8.4 Pharmacology of Constipation and Diarrhoea
Pharmacological agents for the management of constipation and diarrhoea
In this part of the gastrointestinal pharmacology series, we will review the mechanisms of two disorders involving the lower GIT, constipation and diarrhoea. We will also focus on the pharmacology of laxatives and anti-diarrhoeals.
Two common disorders affecting the lower GIT are constipation and diarrhoea.
Learning Outcomes
By the end of this module, students should be able to demonstrate and apply knowledge of:
- Mechanisms of constipation and diarrhoea
- Pharmacology of drugs involved in the treatment of constipation- Bulk forming laxatives, Stimulant laxatives, Osmotic and saline laxatives, Stool softeners
- Pharmacology of drugs involved in the treatment of diarrhoea- Oral rehydration, Opioid agonists.
Constipation
- Defined as difficult faecal evacuation which can be associated with infrequent bowel movements (< 3 times per week), straining, sensation of anorectal obstruction or feeling of incomplete evacuation.
- Causes include neurogenic (eg spinal cord injury), non-neurogenic (eg hypothyroidism or pregnancy), irritable bowel syndrome, drugs (eg verapamil or amitriptyline), stress and dietary factors (eg lack of fibre or reduced fluid intake).
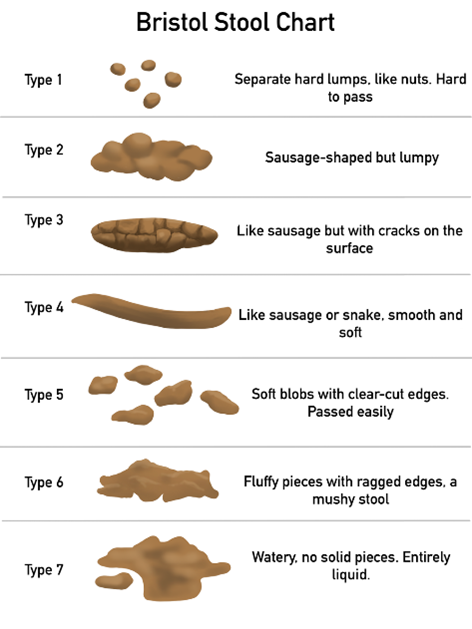
- The Bristol Stool type 1 and 2 are mostly consistent with constipation.
Non-pharmacological measures and laxatives treat constipation
Diet and lifestyle measures
Adequate dietary fibre intake, adequate fluid intake, increasing activity/exercise, immediately responding to the urge to defecate and using the toilet after meals.
Laxatives – oral (liquid, tablets) or rectal (suppositories, enemas) dosage forms
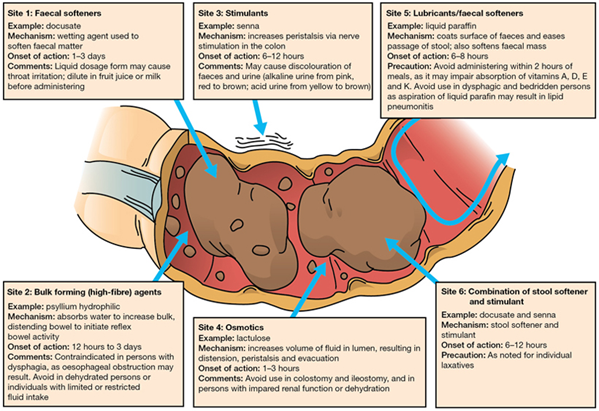
Bulk Forming
- Examples include psyllium husk and bran.
- Absorb water and provide a bulky, hydrated mass in the gut lumen promoting peristalsis and improve faecal consistency.
- Not broken down by the normal digestive process.
- Need to be administered with sufficient fluid.
Stimulant
- Examples include senna and bisacodyl.
- Promotes accumulation of water and electrolytes and stimulate nerve endings to increase intestinal motility.
- Primary effect on small and large intestines- cause cramping
Osmotic and saline laxatives
- Examples include lactulose, macrogol, polyethylene glycols (PEGs), glycerol, sorbitol, mannitol and saline laxatives.
- Osmotic laxatives produce an osmotic load and increase the volume of fluid in the lumen, accelerating the transfer of gut contents, resulting in peristalsis and defecation.
