacology of Nausea and Vomiting
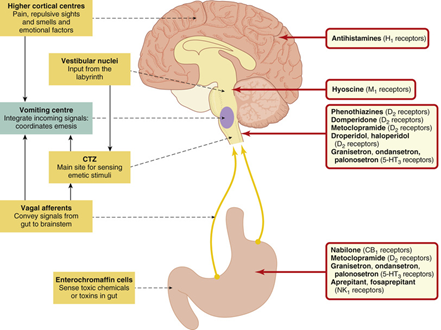
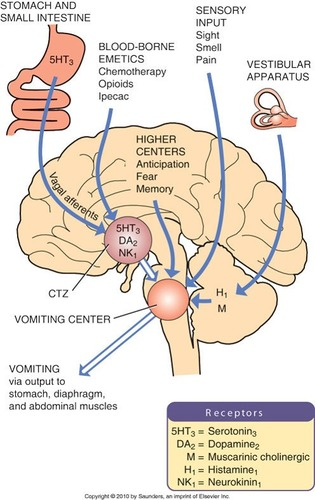
Mechanisms of emesis and the pharmacological agents for nausea and vomiting
In this part of the gastrointestinal pharmacology series, we will review the mechanisms of emesis and discuss the pharmacology of antiemetics.
Learning Outcomes
By the end of this module, students should be able to demonstrate and apply knowledge of:
- Mechanisms of emesis
- Pharmacology of antiemetic agents (for nausea and vomiting)- Anticholinergics/Antimuscarinics, H1 receptor antagonists/Sedating antihistamines, D2 receptor antagonists, 5-HT3 antagonists and NK1 receptor antagonists.
The mechanisms of emesis are complex
Emesis (vomiting) is the forceful expulsion of the contents of the stomach (and sometimes intestines) through the mouth. It can be a helpful, defensive response to toxic stimuli, but it is mostly very distressing. Persistent vomiting can lead to dehydration and electrolyte imbalances.
There are numerous potential causes of Vomiting
Common causes of vomiting include gastroenteritis, pregnancy, vertigo, surgery (post-operative nausea and vomiting) and drugs (drug-induced nausea and vomiting).
-Ingestion of toxin/bacteria (eg gastroenteritis) leads to stimulation of Serotonin or Substance P from ECC cells in gastric lining which impacts the CTZ and VC inducing emesis.
-Damage to the stomach lining/viscera (eg surgery) or mechanical stimulation in GIT (eg pressure or fullness) can lead to stimulation of Serotonin or Substance P from ECC cells in gastric lining which impacts the CTZ and VC inducing emesis
-Emetic agents (drugs) (eg cytotoxic agents used in chemotherapy, Ipecac, Levodopa, Digoxin, opioids, ergot alkaloids induce emesis via multiple mechanisms including ECC, CTZ, 5HT3, D2 receptor stimulation.
-Absorbed toxins can stimulate CTZ directly (outside the BBB)
The mechanisms of emesis are complex and involve many different neurotransmitters and pathways
Mechanisms involve:
- Chemoreceptor Trigger Zone (CTZ)
- Vomiting Centre
- Vestibular System
- Vagal/Visceral Afferents
The two main areas involved in the induction of emesis include the chemoreceptor trigger zone (CTZ) and the vomiting centre.
📚 Read/Explore
The Chemoreceptor Trigger Zone (CTZ) detects toxins in the blood and CSF
The CTZ is located in the area postrema, within the dorsal surface of the medulla oblongata, on the floor of the fourth ventricle of the brain. In the absence of the blood–brain barrier, the CTZ has access to and activation from toxins and chemicals. A variety of neurotransmitters and their receptors are important in the CTZ, including dopamine, adrenaline, 5-HT, acetylcholine, histamine, enkephalin and substance P.
The CTZ receives input from three different pathways:
- Direct stimulation – The CTZ is located outside of the blood brain barrier so it is stimulated directly by endogenous and exogenous substances in the blood. These include: mediators, hormones, toxins and bloodborne drugs.
- Vagal afferents – Cytotoxic drugs and other GI irritants stimulate the release of serotonin and substance P from enterochromaffin cells in the GIT and these bind to receptors in the CTZ.
- Vestibular Nuclei – Stimulation of the labyrinth in the inner ear leads to impulses passing along the vestibular nerve to the vestibular nuclei, to receptors in the CTZ.
The CTZ cannot induce the vomiting reflex itself but it does relay information to the vomiting centre via neurotransmitters such as acetylcholine, serotonin, histamine and dopamine.
The Vomiting Centre can induce the vomiting reflex
The vomiting centre of the brain refers to the groups of loosely organized neurons in the medulla oblongata that include the CTZ within the area postrema and the nucleus tractus solitarii. Neurotransmitter receptors found in the vomiting centre include muscarinic, opioid, cannabinoid, dopamine, serotonin, neurokinin-1 and a2 adrenoceptors.
The vomiting centre receives input from:
- CTZ
- Vagal afferents (enterochromaffin cells in the GIT) takes signal from GIT into the brain stem
- Vestibular system
- Higher brain centres in the cortex and thalamus in relation to sensory information such as pain, emotional factors, memory, bad smells, tastes and sights. (CNS).
The VC can induce emesis. Efferent impulses are sent from the vomiting centre to the upper GIT, diaphragm and abdominal muscles. The contraction of stomach muscles, the movement of stomach contents up the oesophagus, past the oesophageal sphincter and into the mouth results in vomiting. Accompanying symptoms of salivation, sweating, rapid breathing and cardiac dysrhythmias are mediated by the Sympathetic and Parasympathetic Nervous Systems (SNS and PNS).
