Developing Person-Centred Care Plans through Clinical Reasoning
Penelope Coogan; Leisa Sanderson; and Tracey Gooding
Learning Outcomes
In this chapter, you will learn how to:
- Define and differentiate the concepts of critical thinking, clinical reasoning and clinical judgement and how they interconnect in nursing practice
- Outline the key steps in clinical decision-making to effectively plan and deliver care
- Analyse patient care needs and prioritise interventions using critical thinking and clinical reasoning skills
- Utilise structured frameworks to develop individualised, comprehensive, and person-centred care plans.
Introduction
In nursing, the ability to think critically, reason effectively, and exercise sound clinical judgement is essential for providing safe, high-quality, and individualised care. This chapter focuses on building these core skills by exploring the concepts of critical thinking, clinical reasoning, and clinical judgement, and their vital role in the clinical decision-making process to plan and deliver care. In this chapter, you will learn to navigate the key steps in clinical decision-making, from assessing patient needs and analysing data, to planning and prioritising care. By utilising structured frameworks such as the Care Planning Process and the Clinical Reasoning Cycle, this chapter will guide you in developing individualised, person-centred care plans that address the unique needs of each patient.
Critical Thinking, Clinical Reasoning and Clinical Judgement

Critical Thinking
To make sound clinical decisions and provide safe, effective and quality patient care, nurses require critical thinking skills (Reji & Sushma, 2022; Willers et al., 2021). Critical thinking is an intellectual process used to analyse and interpret situations, enabling problem-solving and sound decision-making (DeLaune et al., 2020). According to DeLaune et al. (2020), it requires intellectual autonomy, evaluation of evidence, and the ability to see the bigger picture. Nurses use critical thinking to make decisions when providing care to patients. Making decisions as a critical thinker involves recognising the issue, collecting and assessing pertinent information, and developing possible solutions. In order to make a decision, an evaluation of these potential solutions ensues before choosing the most effective solution through clinical reasoning and evidence-based analysis. So, rather than just following orders without question, nurses should critique every situation to ensure the accuracy of all available information. Care plans should be developed around the specific needs of the patient, using the most current clinical practice guidelines and research.
According to the literature, “critical thinkers” possess certain attitudes that cultivate rational thinking and decision-making including, (from Gupta & Upshur, 2012; Papp et al., 2014; Scheffer & Rubenfeld, 2000):
Clinical Reasoning
Clinical reasoning is a subset of critical thinking that is applied specifically to patient care and forms the basis of clinical decision-making (Tollefson & Hillman, 2022). It can be defined as “a complex cognitive process that uses formal and informal thinking strategies to gather and analyse patient information, evaluate the significance of this information, and weigh alternative actions” (Klenke-Borgmann, 2020). To make sound judgements about patient care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action (Powers et al., 2020). The ability to clinically reason develops over time and is based on knowledge and experience.
Griffits et al. (2023) describe clinical reasoning as a dynamic and non-linear process that integrates critical thinking, specialised knowledge, and practical experience. This approach helps nurses understand clinical situations, make informed judgements, implement and assess interventions, and manage and reflect on patient care effectively. The process of clinical reasoning involves (Dickison et al., 2019; Tanner, 2006):
Inductive and deductive reasoning are essential critical thinking skills that enable nurses to apply clinical judgement effectively when developing plans of care for patients.
|
Inductive reasoning is a cognitive process that uses facts or observations to identify patterns and draw conclusions. In nursing, this involves collecting cues, making generalisations, and creating hypotheses based on specific information or incidents in the environment. Cues, which are pieces of data gathered by the nurse through objective and subjective means, are examined for trends or patterns to hint at possible problems or conditions. By looking for patterns or trends within the cues, generalisations are formed. This thought process, similar to sorting pieces of a jigsaw puzzle into shapes or patterns, helps to make the whole picture clearer. From the generalisations made, the nurse creates a hypothesis regarding a patient problem. The hypothesis is a proposed explanation for a situation, attempting to explain the “why” behind the problem. Once this “why” is identified, a solution can begin to be explored. This type of cognitive process is a key aspect of problem identification and problem-solving. It is important to note that conclusions drawn from inductive reasoning are not guaranteed but are likely based on the evidence gathered. Errors can occur if not all information is collected. Nurses can improve their inductive reasoning skills by searching for as much evidence as possible and paying close attention to details in their surroundings. This includes paying close attention to the patient and the environment, both physical and social. The nurse should work like a detective, looking for all possible cues to either rule out or support the ideas that are forming. Once all appropriate cues have been gathered, it is easier to determine the cause of a problem and therefore solve it. Example: A nurse assesses a patient and finds the surgical incision site is red, warm, and tender to the touch. Recognising these cues as a pattern of signs of infection, the nurse hypothesises that the incision has become infected. The medical staff is notified of the patient’s change in condition, and a new prescription for an antibiotic is received. This is an example of inductive reasoning in nursing practice.
|
|
|
Deductive reasoning differs from inductive reasoning in that it involves reasoning from a general premise to a specific conclusion, rather than from a set of observations or facts (Berman et al., 2021). Also known as “top-down thinking,” deductive reasoning uses a general standard or rule to create a strategy. It relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. This premise is used to reach a specific, logical conclusion. For example, nurses use standards set by the ACSQHC, the Nursing and Midwifery Board of Australia, professional organisations, and their employers to make decisions about patient care and solve problems. Example: Based on research findings, hospital leaders determine that patients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by eliminating overhead paging, promoting low-speaking voices among staff, and reducing hallway lighting. Nurses further implement this policy by organising patient care to promote periods of uninterrupted rest at night. This is an example of deductive reasoning because the intervention is applied to all patients, regardless of whether they have difficulty sleeping or not.
