Managing Oxygenation and Perfusion
Leisa Sanderson and Penelope Coogan
Learning Outcomes
In this chapter, you will learn how to:
- Describe the physiological processes of oxygenation and perfusion, including the role of the respiratory and cardiovascular systems
- Identify and explain clinical indicators of ventilation/perfusion mismatch, hypoxia and hypoxemia
- Recognise lifestyle and behavioural factors that contribute to cardiopulmonary dysfunction and disease progression
- Develop knowledge of cardiopulmonary investigation that supports diagnosis and treatment planning
- Demonstrate foundational skills in performing electrocardiograms (ECGs) and rhythm strip interpretation
- Describe the principles of oxygen therapy, including flow rate, FiO2, humidification and safety precautions
- Identify common oxygen delivery devices, their indication and associated nursing considerations.
The main functions of the cardiac and respiratory systems are to supply the body’s oxygen demands. The respiratory (or pulmonary) system’s primary purpose is the exchange of gases that are essential for life. Gas exchange occurs at the capillary-alveolar bed (or membrane) where capillaries and alveoli meet. The process of breathing, inspiration (inhaling) and expiration (exhaling), provides O2 and removes CO2 waste. The cardiovascular system’s role is to provide a means of transport for O2 and other nutrients and to remove waste products. The joining of these systems as the cardiopulmonary system combines the actions of cardiac perfusion with respiratory ventilation to provide the essential processes of oxygenation and perfusion.
It is important for nurses to have knowledge of the anatomy and physiology of the respiratory and cardiac systems in order to apply the concepts discussed in this chapter. However, you may wish to revise Chapter 18, The Cardiovascular System and Chapter 22, The Respiratory System, in Anatomy and Physiology 2e.
Structure and Function of the Cardiovascular System
The cardiovascular system plays a vital role in maintaining homeostasis by transporting oxygen, nutrients, and hormones to body tissues while removing carbon dioxide and other metabolic wastes. This system comprises the heart, blood vessels, and blood, and works closely with other systems, in particular the respiratory, gastrointestinal, and renal systems, to support cellular function and overall health.
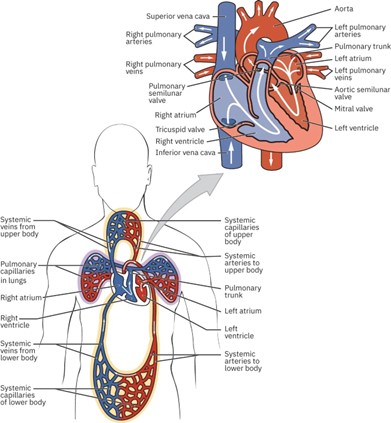
An understanding of the heart’s structure and function is essential for nursing practice. The heart comprises four chambers: two atria and two ventricles. The right ventricle pumps deoxygenated blood to the lungs via the pulmonary circulation, while the left ventricle pumps oxygenated blood through the aorta out to the systemic circulation. Surrounding this central pump is an extensive vascular network of arteries, veins and capillaries that facilitates the distribution of blood and the exchange of gases, nutrients, and waste products at a cellular level.
The Circulatory System
The heart, acting as the central pump, propels blood through two major systems:
- Pulmonary circulation – transports deoxygenated blood to the lungs, where it picks up oxygen to deliver to the heart and drops off carbon dioxide for exhalation
- Systemic circulation – transports oxygenated blood to all of the tissues of the body and returns deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
Gas exchange occurs at the alveolar-capillary membrane in the lungs, where oxygen enters the bloodstream and carbon dioxide is expelled. This close relationship between the respiratory and cardiovascular systems is essential for effective oxygenation and perfusion. Any disruption in either system can impair tissue oxygen delivery, leading to hypoxia.
Understanding Cardiac Output and Regulation of Blood Flow
Cardiac output (CO) refers to the amount of blood the heart pumps into the circulation each minute. More specifically, it is the volume of blood ejected from the left ventricle every minute and is a key determinant of tissue perfusion.
Cardiac output is calculated using the formula CO = HR × SV
- HR is the heart rate (beats per minute)
- SV is the stroke volume, or the amount of blood pumped by the left ventricle with each contraction.
Stroke volume (SV) is the volume of blood expelled from the left ventricle during a single systolic contraction. It is influenced by three primary factors:
- Preload – the degree of stretch in the ventricles before contraction, related to venous return.
- Contractility – the strength or force of the ventricular contraction.
- Afterload – the resistance the ventricles must overcome to eject blood into the arteries (Betts et al., 2022).
In a healthy adult weighing approximately 70 kilograms, normal cardiac output ranges from 4 to 6 litres per minute, depending on activity level and metabolic demand. The volume of circulating blood and cardiac output fluctuates in response to the body’s oxygen and metabolic requirements. For instance, during physical activity, pregnancy, or fever, the body’s demand for oxygen increases, prompting the heart to pump more blood to meet these needs. Conversely, during periods of rest or sleep, metabolic activity slows, and cardiac output naturally decreases (Ingham-Broomfield, 2021). Other examples include:
- Stress or emotional responses can trigger increased heart rate and blood flow due to sympathetic nervous system activation.
- Exposure to cold may cause vasoconstriction and alter blood distribution to preserve core body temperature.
- During hemorrhagic shock, circulating volume decreases significantly, requiring compensatory mechanisms to maintain perfusion.
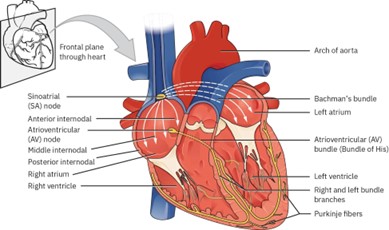
The Cardiac Cycle
The cardiac cycle refers to the physiological process of one complete heartbeat. It encompasses the sequence of events from the initiation of atrial contraction to the relaxation of the ventricles. Throughout this cycle, both the atria and ventricles pass through phases of contraction (systole) and relaxation (diastole), which must be precisely regulated and coordinated to ensure effective blood flow throughout the body. To achieve this, the heart relies heavily on its electrical conduction system, a specialised network of bundles and fibres that generate and transmit electric impulses. These impulses trigger the contraction of the myocardial muscle tissue, enabling the heart to pump blood through both the pulmonary and systemic circuits. This process maintains optimal cardiac output and ensures adequate tissue perfusion.
The efficiency of the cardiac cycle can be evaluated through clinical indicators such as:
- Heart rate
- Blood pressure
- Heart sounds (can reveal abnormalities in valve function or rhythm).
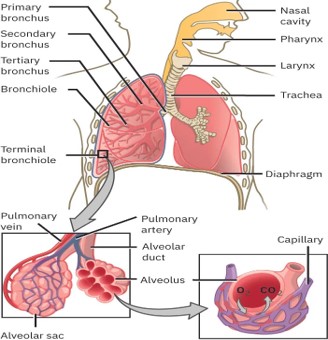
Structure and Function of the Respiratory System
The respiratory system is made up of several key structures, including the nose and paranasal sinuses, the pharynx, the larynx, the trachea, the bronchi and their smaller branches, and the lungs, which contain tiny air sacs called alveoli. These structures are divided into two main areas known as the upper and lower respiratory systems:
The upper respiratory system includes all parts from the nose through to the larynx. Its primary role is to warm, moisten, and filter the air we breathe.
The lower respiratory system begins at the larynx and includes the trachea, bronchi, and lungs. This is further divided into two functional zones:
- The conducting zone comprises the airways from the nose through to the respiratory bronchioles. This zone is responsible for transporting air and continuing the process of warming, humidifying and cleansing.