- Saline laxatives (eg Epsom salts, magnesium or sodium salts) increase salt in the colon leading to water retention and increased water content in the faeces by osmosis.
- Can cause electrolyte disturbances.
- Rectal preparations in this class include glycerol suppositories (osmotic, lubricant effects and local irritation to promote peristalsis)
- Also, oral powders for bowel evacuation prior to gastrointestinal procedures eg: Glycoprep-C, Colonlytely
Softeners
- Examples include docusate and poloxamer.
- Surface active compounds that act in the GIT.
- Facilitate the mixing of water and fatty substances in the faecal mass.
- Wetting agents to produce softer faeces.
Other Pharmacological agents
- Methylnaltrexone – for opioid induced constipation. Peripherally acting competitive mu opioid receptor antagonist; blocks the constipating effects of opioids in the GIT.
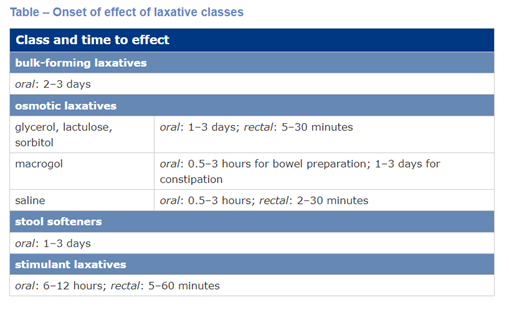
Rectally administered laxatives typically have a faster onset of action. Suppositories and enemas are used when oral laxatives are not effective, unsuitable or rapid relief is required.
The table below is from the AMH and indicates the onset of effect of the different laxative classes.
📚 Read/Explore
Diarrhoea
- Increased passage of semi-liquid or liquid stools.
- Passage of 3 or more loose stools per day or more frequent than normal for the individual
- Caused by infections, drugs (eg NSAIDs or magnesium), foods, post-surgical issues, inflammation in the GIT and psychological factors (eg anxiety).
- Bristol Stool type 6 and 7 are most consistent with diarrhoea.
The causes of diarrhoea are varied
Diarrhoea may be due to decreased absorption by the small and large intestine, accumulation of non-resorbable solutes or excessive secretion in the small intestine and colon.
- Malabsorption/Decreased absorption time- may be due to resection of the small or large intestine
- Osmotic- water retention in the bowel due to the presence of unabsorbable material
- Secretory- more secretion of water and electrolytes into the bowel than is absorbed
- Inflammatory- inflammation or ulceration of the mucosal layer due to disease (may be blood, plasma etc in the faeces)
- Drug induced- drugs or toxins causing stomach upset and diarrhoea
Electrolyte rehydration salts and opioid agonists treat diarrhoea
Electrolyte rehydration
- Fluid and salt replacement are essential
- Oral rehydration with isotonic solutions of NaCl plus glucose is first line.
- The presence of glucose enhances Na reabsorption and water uptake.
Opioid agonists
- Examples include loperamide and diphenoxylate.
- Opioid agonists which slow GI motility
- Activate mu opioid receptors on intestinal smooth muscles, resulting in a reduction in secretions and inhibition of propulsive movements in the gut.
Loperamide
- Is the agent of choice.
- Has a relatively selective action on the GIT
- Affects intestinal motility, has antisecretory effects and decreases the passage of faeces.
- More potent than morphine but does not cross the BBB, reducing likelihood of CNS effects.
Diphenoxylate
- Also lacks morphine-like activity in the CNS but large doses produce typical opioid-like effects.
- Is available as an S3 product in combination with atropine (a muscarinic antagonist)
- The role of atropine is to limit drug diversion (causes dry mouth, blurred vision,urinary retention)
Other treatments may include antimicrobials to treat an underlying infection responsible for the diarrhoea.
📚 Read/Explore
📺 Watch the following lecture on pharmacological agents for the management of constipation and diarrhoea (23 minutes)
 Lecture Notes
Lecture Notes
Summary for Laxatives and Anti-diarrhoeals
- Intermittent constipation is best treated with adequate fluid intake, a high fibre diet and regular exercise. Pharmacotherapy of constipation includes bulk forming, osmotic and stimulate laxatives as well as stool softeners.
- Oral rehydration salts are the mainstay of treatment for diarrhoea but the short-term, occasional use of opioid agonists such as loperamide or diphenoxylate can be helpful in social situations.
💡Learning Activity
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.