|
Clinical Judgement
Clinical judgement is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. The concept of clinical judgement can be defined as a reflective and reasoning process through which nurses integrate all available data, drawing upon a comprehensive knowledge base including theoretical understandings and practical experiences (Connor et al., 2023). The process involves critically analysing patient information, recognising patterns, building therapeutic relationships, and applying a clinical reasoning process to reach informed clinical decisions. Effective clinical judgement is essential for ensuring safe and quality patient care in increasingly complex healthcare environments (Connor et al., 2023). After conducting a concept analysis of sound clinical judgement, Manetti (2019) defined it as,
a cognitive process in which the nurse forms a holistic assessment of a patient situation. Critical thinking, clinical reasoning, practical wisdom, and intuition are used in the decision-making process that ensues. Through careful deliberation, the nurse chooses among alternative actions in light of anticipated outcomes in the best interest of the patient. The nurse reflects on and monitors the patient’s responses and modifies actions accordingly. Afterward, further reflection empowers nurse with the improved judgment for future situations. (p. 106)
The following provides examples of clinical judgement in action.
Common Cognitive Biases that can Influence Decision-making
In nursing practice, several cognitive biases and assumptions can impact decision-making and cause errors in patient care. Nurses play a critical role in identifying and overcoming these biases. Understanding, recognising and addressing these biases can help develop critical thinking skills, improve patient decision-making and ensure quality, safe and effective nursing practice (Jala et al., 2023; Thompson et al., 2023). Click on the tabs below to discover the common cognitive biases and their meaning (Levett-Jones, 2023).
There are several strategies that can minimise the risk of cognitive bias in clinical decision-making including:
- Systematic approach to assessment and decision making: Using a systematic approach such as the care planning process, can mitigate cognitive biases by standardising assessments and ensuring important factors in the patient’s assessment and care are not overlooked.
- Reflection: Routinely reflecting on your decision-making processes can help to identify potential biases that may influence your clinical judgement.
- Collaboration: Collaborating with colleagues and seeking differing opinions can help to reduce the risk of cognitive biases.
The Care Planning Process
The Care Planning Process is a critical thinking model based on a systematic approach to patient-centred care. Nurses use this process to perform clinical reasoning and make clinical judgements when planning and providing patient care. This process has been adapted from the original nursing process based on the American Nursing Association’s Standards of Professional Nursing Practice (2021). To better align with the scope of practice for registered nurses in Australia, we have adapted the traditional nursing process by replacing “diagnosis” with “problem identification” to avoid confusion with medical diagnosis, which falls outside the RN’s role. The Care Planning Process consists of five key components: Assessment, Problem Identification, Developing goals, Implementing interventions, and Evaluating outcomes. Each of these components is further broken down into the key tasks involved in each step of the process.
The Care Planning Process is a continuous, cyclical process that is constantly adapting to the patient’s current health status. It requires ongoing assessment, evaluation, and adjustment to ensure care remains aligned with the patient’s evolving needs, preferences and goals. See Figure 2 for an illustration of the Care Planning Process.
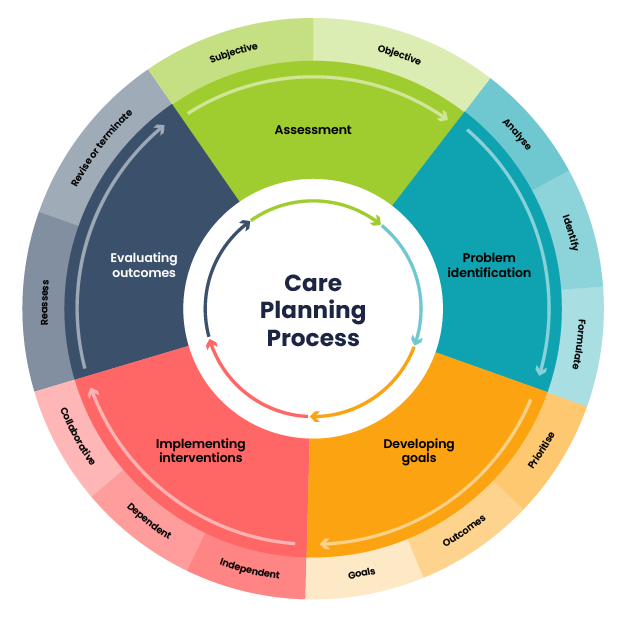
Now let’s take a closer look at each component of the Care Planning Process.
Assessment
Assessment is the first step of the care planning process. The assessment phase of the process aligns with Standard 4 of the Registered Nurse Standards for Practice: Comprehensively conducts assessments (Nursing and Midwifery Board of Australia [NMBA], 2016). This phase involves gathering objective and subjective data to establish a complete understanding of the patient’s health status, needs, and priorities. Information is collected through multiple methods, including patient interviews, physical examinations, observations, and reviewing health records, ensuring a holistic view of the individual. This involves systematically and continuously collecting relevant data related to health and quality of life. This process should be carried out with compassion and respect for each person’s wholeness, inherent dignity, worth, and unique attributes. Accurate and thorough assessments form the foundation for identifying patient problems and planning effective, person-centred care (NMBA, 2016).