- The respiratory zone is where the process of gas exchange takes place. It includes the alveoli and associated structures, which allow oxygen to enter the bloodstream and carbon dioxide to be removed (Marieb & Hoehn, 2023). The zone begins where terminal bronchioles meet a respiratory bronchiole. These bronchioles connect to an alveolar duct that opens into a cluster of alveoli. An alveolus is an individual, grape-like sac in the lungs, while an alveolar sac refers to a group of alveoli. Alveoli are elastic and stretch during inspiration, increasing the available surface area for gas exchange. Their thin walls and proximity to the capillaries facilitate the rapid movement of gases between the air and the blood.
Respiratory Cycle
Oxygenation involves interactions between the respiratory and cardiovascular systems, including air movement through the lungs, where O2 and CO2 are exchanged through the alveoli and capillaries as the respiratory and circulatory systems connect and interact at the alveolar-capillary bed. Physiological processes involved include ventilation and perfusion. The combination of respiratory ventilation and cardiovascular perfusion provides O2 (and other nutrients) to the body’s tissues and removes waste products, including CO2, from the tissues.
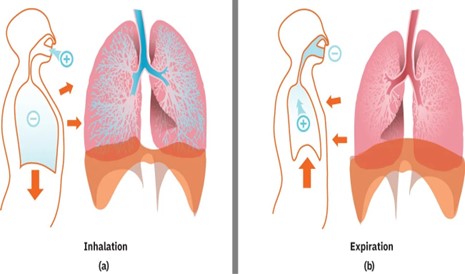
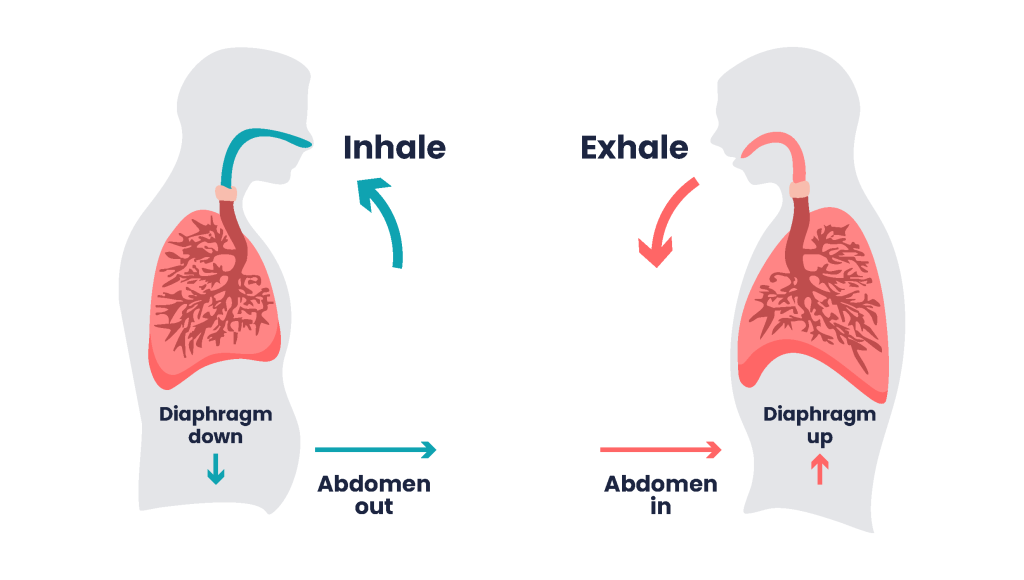
Ventilation
The part of the respiratory cycle whereby the diaphragm and intercostal muscles contract, which enlarges the space within the thorax, is called inspiration. This enlargement lowers the pressure within the alveoli, and air flows into the lungs. During expiration, the muscles that expanded the thoracic cavity now relax, and elastic recoil reduces the pressures in the lungs and surrounding thorax. The pressure within the intrapulmonary system is momentarily higher than atmospheric pressure, and air is passively exhaled from the lungs. Lungs that are compliant and retain the properties of elastic recoil are able to increase and decrease in size and shape with each respiratory cycle. This movement of air into and out of the lungs is called ventilation. The effort required by the body to complete this is called the work of breathing (WOB). WOB is impacted by the degree of lung compliance, airway resistance and the need for active expiration.
Oxygenation
The process when oxygen from the air moves into the bloodstream is called oxygenation. When air enters the lungs and travels to the alveoli, oxygen molecules pass into the capillaries by diffusion.
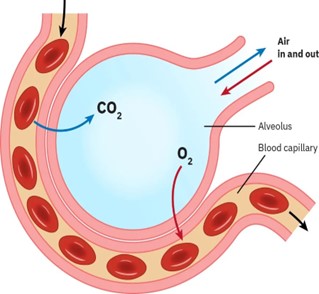
Oxygen is poorly dissolved in blood, with only 1.5% transported in the plasma (Marieb & Hoehan, 2023). The remaining 98.5% occurs by oxygen molecules binding to haemoglobin within the red blood cells. When oxygen binds to haemoglobin, a chemical reaction occurs, and oxyhaemoglobin is formed. Oxyhaemoglobin is a bright red molecule and contributes to the vivid red colour observed in arterial blood. Once oxygen is in the blood, it can travel through the body and be transferred to the tissues. At the tissues, O2 is released from the haemoglobin and taken up by the tissues as needed. It is also here that the waste product, CO2, returns from the body by diffusion into the bloodstream and subsequently the lungs, where it is ultimately removed from the body by exhalation
Disturbances in Pulmonary Function
Disturbances in pulmonary function generally arise from either a ventilation/perfusion (V/Q) mismatch or a reduced ability of the blood to carry oxygen.
