8.5 Inhaler Devices and Technique
Inhaler Devices
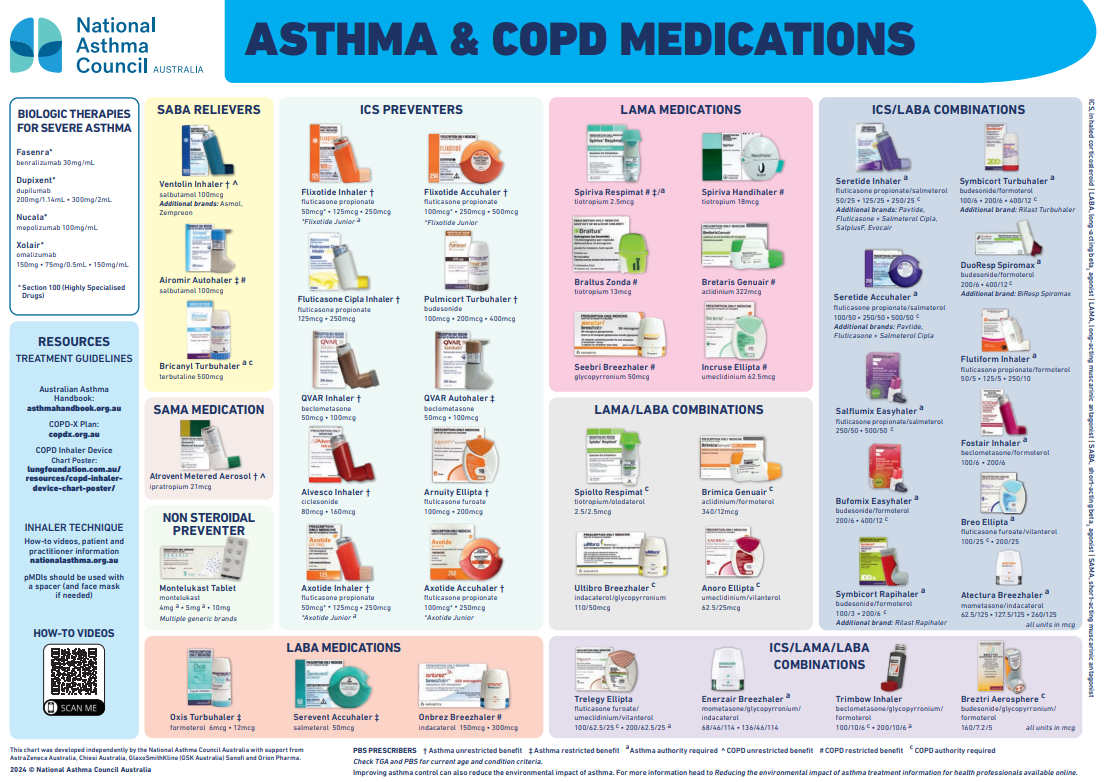
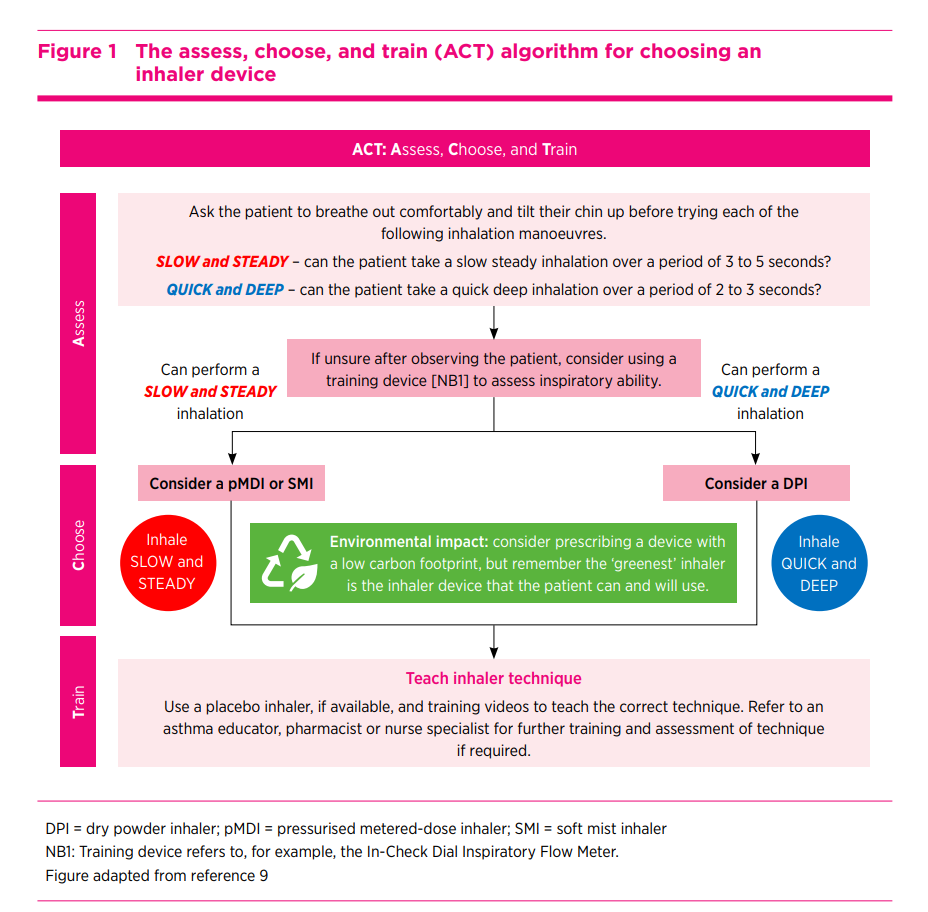
There are many types of inhaler devices, and each device has advantages and disadvantages. Patients need an individualised assessment that considers factors such as the patient’s inspiratory flow rate and volume, dexterity, inhaler regimen complexity and environmental impact before an inhaler device is chosen and prescribed. The following algorithm is taken from an Australian Prescriber article and can be used by prescribers to assist in choosing an inhaler device. The article can be found here: p140-Rigby
This table provides additional considerations for choice of inhaler device type when prescribing inhaled medicines. It’s good to know as you may need to suggest an inhaler device to a prescriber. Or, you may be prescribing inhaled medicines as an accredited pharmacist in the North Queensland Community Pharmacy Full Scope of Practice Pilot!