Nurses assess patients to gather information to inform the plan of care. Data is considered subjective or objective and can be collected from multiple sources. Click on the tabs below to understand the different data collected in each category.
Sources of Assessment Data
There are three sources of assessment data: interview, physical examination, and review of laboratory or diagnostic test results. Click through each section of the sources of data for more information.
Types of Assessments
Several types of nursing assessment are used in clinical practice:
Problem Identification
Problem identification is the second step of the care planning process and aligns with Standard 1 of the Registered Nurse Standards for Practice: Thinks critically and analyses practice (NMBA, 2016). This standard requires the nurse to use a variety of thinking strategies and the best available evidence to make clinical decisions. The desired outcome of this step is the formulation of problem statements, often referred to as a ‘nursing problem’.
Three components that lead to the identification of problems include analysing the data, identifying actual or potential problems, and formulating problem statements. The ability to analyse and compare data effectively to identify accurate problems is a sophisticated skill. It is demonstrated at higher levels as a nurse gains more experience. Experienced nurses often appear to interpret data as second nature; however, it is important to remember that this ability has developed through exposure to a wide range of clinical experiences. While novice nurses tend to focus on more obvious signs or symptoms that are out of range, experienced nurses will pick up on more subtle cues and continue to investigate and analyse the data surrounding these (Levett-Jones, 2023). As a novice nurse, it is recommended to use a structured approach to assessment and problem identification consistently. This reduces the likelihood of missing problems and ensures a thorough identification of issues, systematically addressing all patient needs and leading to a more effective and personalised care plan.
Analysing the Data
During data analysis, nurses compare collected data, such as signs and symptoms, with established norms and standards to identify any deviations from what is considered normal. In this process, they distinguish the relevant data from the irrelevant. Once the relevant data has been identified, the clustering of information occurs. This clustering involves matching patterns and identifying relationships to generate tentative hypotheses about the patient’s condition. Additionally, the nurse will look for gaps and inconsistencies in the data collected to ensure a comprehensive understanding of the patient’s health status is achieved. Discovering the gaps and inconsistencies may instigate the collection of further data to either support or negate the hypothesis (validation).
Identifying Problems
A nursing problem is a clinical judgement that is made following analysis of all available data on the patient’s presenting issues. Nursing problems focus on a human response to actual or potential health conditions or life processes. The problem should, where possible, identify a causative factor to allow the development of targeted intervention/care. There are two types of problems that should be identified at this stage: Actual and potential problems.
Accuracy in problem identification is vital for care planning. Nurses can verify accuracy by clearly establishing connections between the defining characteristics, related factors, and/or risk factors identified during the patient’s assessment. It is important that nursing problems focus on the human response to the health condition and not the medical diagnosis. Key differences between medical diagnosis and nursing problems exist.
 |
Medical diagnoses target a specific illness, injury, or disease process, remain constant until a cure or resolution is achieved, and are diagnosed by a medical practitioner (Delaune, 2023). For example, a medical diagnosis of “pneumonia” is a condition caused by an infection in the lungs. Medical treatment will be to treat the infection (e.g., antibiotics). |
|
|
Nursing problems are a response to a condition that causes an impact on the patient (a human response). The impacts can change as the patient’s health or situation changes and interventions to assist will fall into the scope of practice of the nurse (Delaune, 2023). For example, the patient who was medically diagnosed with Pneumonia experiences inflammation and fluid accumulation in the lungs as part of this condition. This impacts the patient as respiratory effort increases to improve gas exchange in the lungs. This causes undesirable effects such as fatigue. Through the analysis of the data, the nurse will conclude the patient is experiencing fatigue related to impaired gas exchange evidenced by increased work of breathing, cyanosis and low oxygen saturation. The nurse can now plan treatment toward the cause (impaired gas exchange) to relieve the patient’s responses, for example, deep breathing and coughing exercises to expel fluid from the lungs, sitting the patient upright to improve gas exchange.
|
When planning care for a patient the nurse will consider events that are happening at that point in time for the patient and those that could possibly develop in the future if interventions are not implemented. Problems are therefore classified as either an actual problem or a potential problem.
Formulating Problem Statements
To ensure accurate care planning nursing problem statements need to remain focused towards the human response, and causative factors need to be clear. It is therefore important problem statements are written in a manner that reflects this.
A problem statement should contain the problem, related factors, and defining characteristics and be written as either a two or three part statement using the PAS format.
Problem (P): The problem (actual or potential); phrased with ‘is experiencing’ or ‘is at risk of’.
Aetiology (A): The related factors (i.e., the aetiology/cause) of the problem; phrased as “related to”.
Signs and Symptoms (S): The defining characteristics observed during the patient assessment. This will include the signs and symptoms/subjective and objective data/clinical cues that led to the identification of the problem for the patient; phrased with “as evidenced by”.