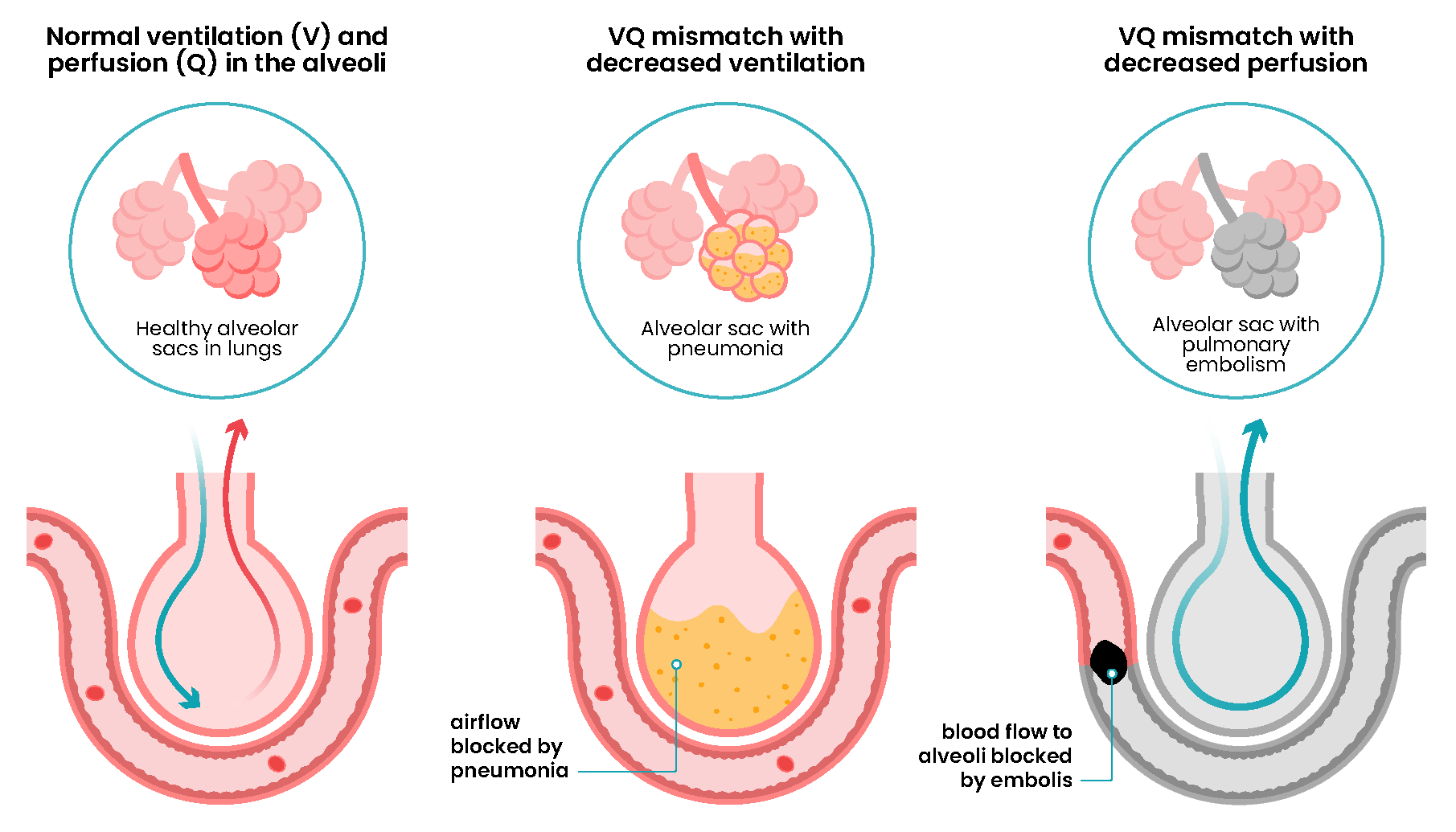
V/Q Mismatch
A V/Q mismatch occurs when there is an imbalance between the air reaching the alveoli (V = ventilation) and the pulmonary capillary blood flow (Q = perfusion). This mismatch is often expressed as a ratio. Lower V/Q ratio reflects shunt-like states, where ventilation is reduced relative to perfusion. A higher V/Q ratio indicates dead space ventilation, where perfusion is reduced relative to ventilation. Some mismatches occur as a combination in different locations of the lung and are referred to as a mixed V/Q mismatch.
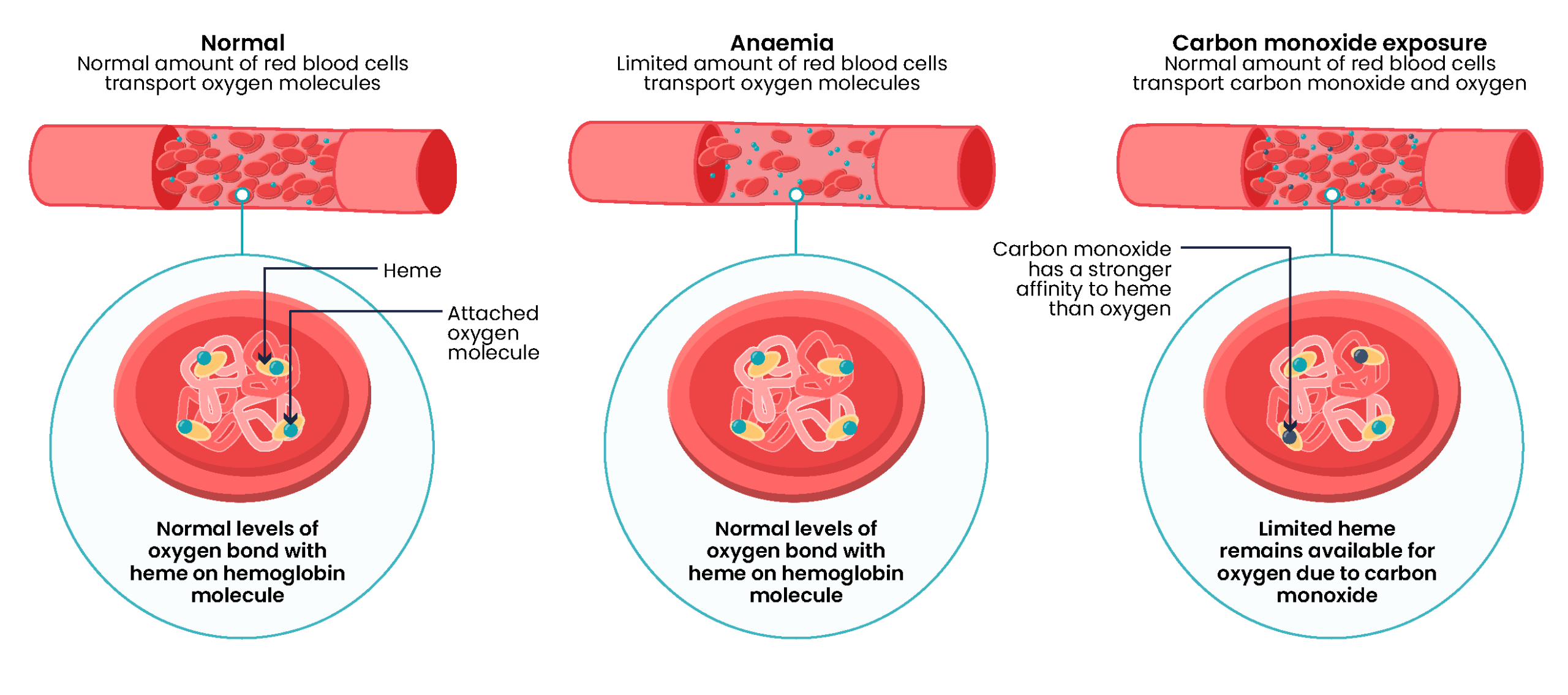
Decreased Oxygen-Carrying Capacity
A reduced ability of the blood to transport oxygen can occur when there is a decrease in circulating haemoglobin or when a competing substance binds to haemoglobin, preventing oxygen transport.
This is commonly seen in conditions such as anemia, haemorrhage, or carbon monoxide poisoning.