|
Clinical Situation |
Consideration |
|
Acute Asthma |
Recommend use of spacer when using reliever pMDI for acute asthma |
|
Any patient using a pMDI for an inhaled corticosteroid |
Recommend use of a spacer every time (except for breath-acuated pMDIs) |
|
Infants and small children |
Use a spacer with a facemask |
|
Poor manual dexterity (e.g. weak hands or arthritis) |
Consider either of: > a Haleraid device with relevant pMDIs (available for salbutamol, fluticasone, fluticasone/salmeterol) > a breath-actuated inhaler |
|
Difficulty connecting spacer to pMDI (e.g. elderly patient with weakness or poor coordination) |
Leave spacer connected: pharmacist can attach spacer to inhaler each time canister is replaced, and leave attached until medicine is used up. (If patient uses more than one pMDI, provide a separate spacer for each device Consider a breath-actuated inhaler. |
|
Inability to form a good seal around the mouthpiece of the inhaler or spacer (e.g. person with cognitive impairment or facial weakness) |
Consider a spacer plus age-appropriate facemask |
|
Difficulty speaking or reading English |
Give a physical demonstration Use videos Use an interpreter or provide written instructions in the person’s first language |
|
Using multiple inhalers |
Choose the same type for each medicine, if possible, to avoid confusion If not possible, train person in the correct inhaler technique for each of their devices, emphasizing any key differences (e.g. speed of inhalation, shake pMDIs but not dry-powder inhalers) |
Inhaler Technique
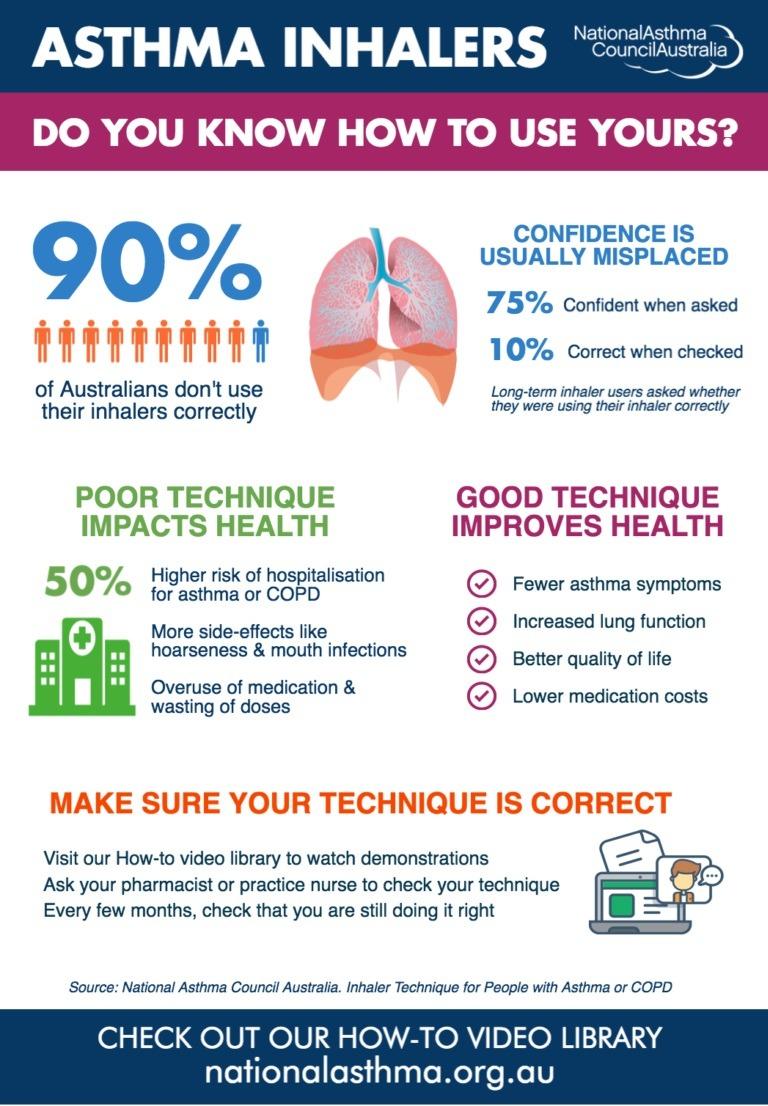
Up to 90% of Australians do not use correct inhaler technique. Poor inhaler technique results in poor control and flare-ups. Repeated hands-on training in correct inhaler use should be emphasised at every interaction with patients. If patients require multiple inhaled drugs, combination inhalers should be prescribed to reduce errors in inhaler technique and improve adherence.
