2.3 Communication – SPIKES
SPIKES – Delivering Bad News
 |
 |
 |
The dynamic and ever-expanding role of pharmacists gives rise to situations where, as trusted healthcare professionals, we are responsible for the holistic care of patients well beyond the provision of medications. One such responsibility includes delivering or discussing bad news. Bad news can be described as an undesirable, unfortunate or unwanted circumstance. In a healthcare setting, this may relate to the diagnosis of a disease, poor prognosis, limited treatment options for a condition, or a decline in the overall health of a patient. Pharmacists are highly accessible to the community. Therefore, it is essential to be prepared for these difficult conversations.
Patients may share bad news with their pharmacist that they have received from another health professional. For example, a recent cancer diagnosis or news about a spouse, family member or friend experiencing a significant cardiac event. In addition to supporting people who have received bad news, pharmacists often deliver bad news or information that is inconvenient, distressing, upsetting or disappointing. Pharmacists may need to communicate to a patient regarding the progression of disease; counsel a patient on the diagnosis of a chronic condition requiring lifelong medication; or provide information about out-of-stock items or medication shortages.
Pharmacists often rely on guidelines and well-defined treatment protocols which provide relative certainty to their scope of practice. It is important to acknowledge in situations of dealing with bad news there may be much less certainty for the people involved. As a result, a compassionate, holistic, patient-centred approach is paramount.
Some important skills for pharmacists delivering or discussing bad news include:
- Accepting the complexity and ambiguity of a patient’s journey or situation
- Expecting a wide range of emotions from the patient (eg: grief, loss, sadness, anxiety etc)
- Showing respect for patients’ beliefs (consider emotional, physical, spiritual and social factors)
- Being prepared for patients to ask difficult questions or share sensitive information.
Pharmacists should remember to:
- Have a patient-centred approach because every person’s journey is unique.
- Use open communication and active listening.
- Consider body language; level and tone of voice; and the privacy of the conversation.
- Acknowledge the trust the patient has put in you by sharing difficult news.
- Develop knowledge of appropriate referral pathways for continuity of care and safety-netting for those patients who require further support.
The SPIKES Protocol
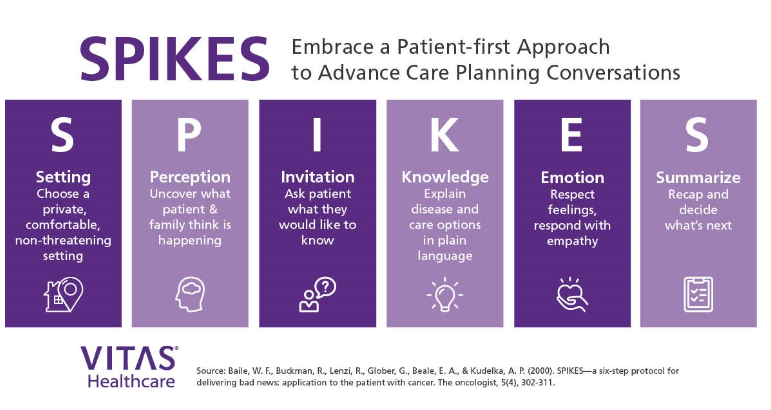
SPIKES stands for: Setting, Perception, Invitation, Knowledge, Emotions/Empathy, and Strategy/Summary.
Consider the following steps in the SPIKES protocol relevant to pharmacy practice:
Using the SPIKES Protocol as pharmacist
Traditionally, the SPIKES model is used in the context of Advanced Care Planning for cancer patients or in the Palliative Care setting. The following image is adapted by VITAS Healthcare as a tool for conversations between healthcare professionals and patients and their families regarding bad news. Now let’s consider how this tool can be adapted to scenarios encountered by a pharmacist.
Case Study 1 – An empathetic interaction between a pharmacist and a patient with a poor cancer prognosis using the SPIKES Protocol
Pharmacist: Emma, a compassionate and experienced pharmacist trained in the SPIKES protocol
Alexander visits Emma at the pharmacy, visibly upset and distressed. Emma immediately acknowledges his emotional state and offers a private consultation room.
Key Points:
- Emma uses the SPIKES protocol to deliver empathetic and patient-centred care.
- She creates a safe environment, actively listens, and validates Alexander’s feelings.
- Emma focuses on improving Alexander’s quality of life, rather than just treating his symptoms.
Alexander leaves the pharmacy feeling more supported and empowered to face his prognosis. Emma has helped him explore palliative care options and adjust his medication to minimize side effects. Their interaction demonstrates the importance of empathetic communication in healthcare, particularly in difficult situations.
Reflection:
Emma’s use of the SPIKES protocol has made a significant difference to Alexander’s experience. By acknowledging his emotional state and offering support, Emma has built trust and helped Alexander feel more in control of his situation. This interaction highlights the value of patient-centred care and the impact pharmacists can have on patients’ lives beyond dispensing medication.
Case Study 2 – Delivering bad news about medication unavailability using the SPIKES protocol
Patient: 75-year-old male, Michael, with chronic conditions (hypertension, diabetes, and arthritis)
Pharmacist: Greg, an experienced pharmacist trained in the SPIKES protocol
Michael visits Greg at the pharmacy to collect his regular medications. Greg has just received notification of a shortage of several crucial medications, including Michael’s blood pressure and diabetes medications.
Key Points:
- Greg uses the SPIKES protocol to deliver bad news about medication unavailability in a compassionate and structured manner.
- He assesses Michael’s understanding, invites him to receive the information, and provides clear knowledge.
- Greg offers empathy and support, helping Michael cope with the news.
Outcome:
Michael leaves the pharmacy feeling informed and supported, with a plan in place to manage his medications. Greg’s use of the SPIKES tool has helped deliver bad news in a way that maintains trust and respect.
Reflection:
Greg’s application of the SPIKES protocol demonstrates effective communication in difficult situations. By being empathetic and structured, Greg has helped Michael navigate a challenging moment, showcasing the value of pharmacist-patient relationships in delivering holistic care.
Case Study 3 – Watch this video which exemplifies a pharmacist using the SPIKES protocol in practice
📚 Read/Explore
Reflect on the use of SPIKES in the Case Studies
Consider how you might navigate situations like the above case studies if you were working as a pharmacist. Would you approach these encounters any differently? If so, how? How would your own knowledge and experience impact your interaction with the patient? What would you do if you felt the patient needed further support beyond what you could provide?
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