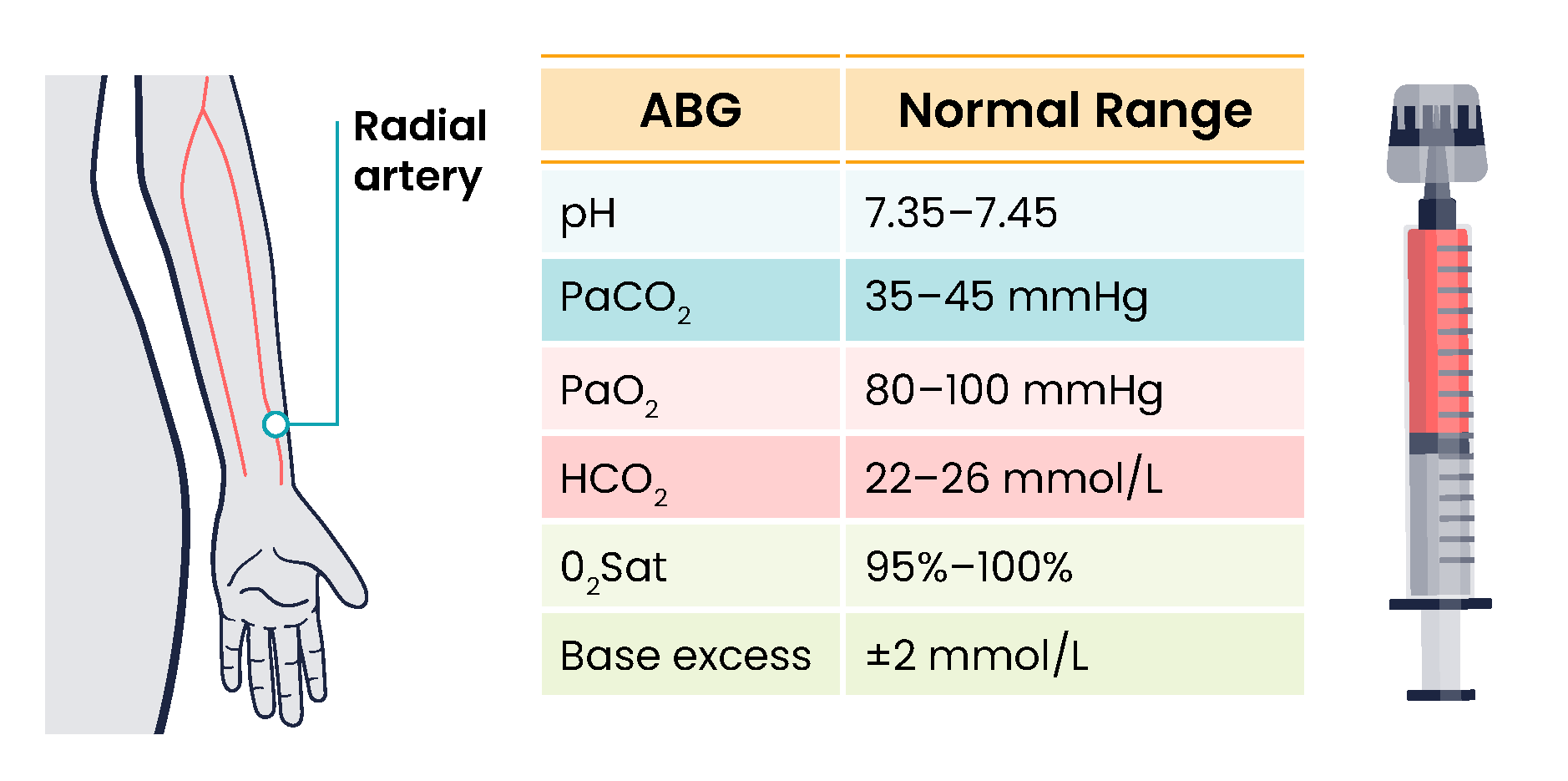
Hypoxemia
Hypoxemia refers to a reduced level of oxygen in the arterial blood, typically measured as a low partial pressure of oxygen (PaO₂) or decreased oxygen saturation (SpO₂). It is identified through arterial blood gas (ABG) analysis or pulse oximetry. Hypoxemia results from impaired gas exchange in the lungs due to conditions such as pneumonia, chronic obstructive pulmonary disease (COPD), pulmonary embolism, or acute respiratory distress syndrome (ARDS). Unlike hypoxia, which affects tissue oxygenation, hypoxemia specifically reflects a deficiency in oxygen within the bloodstream. Clinical signs may include cyanosis, tachypnoea, restlessness, and reduced SpO₂ readings. Prompt recognition and management are essential, as hypoxemia can progress to hypoxia, leading to tissue ischemia and cell death. Treatment typically involves oxygen therapy and addressing the underlying cause of the impaired oxygenation.
Hypoxia
Hypoxia refers to an insufficient supply of oxygen to the tissues, regardless of the oxygen level in the blood. It can occur even when arterial oxygen levels are normal if there is a problem with oxygen delivery or cellular utilisation. There are several types of hypoxia, each with distinct causes.
- Hypoxic hypoxia results from low oxygen availability in the air or lungs, such as in high-altitude environments or respiratory diseases.
- Hypoxaemic hypoxia occurs when the blood’s oxygen-carrying capacity is reduced, as seen in conditions like anaemia or carbon monoxide poisoning.
- Ischaemic hypoxia is due to impaired circulation, such as in heart failure, where oxygenated blood is not effectively delivered to tissues.
- Histotoxic hypoxia arises when cells are unable to use oxygen properly, such as in cyanide poisoning (Marieb & Hoehan, 2023).
Early signs of hypoxia are anxiety, confusion, and restlessness. As hypoxia worsens, the patient’s level of consciousness and vital signs will worsen with an increased respiratory rate and heart rate and decreased SpO2 readings. Late signs of hypoxia include bluish discolouration of the skin and mucous membranes known as cyanosis.
Hypercapnia
Hypercapnia is an elevated level of carbon dioxide in the blood. This level is measured by the PaCO2 level in an ABG test and is indicated when the PaCO2 level is higher than 45. Hypercapnia is typically caused by hypoventilation or areas of the alveoli that are ventilated but not perfused. In a state of hypercapnia or hypoventilation, there is an accumulation of carbon dioxide in the blood. The increased carbon dioxide causes the pH of the blood to drop, leading to a state of respiratory acidosis.
Patients with hypercapnia can present with tachycardia, dyspnea, flushed skin, confusion, headaches, and dizziness. If the hypercapnia develops gradually over time, such as in a patient with chronic obstructive pulmonary disease (COPD), symptoms may be mild or may not be present at all. Hypercapnia is managed by addressing its underlying cause. A noninvasive positive pressure device, such as a BiPAP, may provide support to patients who are having trouble breathing normally, but if this is not sufficient, intubation may be required.
Factors Affecting Ventilation and Perfusion
| Factor / Condition | Mechanism | Effect on Ventilation (V) | Effect on Perfusion (Q) | Disturbance |
| Asthma or angioedema | Increased airway resistance (airway narrowing)can limit airflow into the body, decreasing the amount of oxygen the lungs can utilise | ↓ airflow (bronchoconstriction) | Normal | V/Q mismatch, hypoxaemia |
| COPD | Damage to alveoli and pulmonary capillaries causes loss of elastic recoil and airway collapse – decreases the areas that are available for ventilation, causing inadequate oxygenation | ↓ (air trapping) | ↓ (capillary damage) | V/Q mismatch; chronic hypoxaemia; hypercapnia |
| Atelectasis | Alveoli collapse, leaving fewer capillaries available for gas exchange | ↓ (alveolar collapse) | Normal | V/Q mismatch |
| Neuromuscular disorders (e.g. ALS) | Reduced chest wall compliance due to impaired neuromuscular control (weak respiratory muscles) | ↓ (poor lung expansion) | Normal | Hypoventilation / Respiratory failure |
| Chest trauma (rib fractures) | Impaired chest wall movement secondary to pain | ↓ (mechanical restriction) | Normal | Hypoventilation / atelectasis |
| Alveolar filling disorders/pneumonia | Ventilation is impaired due to the presence of abnormal material (fluid/blood/pus) in the alveoli, compressing lung tissue | ↓ (poor lung expansion) | Normal | V/Q mismatch |
| Pulmonary Embolism / Blood Clot | Perfusion impacted as unable to reach the alveoli | Normal | ↓ (blocked blood flow) | V/Q mismatch |
| Anemia or hemorrhage | Oxygen-carrying capacity is reduced due to low circulating haemoglobin | Normal | Normal | Decreased Oxygen carrying capacity |
| Toxic inhalant (Carbon monoxide) | Impaired oxygen carrying capacity due to low haemoglobin availability | Normal | Normal | Decreased Oxygen carrying capacity |
| Sedation or CNS Depression | Suppressed respiratory centres in brainstem | ↓ (suppressed respiratory drive) | Normal | Hypoventilation / hypercapnia |
| Obesity | Reduced chest wall compliance | ↓ (poor lung expansion) | Normal | Hypoventilation (especially while sleeping) |
Cardiopulmonary Function Considerations
Lifestyle and lifespan factors should be considered when assessing and managing patients with cardiopulmonary conditions. Elements such as diet, exercise, stress and anxiety levels, smoking, alcohol and substance abuse, environmental exposures, and cultural background can all impact cardiopulmonary health and affect response to illness, and the effectiveness of treatment.