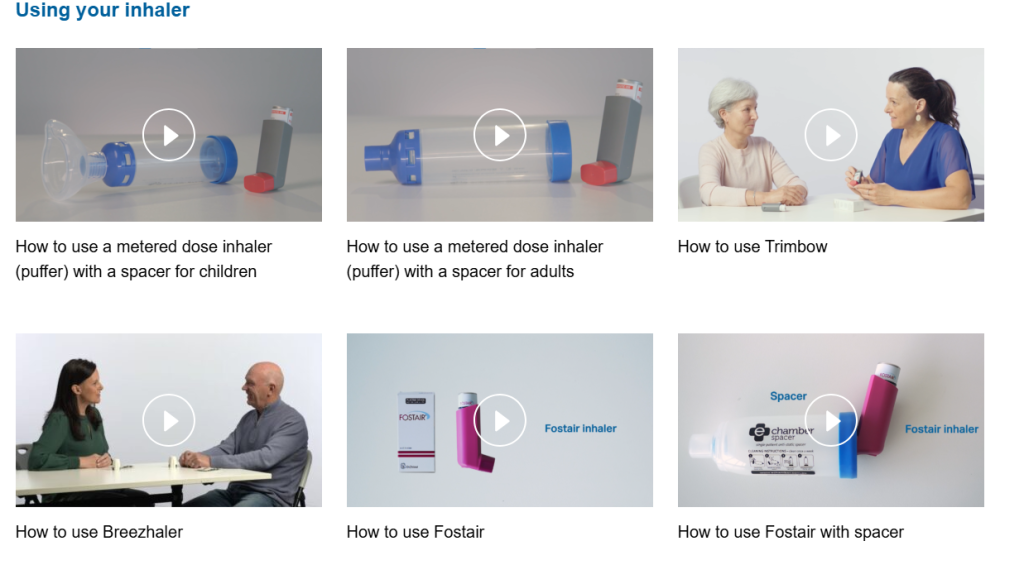
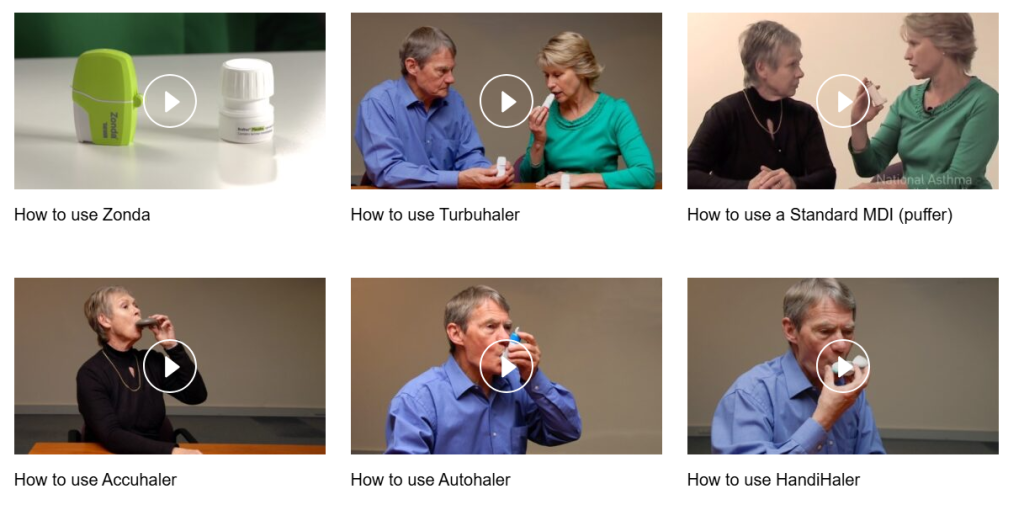
Use this link to access a library of videos published by the National Asthma Council which demonstrate correct inhaler technique: https://www.nationalasthma.org.au/living-with-asthma/how-to-videos
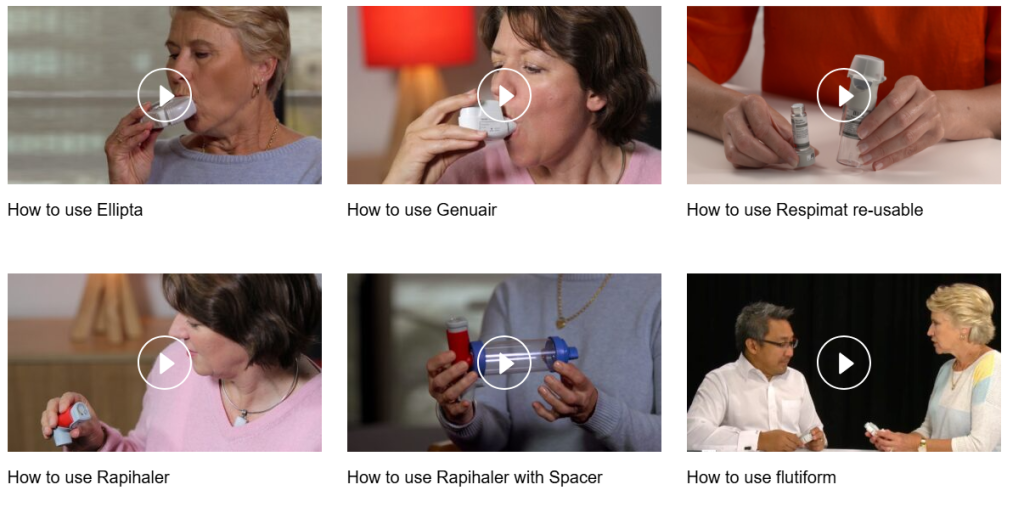
 We will review the use of these in devices in the GLS so you can become familiar with them, but you will need to practice, practice, practice at every opportunity on the use of:
We will review the use of these in devices in the GLS so you can become familiar with them, but you will need to practice, practice, practice at every opportunity on the use of:
