2.1 The Story of Blood Pressure Regulation: Keeping the Body in Balance
Blood Pressure Regulation
 |
 |
 |
Imagine the human body as a bustling city, with its cardiovascular system acting as a complex network of roads ensuring vital resources are delivered efficiently. Just like a city needs effective traffic control, the body relies on precise blood pressure regulation to maintain homeostasis. Here’s the fascinating story of how our body achieves this delicate balance.
Play this track, turn it up and keep reading!
Central Command: The Brain and Heart
In this story, the brain and heart are the central command centres. The brain constantly monitors the body’s needs and sends signals to the heart to adjust its pumping action. The heart, in turn, modulates the force and rate of its beats to ensure optimal blood pressure, ensuring all organs receive the blood they need.
Sensory Network: The Baroreceptors
Scattered along the walls of major arteries, such as the aorta and carotid arteries, are baroreceptors, the body’s surveillance cameras. These specialized sensors continuously monitor arterial pressure. When there’s a rise or drop in blood pressure, baroreceptors detect these changes and alert the brain to initiate corrective actions.
Rapid Response: Sympathetic and Parasympathetic Systems
Upon receiving signals from baroreceptors, the brain activates its rapid response teams: the sympathetic and parasympathetic nervous systems. The sympathetic system, akin to a city’s emergency response unit, springs into action when blood pressure drops. It releases catecholamines (like adrenaline and noradrenaline) to increase heart rate and constrict blood vessels, raising blood pressure. Conversely, the parasympathetic system, like a calming influence, slows the heart rate and dilates blood vessels when blood pressure is too high, helping to lower it.
Long-Term Regulation: The Kidneys and Hormones
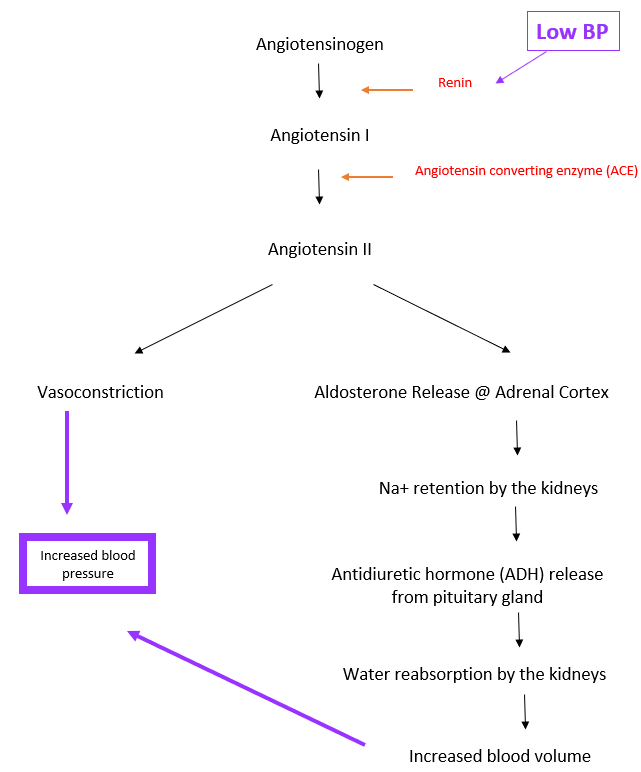
For long-term blood pressure regulation, the kidneys and various hormones play a crucial role. The kidneys adjust blood volume by regulating the amount of sodium and water excreted. Hormones like aldosterone and antidiuretic hormone (ADH) help the kidneys retain sodium and water, increasing blood volume and pressure. Conversely, natriuretic peptides help excrete sodium and water, reducing blood volume and pressure.
This intricate system of checks and balances ensures that blood pressure remains within a healthy range, enabling the body to function optimally. By coordinating the actions of the brain, heart, blood vessels, kidneys, and hormones, the body maintains a stable internal environment, much like a well-governed city ensures smooth traffic flow and resource distribution.
The Relationship Between Blood Pressure and Blood Flow
 |
 |
 |
Blood moves from areas of higher pressure to lower pressure, with greater pressure differences resulting in increased blood flow. The ventricles’ contraction generates blood pressure (BP), which is the force exerted by blood on vessel walls. BP is influenced by cardiac output, blood volume, and vascular resistance.