Lifestyle Factors
Nutrition
- Obesity: Significantly impairing cardiopulmonary function, obesity restricts lung expansion, reducing respiratory efficiency and increasing the work of breathing. Causing an increased metabolic demand, overall oxygen requirements are raised. Obese individuals have a higher risk of developing anaemia, which further compromises oxygen delivery to the tissues.
- Malnutrition: Malnourished individuals may experience muscle wasting, including the respiratory muscles, leading to reduced respiratory excursion and diminished cough effectiveness. This weakens the body’s ability to clear secretions and maintain airway patency. Malnutrition also contributes to a higher risk of anaemia due to insufficient intake of iron and other essential nutrients required for red blood cell production (World Health Organization [WHO], 2023).
- Dietary fat and cholesterol: Diets high in saturated fats contribute to elevated cholesterol levels, promoting atherogenesis in the coronary arteries (Ingham-Broomfield, 2021). This causes narrowing of the vessels and impairs blood flow to the heart, increasing the risk of developing cardiovascular disease. Over time, this can reduce cardiac output, compromising oxygen delivery throughout the body.
- Sodium intake: Excessive sodium intake is strongly associated with hypertension, a major risk factor for cardiovascular disease (Buckley, 2019). In Australia, the Suggested Dietary Target (SDT) for sodium is 2000 mg/day, with most individuals exceeding this amount (WHO, 2023). Reducing sodium intake is recommended to help reduce blood pressure and decrease strain on the heart and blood vessels.
- Potassium intake: Low potassium intake is considered a risk factor for hypertension as it plays a key role in regulating blood pressure (Buckley, 2019). Higher dietary potassium intake is associated with maintaining lower blood pressure levels, particularly when balanced against sodium intake. Encouraging consumption of potassium-rich foods such as fruits and vegetables can support cardiovascular health and help mitigate the effects of high sodium intake.
Exercise
A balanced exercise program that includes regular physical activity enhances cardiopulmonary function. The National Heart Foundation of Australia recommends at least 150 minutes of moderate-intensity aerobic activity per week to support heart health (National Heart Foundation of Australia, 2016). One of the major benefits of increased physical activity is improved circulation, which enhances oxygenation and tissue perfusion. This contributes to a lower resting heart rate and blood pressure, as well as reduced cholesterol levels. Regular exercise also supports mental health and assists with weight management.
Stress and Anxiety
Chronic stress and severe anxiety can significantly impact cardiopulmonary function by increasing the body’s metabolic rate and oxygen demand. In response to stress, the sympathetic nervous system is activated, leading to an increase in the rate and depth of respiration, pulse rate, and cardiac output. While most healthy individuals can adapt to these physiological changes, those with pre-existing heart disease or acute illness may struggle to meet the heightened oxygen requirements (Ingham-Broomfield 2021).
Smoking, Alcohol/Substance Abuse
Smoking contributes to a number of diseases of the lungs, heart, and vessels. Constant exposure to chemicals in the lungs, mouth, and larynx can cause abnormal cells to divide and cause various cancers. The risk of developing lung cancer is increased by nine times for those who smoke (Hurley et al., 2023). Smoking is the main cause of Chronic Obstructive Pulmonary disease (Winnall et al., 2020). Smoking causes a disruption of the mucociliary clearance, cough and alveolar clearance systems in the lungs, which can lead to increased colonisation of bacteria and cause frequent infections (Winnall et al., 2020). Smoking also damages the lining of blood vessels, promotes the formation of atherosclerotic plaques, and reduces oxygen levels in the blood. It is one of the leading causes of coronary heart disease, stroke, and peripheral vascular disease (Briffa et al., 2021).
Substance abuse, including the use of illicit drugs and excessive alcohol, further compromises cardiopulmonary health. Stimulants such as cocaine and methamphetamine can cause acute cardiac events, arrhythmias, and sudden increases in blood pressure, while long-term use may lead to cardiomyopathy and respiratory depression. Inhaling and smoking of toxic chemicals such as glues and paints causes direct injury to the lungs and leads to permanent damage (Ingham-Broomfield, 2021).
Environmental Influences
Environmental stressors can significantly affect cardiopulmonary function, particularly in urban settings where exposure to pollutants and noise is more concentrated. Living in cities intensifies these stressors, with air pollution being a major concern. Fine particulate matter and gases such as nitrogen dioxide and sulphur dioxide, often released from vehicle exhaust and industrial activity, can penetrate deep into the lungs, causing inflammation, reduced lung function, and increasing the risk of respiratory and cardiovascular diseases (Eckhardt & Wu, 2021).
Noise pollution, especially from traffic, is another urban environmental factor that can elevate stress levels. Chronic exposure to noise activates the sympathetic nervous system, contributing to hypertension, myocardial infarction (MI), and stroke (Münzel et al., 2021).
In occupational settings, environmental exposure is also a concern. Workers in industries such as mining and construction may be exposed to silica dust, increasing the risk of silicosis, while coal miners are at risk for pneumoconiosis (“black lung”). Asbestos exposure, still a concern in older buildings and infrastructure, is linked to mesothelioma, a rare but aggressive form of lung cancer.
 |
Cultural Influences Cultural and social determinants play a significant role in cardiopulmonary health outcomes across diverse populations in Australia. Aboriginal and Torres Strait Islander (ATSI) peoples experience disproportionately higher rates of hypertension, a key risk factor for cardiovascular disease, compared to non-Indigenous Australians (Buckley, 2019). This disparity is influenced by a complex interplay of factors, including historical disadvantage, limited access to culturally safe healthcare, socioeconomic inequality, and environmental stressors. Additionally, higher rates of smoking, poor nutrition, and chronic stress contribute to increased cardiopulmonary risk. Culturally responsive care that respects community values, supports self-determination, and integrates traditional knowledge is essential to improving health outcomes in ATSI communities.
|
Life Span Considerations
 |
Infants and Toddlers Infants’ and toddlers’ respiratory and cardiovascular systems are still developing, making them particularly vulnerable to oxygenation and perfusion compromise. The airways are smaller and more easily obstructed, and they have fewer alveoli, which limits gas exchange. The diaphragm is the primary muscle of respiration, and fatigue can quickly lead to respiratory distress. Additionally, infants have a higher metabolic rate and oxygen demand, but less efficient oxygen delivery due to immature haemoglobin and limited cardiac reserve. Monitor for signs of hypoxia, such as nasal flaring, grunting, and cyanosis.
|
 |
Older Adults Older adults experience structural and functional changes in the cardiopulmonary systems that can reduce efficiency. The heart muscle becomes stiffer, and valves may thicken, leading to reduced cardiac output and increased risk of murmurs and dysrhythmias. Baroreceptor sensitivity declines, contributing to orthostatic hypotension. In the lungs, elastic recoil decreases, and the chest wall becomes more rigid, reducing lung compliance and ventilation efficiency. These changes, combined with a slower immune response and reduced red blood cell production, make older adults more susceptible to hypoxia, anaemia, and respiratory infections.
|
Assessment of Cardiopulmonary Functioning

Focused Cardiopulmonary Assessment
A combined cardiac and respiratory-focused assessment is essential for evaluating cardiopulmonary function. The following outlines key assessment criteria; refer to the relevant sections in Health Assessment, part 3: Physical Health Assessment – Systems-Based/Focused Assessment for detailed procedures.
- Focused cardiac assessment
The cardiac assessment should focus on identifying signs of impaired circulation, perfusion, or conduction. Assess the pulse for quality, regularity, and strength. Inspect the limbs for colour and warmth, which may indicate peripheral perfusion status. Auscultate the heart to detect any abnormal heart sounds, such as murmurs. To assess for conduction abnormalities, perform a 12-lead electrocardiogram (ECG).