Two common errors are seen when formulating problem statements and are explored below:
|
|
1. The nurse focuses on individual signs and symptoms (cues) rather than completing a full analysis. Incorrect problem statement: (Patient name) is experiencing tachycardia related to pain evidenced by heart rate of 110bpm. In the example, the nurse has focused on one particular sign and not the causative factor that is producing this sign. Further analysis of the patient’s situation is required to allow interventions to be targeted towards the causative factor of tachycardia. In this case, the human response that is observable is pain, to treat the pain we need to know the causative factor, therefore adding a focused pain assessment can assist in understanding this. Correct problem statement: (Patient Name) is experiencing acute pain in ankle related to tissue swelling as evidenced by recent surgery, patient statement of 6/10 on VAS, facial grimacing on movement, and tachycardia. |
|
|
2. The nurse uses medical terminology rather than nursing terminology. Incorrect problem statement: (Patient name) is experiencing inflammation and fluid accumulation in the lungs related to pneumonia evidenced by low oxygen saturation and shortness of breath. In the example, the focus has become the medical diagnosis rather than that of the human response displayed with the causative factor. Further analysis of the situation can establish what issues the accumulation of fluid is causing for the patient. Correct problem statement: (Patient name) is experiencing fatigue related to impaired gas exchange evidenced by increased work of breathing, cyanosis and low oxygen saturation.
|
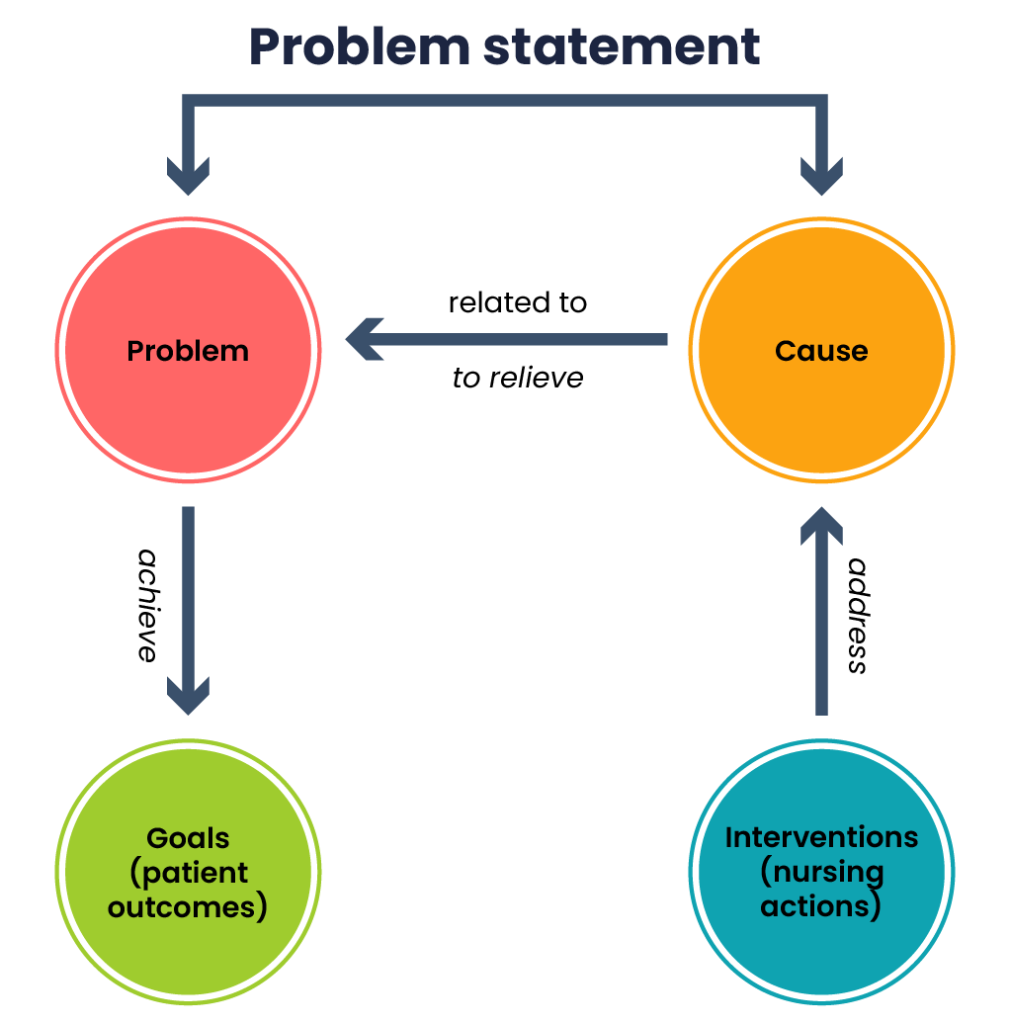
After formulating problem statements tailored to your patient’s specific assessment findings, it is essential to evaluate whether the identified problem statement addresses the root cause of the issue. Refer to Figure 3 for a cognitive aid designed to support the evaluation of your problem statements.
Developing Goals
Once problems have been identified, the nurse collaborates with the patient to determine desired outcomes and set goals to achieve them. This third stage of the care planning process involves the development of comprehensive care plans that address the patient’s specific health concerns.
Care planning aligns with Standard 5 of the NMBA Registered Nurse Standards for Practice: Develops a plan for nursing practice. In accordance with this standard, nurses are accountable for developing and communicating nursing care plans based on comprehensive assessments, evidence, and agreed priorities. They must collaboratively establish goals, actions, outcomes, and timeframes, ensuring these are clearly documented and effectively communicated. Plans must be regularly evaluated and adjusted to support the achievement of outcomes, with resources coordinated appropriately (NMBA, 2016).