- pMDI
- pMDI + spacer
- Autohaler
- Turbuhaler
- Accuhaler
- Handihaler
- Respimat
- Spacers.
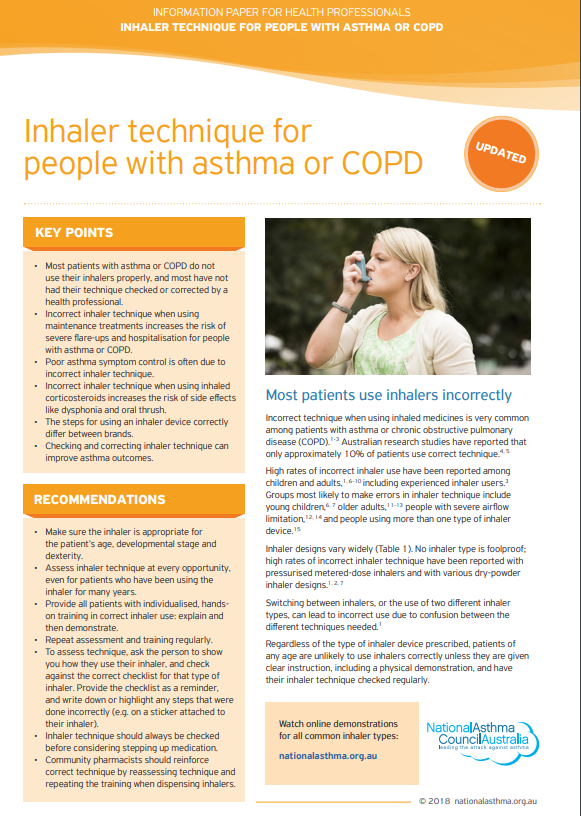
This information paper is for health professionals to assist in counselling on good inhaler technique in patients with asthma or COPD (discussed next week). It is available here: Inhaler-Technique-info-paper-20180607-web
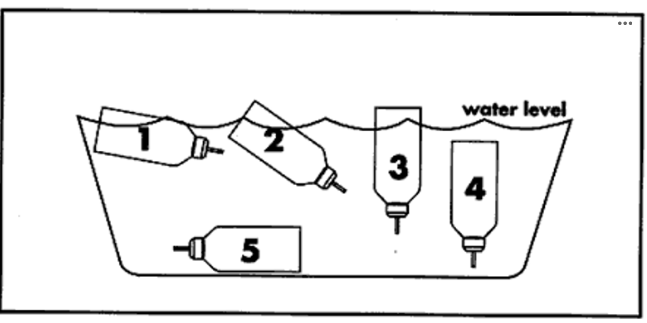
How do you know when an inhaler is empty? If you are unsure go back to the video in Chapter 8.3.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.