Refer to Part 3: Health Assessment – Cardiac - Focused respiratory assessment
The respiratory assessment should aim to detect signs of reduced ventilation and perfusion. In addition to measuring respiratory rate, observe the depth and regularity of breathing, symmetry of chest movement, and the use of accessory muscles. Note the patient’s preferred position, breathing patterns (e.g., pursed lips, gasping, apnoeic pauses), and any signs of anxiety. Auscultate lung fields for adventitious breath sounds, which may indicate fluid accumulation or airway obstruction.
Refer to Part 3: Health Assessment – Respiratory
Common Cardiopulmonary Diagnostic Tests
Haemoglobin (Hb)
This test measures the concentration of haemoglobin in a blood sample and is a key indicator of the blood’s oxygen-carrying capacity.
Arterial blood gas (ABG)
ABG testing offers important data in relation to acid-base balance. ABGs are considered an invasive procedure and are often reserved for those with severe disturbance. They are collected via puncture from the radial or femoral artery and drawn into a specialised heparinised syringe. If the result is not able to be analysed immediately (at point of care), it must be placed on ice for transport to the pathology laboratory. Refer to the Fluid, Electrolyte and Acid Base chapter for more information on ABGs.
Cultures
To determine if a bacterial infection is contributing to a patient’s illness, various cultures may be collected, including blood, sputum, urine, or swabs from a wound or throat. In an unwell patient, it is preferable to collect a culture before commencing antibiotic therapy; however, this should not delay the commencement of therapy (Mondor & Kourouche, 2024). Empirical antibiotic therapy is used until the specific organism and its antibiotic sensitivities can be confirmed.
- Sputum culture and sensitivity: Sputum is the mucous secretion from the lungs, bronchi, and trachea, and is not produced in a healthy individual. To gain a sputum sample, the individual must cough deeply to bring up sputum into the mouth and then transfer it into a specimen container. An attempt should be made to avoid contaminating the specimen with saliva, which may compromise results. Specimen is often collected first thing in the morning, as it tends to accumulate in the lungs when laying down for a period of time.
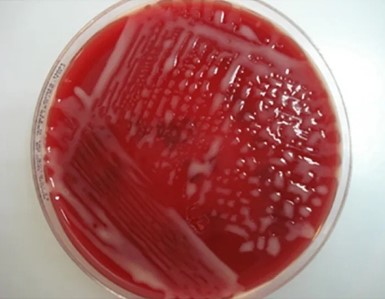
- Blood cultures: Blood cultures are ordered when sepsis is suspected. With some infections, pathogens are only found in the blood intermittently, so a series of three or more blood cultures, as well as blood draws from different veins, may be performed to increase the chance of finding the infection. Blood cultures are incubated for several days before being reported as negative. Some types of bacteria and fungi grow more slowly than others and/or may take longer to detect if initially present in low numbers.

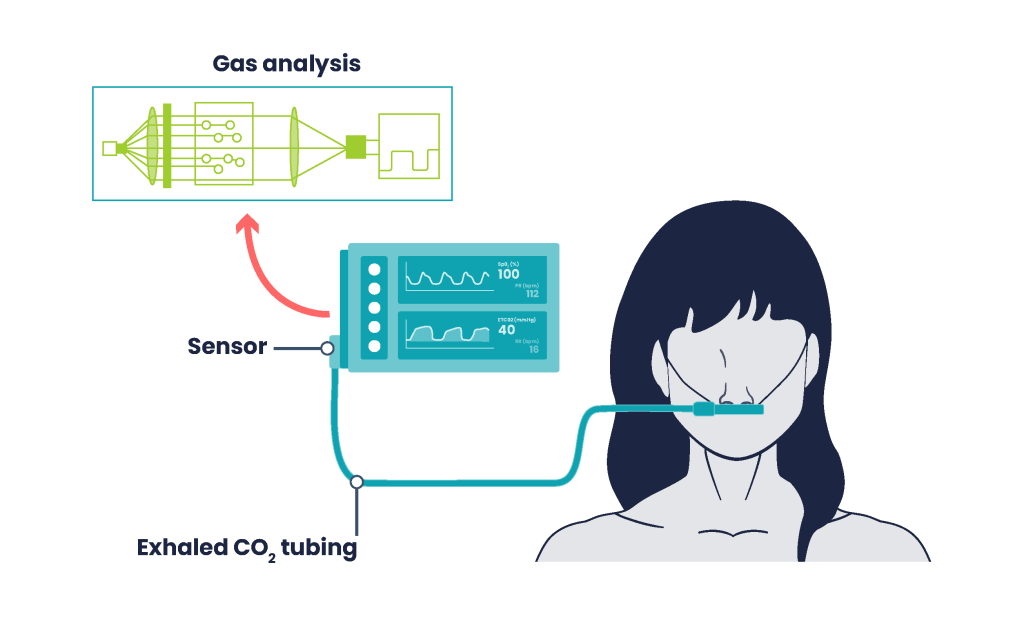
Capnography
Capnography involves noninvasive measurement of CO2. Expired gases are sampled from the patient’s airway and measured with an adapter attached to the endotracheal tube, tracheostomy tube or nasal cannula with a side stream cap (Bonaduce et al., 2024).
Pulse Oximetry
A pulse oximeter is a noninvasive device placed on the finger that is able to read the saturation of haemoglobin using an infrared light. When considering the results, it is important to remember the relationship between haemoglobin and oxygen, recalling that each haemoglobin molecule can carry up to four molecules of O2. A normal saturation level is considered between 94-98% SpO2. Refer to Health Assessment, part 2: Vital signs on the correct usage of a pulse oximeter.

|
Note: In patients with chronic respiratory disease such as COPD or emphysema, lower levels are tolerated with acceptable parameters, approximately 88%-92% (Barnett et al., 2022). Facility policy may vary, therefore acceptable parameters should be verified before any adjustments are made. |
Additional diagnostics may include chest radiographs (x-rays), computed tomography or magnetic resonance imaging, ventilation-perfusion (V/Q) scan, and a variety of pulmonary function tests, depending on the diagnosis being explored.
Electrocardiogram (ECG)
Electrocardiograms (ECGs) use leads with electrodes attached to the patient’s body to record the electrical activity of the heart on special graph paper or on a cardiac monitor. These electrodes detect the small electrical changes of cardiac muscle depolarisation followed by repolarisation during each cardiac cycle. The standard electrocardiograph (the instrument that generates an ECG) uses 3, 5, or 12 leads. The greater the number of leads an electrocardiograph uses, the more information the ECG provides.
Management of Alterations in Cardiopulmonary Functioning
Encourage Breathing Techniques
There are several breathing exercises a nurse can teach a patient to use to enhance ventilation and oxygenation. These techniques include pursed-lip breathing, diaphragmatic breathing, incentive spirometry, and deep breathing and coughing (DB&C).