During the goal development phase, the nurse focuses on three key areas:
- Prioritising identified problems
- Identifying outcomes
- Developing patient-centred short- and long-term goals
Prioritising Identified Problems
Priority setting is a crucial skill for nurses, involving the determination of which actions must come first to ensure patient safety and optimal outcomes. Nurses frequently prioritise their actions throughout their shifts, with the highest priority given to patient problems that could result in harm if left untreated, especially life-threatening issues. Each patient situation is unique, necessitating different priorities. Involving patients in the planning process ensures their needs are met.
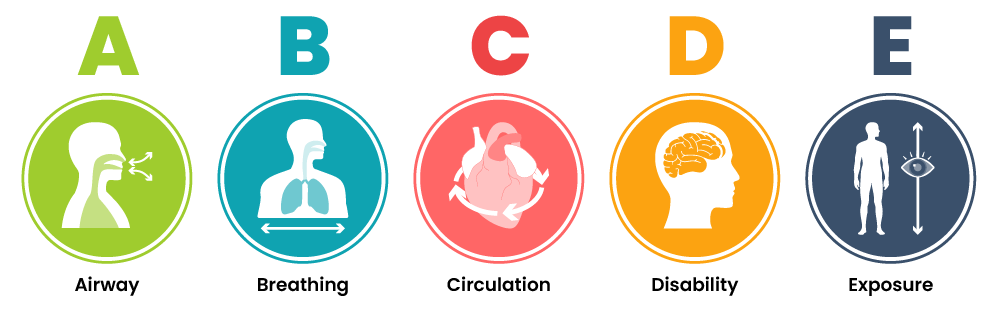
Several concepts guide the prioritisation of care, including the “Safety First” principle and the ABCDE health assessment framework. Considerations are also made in regard to actual and potential problems, acute vs chronic conditions and any uncompensated condition. When considering the intervention or care to be provided the least invasive option is the preferred choice.
Safety first
Safety always comes first, addressing any immediate dangers to both the healthcare provider and the patient before moving on to other priorities. For example, a patient in immediate danger from a fire must be moved before any life-saving measure can begin.
ABCDE approach to health assessment framework
The ABCDE approach (Airway, Breathing, Circulation, Disability, and Exposure) is used during patient assessment and can also help prioritise care. Problems are addressed in this order, with life-threatening issues attended to first, interventions should start immediately and be resolved before moving to the next step. For instance, if you are about to clean a tracheostomy (exposure) and notice sputum collecting in the airway (airway), suctioning the airway becomes the priority before proceeding with the cleaning (A before E).
Using the concepts discussed, the following is an example of prioritisation:
|
|
Example of prioritisation A frail elderly gentleman is admitted with pneumonia and is currently experiencing an increase in his work of breathing. The following problems have been identified and prioritised.
The problems were prioritised based on immediacy and severity of impact on the patient, with patient safety considered first and working through the hierarchy order of ABCDE. |
Development of Outcomes and Goals
Before you write a nursing goal, it is essential to know both the desired and expected outcomes. This is why we prioritise understanding these outcomes first. However, it is important to note that the goal and outcome need to be developed in combination. For this reason, we will discuss these two important stages together. This integrated approach helps in creating an effective, person-centred care plan that is tailored to the patient’s needs and provides a clear pathway for evaluating progress and success.
Desired and Expected Outcomes
Outcomes in the care planning process may refer to two related but distinct concepts: the desired outcome and the expected outcome. A desired outcome is the specific result a patient would like to achieve through nursing care and intervention. It reflects the patient’s personal goals and should align with the expected outcome, which is the anticipated response to nursing interventions. Expected outcomes serve as measurable benchmarks for evaluating whether goals have been successfully met. Both types of outcomes should be specific, realistic, and measurable. Clearly defined desired outcomes help shape both short- and long-term goals, providing direction, focus, and a framework for evaluating the effectiveness of care.
Short and Long-Term Goals
The nursing goal is a broad statement of the overall direction in which the patient must progress to improve the nursing problem and is often the direct opposite of the problem. Goals may be short-term or long-term, depending on the patient’s needs. Short-term goals address immediate needs, while long-term goals guide planning for discharge or ongoing care.
Example of a broad goal: (Patient name) will achieve a state of fluid balance.
Developing Patient-Centred Short and Long-Term Goals Aligned with Outcomes
Setting goals and outcomes gives direction for interventions and establishes standards for evaluating effectiveness. A patient-centred goal is a specific, measurable objective aimed at optimal health and independence levels. Goals require realism and need to be tailored specifically to each patient’s needs, values, and cultural beliefs. To promote person-centred care the patient and family members should be included in the goal-setting process, this motivates participation and the likelihood of successfully achieving the goals.
Expected outcomes are required to determine when goals have been met. They are used to evaluate an intervention’s effectiveness in resolving problems. The outcome includes the specific response desired to interventions and needs to be specific, measurable, and set within time frames.
Example of a broad goal with expected outcomes: (Patient name) will achieve a state of fluid balance (broad goal) evidenced by equal input/output on fluid balance chart over the next 24 hours (expected outcome).