📚 Read/Explore
📺 Watch: Physiology of Vomiting – Physiology of Vomiting – Vomiting reflex (NEW)
📺 Watch: The following lecture on mechanisms of emesis (14 minutes)
Now that you understand the neurotransmitters and pathways involved in the mechanisms of emesis, can you think of potential ways in which drugs could treat nausea and vomiting? Hint: The neurotransmitters and receptors involved are predominantly:
- Acetylcholine – M1 receptors
- Histamine – H1 receptors
- Dopamine – D2 receptors
- Serotonin (5-hydroxytryptamine) – 5HT3 receptors
- Substance P – NK1 receptors
The pharmacology of antiemetics is based on blocking the actions of neurotransmitters involved in the mechanisms of emesis
Antiemetics act by blocking neurotransmitters from binding to receptors in the CTZ, vomiting centre, cerebral cortex or the vestibular apparatus. Examples include antimuscarinics/anticholinergics, H1 receptor antagonists, D2 receptor antagonists, 5-HT3 antagonists and NK1 antagonists.
When aiming to treat or prevent nausea and vomiting, it is useful to think about what the source of the symptoms are, which mechanism of emesis is occurring and therefore which receptor/target is involved. This will allow for an appropriate selection of antiemetic agent to be used for treatment.
Antimuscarinics/Anticholinergics
- Examples include hyoscine hydrobromide.
- Competitive antagonist of the actions of Ach at muscarinic receptors
- Anticholinergic actions on M1 in the vestibular nuclei and possibly elsewhere.
- Used to prevent and treat vomiting associated with motion sickness.
- More effective if given before motion sickness develops (the first dose given 30min before travel).
- Hyoscine hydrobromide crosses the blood brain barrier, thus side effects such as dry mouth, dizziness and blurred vision may limit patient acceptance.
Sedating antihistamines
- Examples include promethazine, dimenhydrinate and cyclizine.
- Block H1 receptors in the CNS and possibly anticholinergic actions in the vestibular apparatus.
- Used to prevent and treat vomiting associated with motion sickness and morning sickness.
- Not very effective against substances that act directly on the CTZ.
- Anticholinergic side effects of sedating antihistamines such as dry mouth, dizziness, dry eyes, and blurred vision may limit use.
- Causes drowsiness and can lower seizure threshold.

D2 receptor antagonists
- Examples include prochlorperazine, droperidol, haloperidol, metoclopramide and domperidone.
- Used short term only as the risk of EPSE (movement disorders) increases with dose and length of treatment.
- Can cause hyperprolactinemia.
Prochlorperazine
- Blocks D2 receptors in the CTZ and also blocks histamine and muscarinic receptors.
- Used for nausea and vomiting caused by migraine, motion sickness, vertigo and viral gastroenteritis.
- Main side effects include sedation, dry mouth, constipation, blurred vision and EPSE.
- Avoid use in Parkinson’s disease as can worsen symptoms (Domperidone preferred)
Metoclopramide
- Blocks central D2 receptors in the CTZ and peripheral D2 receptors in the GIT.
- Exerts prokinetic activity (accelerates gastric emptying).
- Used for nausea and vomiting caused by migraine or acute gastroenteritis,
- Side effects include drowsiness, dizziness, headache and EPSE.
- AMH states maximum treatment length is 5 days.
- Avoid use in Parkinson’s disease as can worsen symptoms (Domperidone preferred)
Domperidone
- A dopamine antagonist (D2 and D3) that is hydrophyllic, therefore does not cross the blood–brain barrier and CNS effects are rare.
- Rarely causes EPSE and is the anti-emetic of choice in a patient with Parkinson’s disease.
- Exerts prokinetic activity (accelerates gastric emptying)

- Examples include ondansetron, granisetron, palonosetron and tropisetron.
- Block central 5-HT3 receptors in the CTZ and blocks peripheral 5-HT3 receptors on vagal nerve terminals.
- Used to prevent or treat nausea and vomiting associated with chemotherapy, radiation or surgery.
- Side effects include constipation, headache, dizziness.
NK1 antagonists
- Also known as substance P antagonists.
- Examples include aprepitant and fosaprepitant.
- Aprepitant blocks NK1 receptors in the CTZ and vomiting centre and possibly the GIT.
Used to treat nausea and vomiting associated with emetogenic chemotherapy and they are sometimes co-administrated with 5-HT3 antagonists and dexamethasone (a corticosteroid).
📺 Watch: Pharmacology of Vomiting Pharmacology – Antiemetics
—————————————————————————————————————————————————————–
📺 Watch: The following lecture on the pharmacological agents for nausea & vomiting (12 minutes)
 Lecture Notes
Lecture Notes
Summary
- The vomiting centre receives input from the CTZ, GIT and higher centres of the brain to stimulate emesis. The CTZ relays information to the vomiting centre about circulating toxins in the blood as well as information from the GIT and labyrinth.
- Neurotransmitters involved in mechanisms of emesis include acetylcholine, histamine, serotonin, dopamine and substance P. These bind to muscarinic, H1, 5-HT3, D2 and NK1 receptors, respectively.
- Clinically useful antiemetics include antimuscarinics, H1 receptor antagonists, D2 receptor antagonists, 5-HT3 antagonists and NK1 antagonists.
💡Learning Activity
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.