Pursed-Lip Breathing
Pursed-lip breathing is a technique that allows people to control their oxygenation and ventilation. The technique requires a person to inspire through the nose and exhale through the mouth at a slow, controlled flow. This type of exhalation gives the person a puckered or pursed appearance. By prolonging the expiratory phase of respiration, a small amount of positive end-expiratory pressure is created in the airways that helps to keep them open so that more air can be exhaled, thus reducing air trapping that occurs in some conditions such as COPD. Pursed-lip breathing often relieves the feeling of shortness of breath, decreases the work of breathing, and improves gas exchange.
 |
||||||||||||
|
Diaphragmatic Breathing
Diaphragmatic breathing, also known as abdominal breathing, is a technique that encourages deeper and slower breaths by engaging the diaphragm rather than the chest muscles. It is helpful for patients who are tachypneic due to physiological stress or anxiety. The technique promotes relaxation, improves oxygenation and enhances respiratory efficiency. The nurse teaches the patient how to become aware of their breathing pattern and intentionally shift from shallow chest breathing to deeper abdominal breathing.
 |
||||||||||||
|
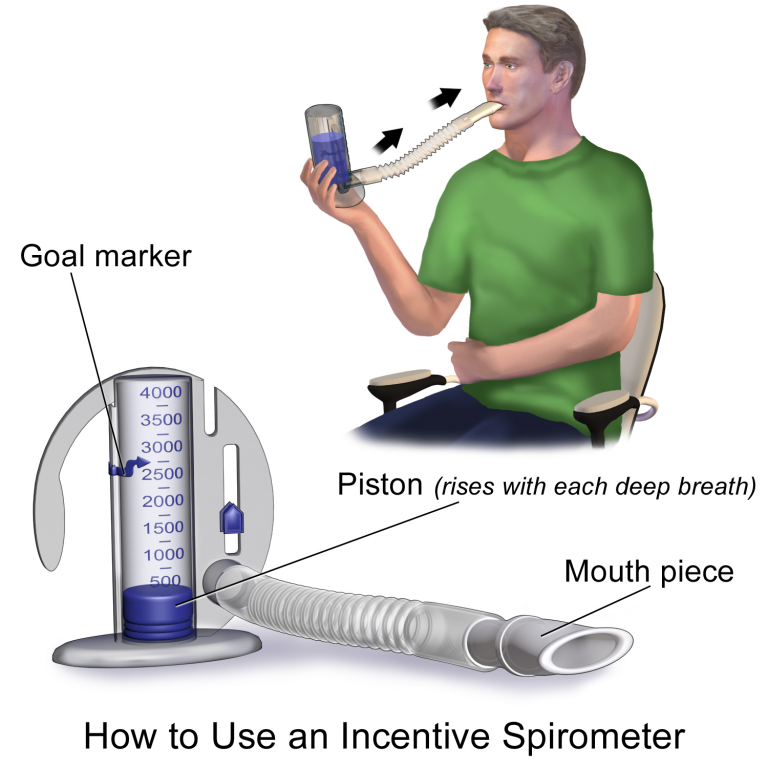
Incentive Spirometry
An incentive spirometer is a handheld device commonly prescribed for those with decreased mobility, a respiratory illness or after surgery. It is aimed at preventing complications such as atelectasis, sometimes referred to as lung collapse, which occurs when alveoli become deflated or filled with fluid, placing the patient at high risk of developing pneumonia. The spirometer provides visual feedback to help patients take slow, deep breaths. While sitting upright, the patient should breathe in slowly and deeply through the tubing with the goal of raising the piston to a specified level. The patient should attempt to hold their breath for five seconds, or as long as tolerated, and then rest for a few seconds. This technique should be repeated by the patient ten times every hour while awake.
Incentive Spirometry Teaching Guide
 |
||||||||||||||
|
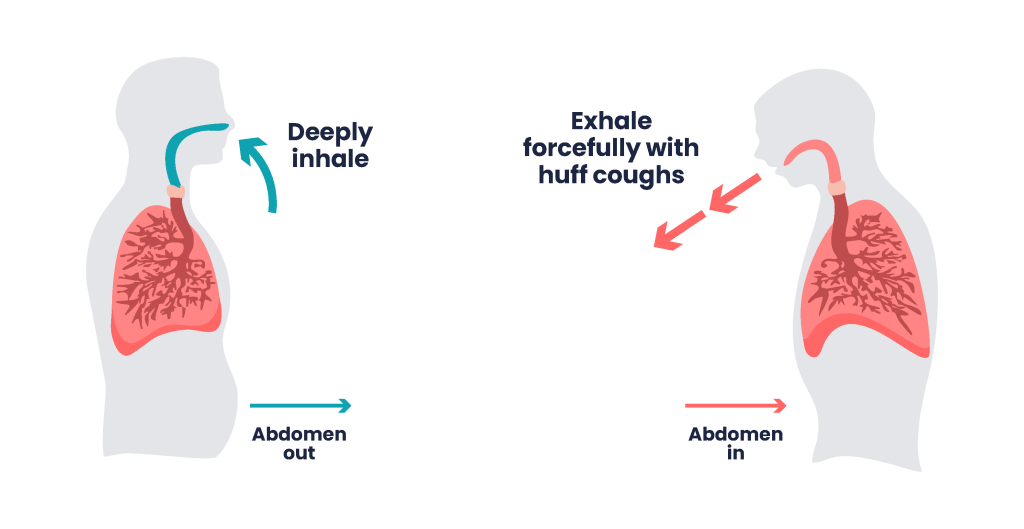
Deep Breathing and Coughing
Deep breathing and coughing helps open the alveoli, improves oxygenation, and prevents complications such as atelectasis. Coughing assists in mobilising and removing mucus from the lower respiratory tract, promoting airway clearance.
Regular, controlled deep breathing followed by effective coughing can reduce painful, uncontrolled coughing episodes that are often ineffective. One recommended method is the huff cough, a controlled technique that helps clear secretions without straining the airways.
Deep Breathing with Huff Cough Teaching Guide
 |
||||||||||||||||
|
Positioning
Proper patient positioning plays a vital role in enhancing lung expansion, improving oxygenation, and reducing the work of breathing. Two key positions commonly include High Fowler’s position and the Orthopnoeic position (also known as the tripod position).
 |
High Fowler’s Position
Raising the head of the bed to a 90-degree angle (High Fowler’s) promotes maximum thoracic expansion. This position facilitates deeper inhalation, reduces pressure on the lungs from abdominal organs, and decreases the effort required to breathe. It is especially beneficial for patients experiencing dyspnoea or recovering from abdominal or thoracic surgery. If the high Fowler’s position is not tolerated or contraindicated, a semi-Fowler’s (45-degree) position may be employed. |
|
|
Orthopnoeic Position
The orthopnoeic position involves the patient sitting or standing, leaning forward while resting their arms on a bedside table or knees. Pillows are commonly placed over the table for additional support. The posture takes on a tripod effect, allowing gravity to assist in opening the chest cavity, expanding the lungs and reducing accessory muscle work. It is commonly used by patients with chronic obstructive pulmonary disease (COPD) or acute respiratory distress, as it helps ease breathing and enhances oxygen intake. |
Oxygen Therapy
Key Takeaways
In this chapter, we covered:
- Oxygenation and perfusion rely on the coordinated function of the respiratory and cardiovascular systems to deliver oxygen to tissues and remove carbon dioxide.
- Ventilation/perfusion mismatch, hypoxia, and hypoxaemia are critical indicators of impaired gas exchange and require early recognition through clinical assessment and monitoring tools such as SpO₂ and ABGs.
- Lifestyle factors such as poor diet, sedentary behaviour, environmental exposures, stress and anxiety, smoking/substance abuse can significantly impact cardiopulmonary health and contribute to chronic disease.
- Cardiopulmonary investigations such as chest X-rays, ECGs, and ABGs provide essential diagnostic information and guide treatment decisions in patients with respiratory or cardiac compromise.
- Electrocardiogram (ECG) interpretation is a foundational skill for nurses, enabling early detection of arrhythmias and cardiac dysfunction that may affect perfusion.
- Oxygen therapy must be tailored to the patient’s clinical condition, with careful consideration of flow rate, FiO₂, humidification, and safety precautions to avoid serious complications.
- Understanding oxygen delivery devices, including nasal cannula, Venturi masks, non-rebreather masks, and high-flow systems, is essential for selecting the appropriate method and ensuring safe, effective care.