The expected outcomes are linked to the broad goal with the identifying term “evidenced by”, by linking these outcomes the broad goal has now become specific. In this text, we will refer to this as a goal statement. These statements should contain five components, easily remembered using the “SMART” mnemonic: Specific, Measurable, Attainable, Relevant, and Time-based.
Each of these components is further described in the following subsections.

Implementing Interventions
Once goals and outcomes have been established the nurse begins planning nursing interventions that are most appropriate to implement. A nursing intervention is that which is within the scope of the registered nurse’s role and may include ongoing observation, assessment and evaluations, preventative measures to reduce risks of complications, treatments for physical care, education and health promotion, and referral to specialist care both within the field of nursing (e.g. wound care specialist) or the multidisciplinary team (e.g social worker) (Berman et al., 2021).
Nursing intervention, when able should target the cause of the problem (the ‘related to’). When it is not possible to alleviate the causative factors then interventions are directed at the signs and symptoms. Nursing intervention selection can vary widely depending on the individual circumstances of the patient and the causative factor, therefore accuracy of problem statement development and identification of the correct cause is vital in achieving the best possible outcome.
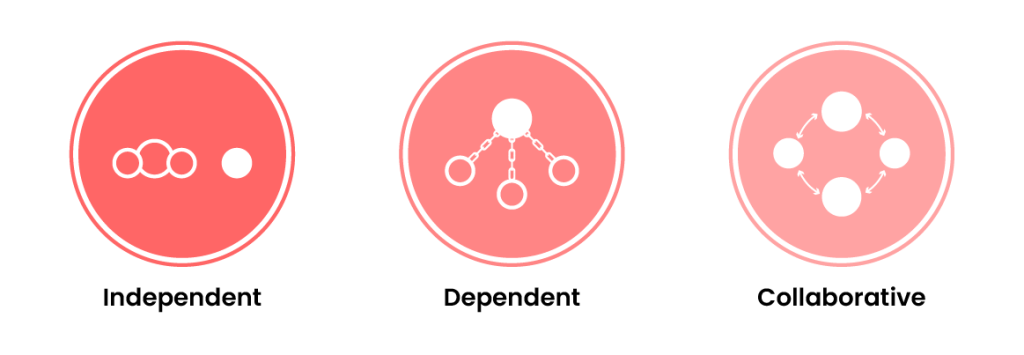
There are three types of nursing interventions that may need to be coordinated or escalated by the nurse: independent, dependent, and collaborative. Click on each of the tabs below to learn more about the three types of nursing interventions:
Creating and Recording the Plan of Care
Once interventions are determined, an overall plan of care, known as a nursing care plan, is recorded. Care plans are crucial for communicating planned care for patients, aiming to prevent incomplete, incorrect, or inaccurate care (Crisp et al., 2021). These written guides ensure continuity of care over time and among different nurses and health professionals.
The methods for recording care plans vary between facilities and can be presented in different formats depending on the services provided. Many facilities use computer-generated tools. Regardless of the format, each care plan should be individualised, including identified problems, goals of care, expected outcomes, and planned nursing interventions.
Clinical management pathways are commonly used tools that contain preplanned expected pathways for patients based on specific diagnoses or planned procedures. These plans are developed using best practices, clinical guidelines, and evidence-based practice. They clearly list treatment goals and the actions required by all healthcare team members to achieve those goals. Any variances from the plans are documented in the appropriate section, allowing for individualised care. The plans also include evaluation criteria to assess the effectiveness of the planned care.
Documentation of the interventions and patient responses is an essential part of this phase. During implementation, the nurse must critically think and use clinical judgement. Continual reassessment of the patient during the phase is necessary to detect any changes in the patient’s condition that may require modification of the plan. The need for continual patient reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
Implementing the Interventions
Implementation requires several steps and this includes reassessing the person, determining nurses’ needs for assistance, the act of implementing intervention, and documenting the activities (Berman et al., 2021).
Integral to this phase is the ability to make decisions about delegation of interventions if and when appropriate. The Decision-Making Framework, developed by the NMBA used in conjunction with the standards for practice, policies, regulations and legislation, supports nurses and midwives in making consistent, safe, person-centred, and evidence-based decisions regarding the scope of practice, delegation, and supervision (NMBA, 2020). To read this document and understand more about decision-making and the scope of practice relevant to your role, you can access the framework on the Frameworks page of the Nursing and Midwifery Board website.
Evaluation

Evaluation, the fifth and final step of the care planning process, aligns with Standard 7 of the NMBA Registered Nurse Standards for Practice: Evaluates outcomes to inform nursing practice. Nurses assess the patient’s response to interventions, reevaluate the data, and compare the outcomes with the expected results. If needed, modifications to the plan of care are made to promote better patient outcomes and address any new or evolving health needs.
Reassess to Determine if Outcomes are Achieved
In this step, the nurse conducts a thorough reassessment of the patient to determine the extent to which the established outcomes have been achieved. They assess whether the patient’s health has improved, stabilised, or deteriorated based on the identified criteria. They compare the patient’s current status with the expected outcomes defined in the planning phase. This reassessment involves collecting new data, evaluating changes in the patient’s condition, and reviewing any documentation or feedback from the patient. By evaluating the progress made toward achieving the outcomes, nurses can determine if the interventions have been effective in addressing the identified concerns.