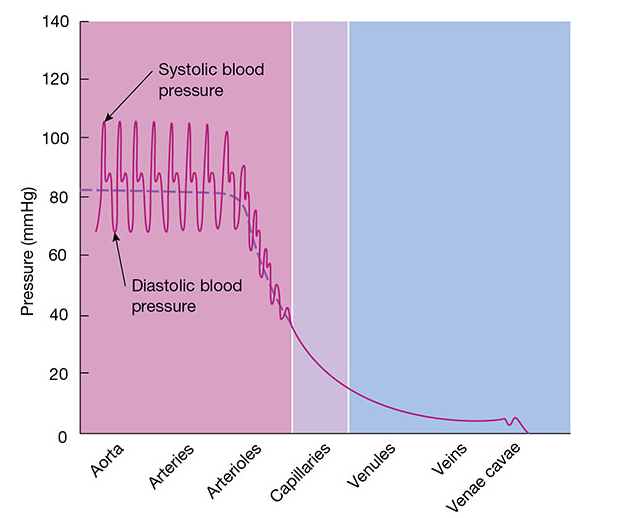
In the aorta and large systemic arteries, BP is highest. For a resting young adult, BP peaks at around 110 mmHg during systole (ventricular contraction) and drops to approximately 70 mmHg during diastole (ventricular relaxation). Systolic blood pressure (SBP) is the maximum pressure in arteries during systole, while diastolic blood pressure (DBP) is the minimum pressure during diastole.
As blood exits the aorta and travels through the systemic circulation, pressure gradually decreases with increasing distance from the left ventricle. BP falls to about 35 mmHg as blood moves from systemic arteries to arterioles and capillaries, where pressure fluctuations cease. At the venous end of capillaries, BP drops further to around 16 mmHg and continues to decrease in venules and veins, ultimately reaching 0 mmHg as blood enters the right ventricle.
What is blood pressure and why is it important?
Blood pressure is the pressure that is exerted by the blood upon the walls of the arteries. It is influenced by a number of variables, including efficiency of the heart muscle, blood volume and viscosity, and the condition of the blood vessel walls.
Homeostatic mechanisms play an important role in keeping blood pressure within a normal quantifiable range. A blood pressure that is too low results in inadequate tissue perfusion with oxygen and nutrients. On the other hand, a blood pressure that is too high can result in damage to the coronary arteries as well as the fragile vessels of end-organs like the kidneys and the eyes. High blood pressure also causes the heart to work harder with every beat to push blood out into the systemic circulation, hence hypertension is also a risk factor for heart failure.
The CNS consists of the brain and spinal cord, and the peripheral nervous system consists of nerves that run to the rest of the body.
If you know that blood pressure is the product of cardiac output and systemic vascular resistance, then you will be in a good position to extrapolate some of the factors that influence blood pressure. If you understand this, then the treatment of hypertension will be straightforward.
Short-term regulation of blood pressure
Blood pressure is normally regulated in the short term to ensure that adequate blood flow is maintained to the brain despite behavioural, emotional, and physiological changes. This is achieved primarily by activation of the sympathetic nervous system, which functions to increase BP by increasing both heart rate and systemic vascular resistance. The SNS neurotransmitters adrenaline and noradrenaline bind to:
- β1 receptors within the heart causing increased rate of firing of the sinoatrial node
- α1 receptors on smooth muscles of the arterial vessels causing vasoconstriction
Longer-term regulation of blood pressure
Longer term control of blood pressure is closely associated with fluid volume homeostasis, which is primarily driven by the renin-angiotensin-aldosterone system.
Still, long-term regulation of BP is likely multifactorial. The Atrial Natriuretic Peptide (ANP) is another factor involved in the longer-term regulation of blood pressure. It is secreted in response to stimulation of stretch receptors when there is increased volume in the atria of the heart. It causes the kidneys to increase water and sodium excretion, leading to reduced circulating blood volume and reduced blood pressure.
Next, we consider a blood pressure that is too high – hypertension.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNINGThis material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.