References
Australian Commission on Safety and Quality in Health Care. (2025). Documenting oxygen therapy and response for safety. https://www.safetyandquality.gov.au/publications-and-resources/resource-library/documenting-oxygen-therapy-and-response-safety
Barnett A., Beasley R., Buchan C., Chien J., Farah C. S., King G., McDonald, C. F., Miller, B., Munsif, M., Psirides, A., Reid, L., Roberts, M., Smallwood, N., & Smith, S. (2022). Thoracic Society of Australia and New Zealand position statement on acute oxygen use in adults: ‘Swimming between the flags’. Respirology, 27(4), 262–276. https://doi.org/10.1111/resp.14218
Betts, J. G., Kelly A. Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M. & DeSaix, P. Anatomy and physiology 2e. Openstax. https://openstax.org/details/books/anatomy-and-physiology-2e
Bonaduce, S. J. (Writer), Kourouche, S. & Buckley, T. (adaptors). (2024). In D. Brown, T. Buckley, R. Aitken, & H. Edwards (Eds). Lewis’s medical-surgical nursing: Assessment and management of clinical problems (6th ed., Australian and New Zealand ed., pp 568-593). Elsevier.
Briffa, T., Greenhalgh, E. M. & Winstanley, M. H. (2021). 3.1 Smoking and cardiovascular disease. Cancer Council Victoria. https://www.tobaccoinaustralia.org.au/chapter-3-health-effects/3-1-smoking-and-cardiovascular-disease
Buckley, T. (2019). Alterations in cardiovascular function across the life span. In J. Craft, C. Gordon, S. E., Huether, K. L. McCance, V. L. Brashers & N. S. Rote. Understanding pathophysiology (3rd ed, Australian and New Zealand ed.). Elsevier Australia.
Eckhardt, C. M., & Wu, H. (2021). Environmental exposures and lung aging: Molecular mechanisms and implications for improving respiratory health. Current Environmental Health Reports, 8(4), 281–293. https://doi.org/10.1007/s40572-021-00328-2
Hurley, S., Winnall, W., Greenhalgh, E. M. & Winstanley, M. H. (2023). 3.4 Lung cancer. Cancer Council Victoria. https://www.tobaccoinaustralia.org.au/chapter-3-health-effects/3-4-lung-cancer
Ingham-Broomfield, B. (2021). Supporting oxygenation and perfusion. In Crisp, J., Douglas, C., Rebeiro, G., Waters, D., Potter & Perry’s fundamentals of nursing (6th ed, Australian & New Zealand ed, pp. 738-824). Elsevier.
Marieb, E. & Hoehn, K. (2023). Human anatomy and physiology (12th global ed.). Pearson.
Mondor, E. E. & Kourouche, S. (2024). Nursing management: Lower respiratory problems. In D. Brown, T. Buckley, R. Aitken, & H. Edwards (Eds). Lewis’s medical-surgical nursing: Assessment and management of clinical problems (6th ed., Australian and New Zealand ed., pp 617-658). Elsevier.
Mondor, E. E. (Writer) & Williams, E. (Adapter). (2024). Nursing management: Obstructive pulmonary diseases. In D. Brown, T. Buckley, R. Aitken, & H. Edwards (Eds). Lewis’s medical-surgical nursing: Assessment and management of clinical problems (6th ed., Australian and New Zealand ed., pp 659-709). Elsevier.
Münzel, T., Hadad, O., Sørensen, M., Lelieveld, J., Duerr, G. D., Nieuwenhuijsen, M., & Daiber, A. (2021). Environmental risk factors and cardiovascular diseases: A comprehensive expert review. Cardiovascular Research, 118(14), 2880–2902. https://doi.org/10.1093/cvr/cvab316
National Heart Foundation of Australia. Guideline for the diagnosis and management of hypertension in adults-2016. https://assets.contentstack.io/v3/assets/blt8a393bb3b76c0ede/bltbf3d36e10b48f01f/65b0963ea933e532ae0286de/01_Hypertension-guideline-2016_WEB.pdf
Sharma, S., Danckers, M., Sanghavi, D. K., Chakraborty, R. K. (2023). High-flow nasal cannula. In W. B. Ackley, T. S. Adolphe, T. C. Aeby, N. R. Aeddula, S. Agadi, P. Agasthi, S. Ahmad, A. Ahmed, F. W. Ahmed, I. Ahmed, R. A. Ahmed, S. W. Ahmed, A. M. Akanmode, R. Akella, S. M. Akram, Y. Al Khalili, E. Al Zaabi, M. H. Alahmadi, G. Alexander, … H. Zulfiqar (Eds). StatPearls. StatPearls Publishing. Retrieved January 2025, from https://www.ncbi.nlm.nih.gov/books/NBK526071/
Winnall, W. R., Peters, M., Greenhalgh, E. M. & Winstanley, M. H. (2020). 3.2 Respiratory diseases (excluding lung cancer). Cancer Council Victoria. https://www.tobaccoinaustralia.org.au/chapter-3-health-effects/3-2-respiratory-diseases
World Health Organization. (2025). Sodium reduction. https://www.who.int/news-room/fact-sheets/detail/sodium-reduction
Chapter Attribution
This chapter has been adapted in part from:
Clinical nursing skills (2024) by Christie Bowen et al., OpenStax, is used under a CC BY licence.
Medical-surgical nursing (2024) by Christy Bowen, Bridget Carey, Jessica Palozie and Maren Reinholdt, is used under a CC BY-NC licence.
Nursing skills 2e (2023) by Open Resources for Nursing, Chippewa Valley Technical College, is used under a CC BY licence.
Media Attributions
- Blood flow through the cardioplumonary system © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble and Peter DeSaix is licensed under a CC BY (Attribution) license
- Electrical pathway of the cardiac conduction system © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix adapted by Leisa Sanderson is licensed under a CC BY (Attribution) license
- Respiratory system Aveoli © Christy Bowen is licensed under a CC BY (Attribution) license
- Inhalation Exhalation © Christy Bowen is licensed under a CC BY (Attribution) license
- Diffusion of CO2 and O2 © Christy Bowen, Bridget Carey, Jessica Palozie & Maren Reinholdt is licensed under a CC BY (Attribution) license
- VQ Mismatch © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Oxygen-Carrying Capacity in Red Blood Cells © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Cardiopulmonary assessment square © George Coogan is licensed under a CC BY-NC (Attribution NonCommercial) license
- Arterial Blood Gas Testing © Eileen Siddins is licensed under a CC BY-NC (Attribution NonCommercial) license
- Sputum culture © National Library of Medicine adapted by Christy Bowen is licensed under a CC BY (Attribution) license
- Blood Cultures Green and orange © Leisa Sanderson is licensed under a CC BY-NC (Attribution NonCommercial) license
- CapnographyFigure © Eileen Siddens is licensed under a CC BY-NC (Attribution NonCommercial) license
- Pulse oximeter © George Coogan is licensed under a CC BY-NC (Attribution NonCommercial) license
- aid611002-v4-728px-Live-With-Chronic-Obstructive-Pulmonary-Disease-Step-8 © WikiHow adapted by Ernstmeyer & Christman - Open Resources for Nursing (Open RN) is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- DiaphragmaticBreathingFigure-ESpng © Eileen Siddens is licensed under a CC BY-NC (Attribution NonCommercial) license
- Incentive_Spirometer-768×768 © BruceBlaus is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- CoughingFigure ES © Eileen Siddens is licensed under a CC BY-NC (Attribution NonCommercial) license
- Hudson mask application © Penny Coogan is licensed under a CC BY-NC (Attribution NonCommercial) license
- Tripod position square © Ben Green is licensed under a CC BY-NC (Attribution NonCommercial) license