Revise or Terminate Nursing Plan of Care
Based on the evaluation findings, nurses determine whether revisions to the nursing plan of care are necessary or if the plan can be terminated. If the outcomes have been achieved, the plan may be concluded, and the nurse focuses on discharge planning or transition to ongoing care. However, if the outcomes have not been met, the nurse revises the plan by identifying new interventions or modifying existing ones to better support the patient’s progress toward achieving the desired outcomes. Nurses continue to reassess and evaluate the patient’s condition at regular intervals, adjusting the plan of care as needed to optimise outcomes and address any emerging concerns.
Case Study: Putting it all Together
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. To assist with your nursing care plan, answer the critical thinking questions below:
The patient, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The patient also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the patient avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
The Clinical Reasoning Cycle
Evidence indicates that, despite the presence of warning signs preceding adverse events, at-risk patients are not consistently identified or managed effectively. According to Levett-Jones et al. (2010, p. 516), clinical reasoning is defined as ‘the process by which nurses (and other clinicians) collect cues, process the information, come to an understanding of a patient problem or situation, plan and implement interventions, evaluate outcomes, and reflect on and learn from the process’. The development of the Clinical Reasoning Cycle stems from the recognition that deficiencies in clinical reasoning skills significantly contribute to nurses’ inability to recognise and appropriately respond to patient deterioration, a phenomenon referred to as “failure to rescue.” This highlights the critical need for educational strategies to enhance clinical reasoning skills in nursing practice (Levett-Jones et al., 2010, p. 515).
The Clinical Reasoning Cycle is a dynamic and reflective tool for guiding complex clinical decisions, while the Care Planning Process provides a more structured, linear framework for delivering care. Together, these approaches complement each other in promoting high-quality, evidence-based nursing practice and person-centred care.
The CRC figure outlines the intricate nature of a nurse’s decision-making, clinical reasoning, and care planning process, which is divided into eight phases. Click or tap on the ‘+’ buttons for a summary of these eight phases.
The CRC in Action
Let’s take a closer look at the Clinical Reasoning Cycle by applying it to a case study.
Many of these phases closely align with the nursing process discussed earlier in this chapter, reflecting similar steps. However, the CRC stands out in its value for managing more complex patient cases and includes an additional step: reflection. This crucial element of nursing practice fosters deeper learning and professional growth. Now it is time to apply your newfound knowledge with a case study. Read the following ISBAR handover, then answer the questions in the activity that follows.
Case Study – Mr James
ISBAR handover for Mr James
Introduction: This is Mr James
Situation: A 72-year-old male admitted with complaints of shortness of breath and fatigue. He has a history of COPD.
Background: Mr James is on home oxygen therapy and typically uses 2L oxygen via nasal cannula. His last ABG, done two months ago, showed mild hypoxaemia. He has been increasingly tired over the past 24 hours, with worsening breathlessness.
Assessment: On assessment, his respiratory rate is 24/min, and his SpO2 is 88% on 2L oxygen. He appears fatigued but is responsive. He denies chest pain. Lungs show reduced air entry bilaterally with no wheezes noted. He has no fever.
Recommendation: We might need to review his oxygen therapy.
Summary
The care planning process and clinical reasoning cycle are both essential frameworks for delivering safe, effective, and patient-centred care. These two frameworks complement each other, involving a systematic approach to assess patients, plan and implement care, and evaluate outcomes. You have now learned how to perform each step of the care planning process and clinical reasoning cycle. Regardless of which process or cycle you use, critical thinking, clinical reasoning, and clinical judgement are essential when assessing the patient, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the patient achieve expected outcomes. Throughout the entire process, the patient always remains the cornerstone of nursing care. Providing individualised, patient-centred care and evaluating whether that care has been successful in achieving patient outcomes is crucial for delivering safe, professional nursing practice.
References
American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association.
Australian Commission on Safety and Quality in Health Care. (2021). National safety and quality health service standards (2nd ed.). https://www.safetyandquality.gov.au/sites/default/files/2021-05/national_safety_and_quality_health_service_nsqhs_standards_second_edition_-_updated_may_2021.pdf
Berman, A., Frandsen, G., Snyder, S., Levett-Jones, T., Burston, A., Dwyer, T., Hales, M., Harvey, N., Langtree, T., Moxham, L., Reid-Searl, K., Rolf, F., Stanley, D., Kozier, B., & Erb, G. L. (2021) . Kozier and Erb’s fundamentals of nursing: Concepts, process and practice, (5th Australian ed.). Pearson Australia.
Connor, J., Flenady, T., Massey, D., & Dwyer, T. (2023). Clinical judgement in nursing: An evolutionary concept analysis. Journal of Clinical Nursing, 32(13–14), 3328–3340. https://doi.org/10.1111/jocn.16469
Crisp, J., Douglas, C., Rebeiro, G., & Waters, D. (2021). Potter and Perry’s fundamentals of nursing (6th ed.). Elsevier Australia.
Dickison, P., Haerling, K., & Lasater, K. (2019). Integrating the National Council of State Boards of Nursing Clinical Judgment Model into nursing educational frameworks. Journal of Nursing Education, 58(2), 72-78. https://doi.org/10.3928/01484834-20190122-03
DeLaune, S. C., Ladner, P. K., McTier, L., Tollefson, J., & Lawrence, J. (2020). Fundamentals of nursing: Australia and New Zealand (2nd ed.). Cengage.
DeLaune, S.C.., Ladner, P. K., McTier, L., Tollefson, J., & Lawrence, J. (2023). Fundamentals of nursing: Australia and New Zealand (3rd ed.). Cengage.
Griffits, S., Hines, S., & Moloney, C. (2023). Characteristics and processes of registered nurses’ clinical reasoning and factors relating to the use of clinical reasoning in practice: A scoping review. JBI Evidence Synthesis, 21(4), 713–743. https://doi.org/10.11124/JBIES-21-00373
Gupta, M., & Upshur, R. (2012). Critical thinking in clinical medicine: What is it? Journal of Evaluation in Clinical Practice, 18(5), 938–944. https://doi.org/10.1111/j.1365-2753.2012.01897.x
Jala, S., Fry, M., & Elliott, R. (2023). Cognitive bias during clinical decision‐making and its influence on patient outcomes in the emergency department: A scoping review. Journal of Clinical Nursing, 32(19–20), 7076–7085. https://doi.org/10.1111/jocn.16845
Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41(4), 215-221. https://doi.org/10.1097/01.NEP.0000000000000669
Levett-Jones, T. (Ed.). (2023). Clinical reasoning: Learning to think like a nurse (3rd ed.). Pearson Australia.
Levett-Jones, T., Hoffman, K., Dempsey, J., Jeong, S. Y., Noble, D., Norton, C. A., Roche, J., Hickey, N. (2010). The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today, 30(6), 515–20. https://doi.org/10.1016/j.nedt.2009.10.020
Manetti, W. (2019). Sound clinical judgment in nursing: A concept analysis. Nursing Forum, 54(1), 102–110. https://doi.org/10.1111/nuf.12303
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards of practice. https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-standards/registered-nurse-standards-for-practice.aspx
Nursing and Midwifery Board of Australia. (2020). Framewords. https://www.nursingmidwiferyboard.gov.au/codes-guidelines-statements/frameworks.aspx
Papp, K. K., Huang, G. C., Lauzon Clabo, L. M., Delva, D., Fischer, M., Konopasek, L., Schwartzstein, R. M., & Gusic, M. (2014). Milestones of critical thinking: A developmental model for medicine and nursing. Academic Medicine, 89(5), 715–720. https://doi.org/10.1097/ACM.0000000000000220
Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15(7), 37-39. https://www.myamericannurse.com/nurse-preceptors-and-new-graduate-success/
Reji, R. K. & Sushma, S. (2022). Critical thinking and decision making: Essential skills in nursing. International Journal of Research in Pharmaceutical Sciences, 13(1), 61-67. https//doi.org/10.26452/ijrps.v13i1.21
Scheffer, B., K. & Rubenfeld, M., G. (2000). A consensus statement on critical thinking in nursing. Journal of Nursing Education, 39(8):352-9. https://doi.org/10.3928/0148-4834-20001101-06
Tanner, C. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204-211. https://doi.org/10.3928/01484834-20060601-04
Thompson, J., Bujalka, H., McKeever, S., Lipscomb, A., Moore, S., Hill, N., Kinney, S., Cham, K. M., Martin, J., Bowers, P., & Gerdtz, M. (2023). Educational strategies in the health professions to mitigate cognitive and implicit bias impact on decision making: A scoping review. BMC Medical Education, 23(1), 455–23. https://doi.org/10.1186/s12909-023-04371-5
Tollefson, J., & Hillman, E. (2022). Clinical psychomotor skills : Assessment tools for nurses (8th ed.). Cengage Learning.
Willers, S., Jowsey, T., & Chen, Y. (2021). How do nurses promote critical thinking in acute care? A scoping literature review. Nurse Education in Practice, 53, 103074–103074. https://doi.org/10.1016/j.nepr.2021.103074
Chapter Attribution
This chapter has been adapted in parts from:
Clinical nursing skills (2024) by Christie Bowen, OpenStax, is used under a CC BY licence.
Media Attributions
- Core Thinking Skills © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Subsections of the Care Planning Process © Penelope Coogan, Leisa Sanderson, and Tracey Gooding adapted by Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Nursing Problem Statement Process © Penelope Coogan, Leisa Sanderson, and Tracey Gooding adapted by Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- ABCDE Assessment © David Peran, Jiri Kodet, Jaroslav Pekara, Lucie Mala, Anatolij Truhlar, Patrik Christian Cmorej, Kasper Glerup Lauridsen, Ferenc Sari & Roman Sykora adapted by Eileen Siddins is licensed under a CC BY (Attribution) license
- SMART Goals © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Intervention Types © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Evaluating Outcome Types © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
An intellectual process used to analyse and interpret situations, enabling problem-solving and sound decision-making
A complex cognitive process that uses formal and informal thinking strategies to gather and analyse patient information, evaluate the significance of this information, and weigh alternative actions
The result of critical thinking and clinical reasoning using inductive and deductive reasoning
Making a specific observation from the obvious
Making generalisations from specific data
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder
Predictions of a relationship between variables
A specific illness, injury, or disease process diagnosed by a medical practitioner
Signs that are observable by an observer or can be measured or tested against an acceptable standard
Symptoms that are only apparent to the person that is affected and can only be verified only by that person
A measurable behaviour demonstrated by the patient’s response to nursing interventions
A human response to a condition that is causing an impact on the patient
The skillful process of deciding which actions to complete first for patient safety and optimal patient outcomes