2.2.3 Pharmacology of Common Drugs to Lower Cholesterol
Learning Outcomes
Be able to:
- Relate the mechanism of action of the statins, fibrates, ezetimibe, PSCK9 inhibitors and siRNAs to their cholesterol lowering effect.
- Describe the common and catastrophic side effects of the statins, fibrates, ezetimibe, PSCK9 inhibitors and siRNAs.
- Identify the potency of the 4 major lipid lowering drug therapies available in Australia.
HMG-CoA reductase inhibitors or “statins”
 |
 |
 |
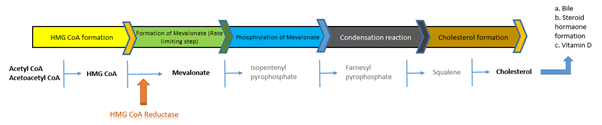
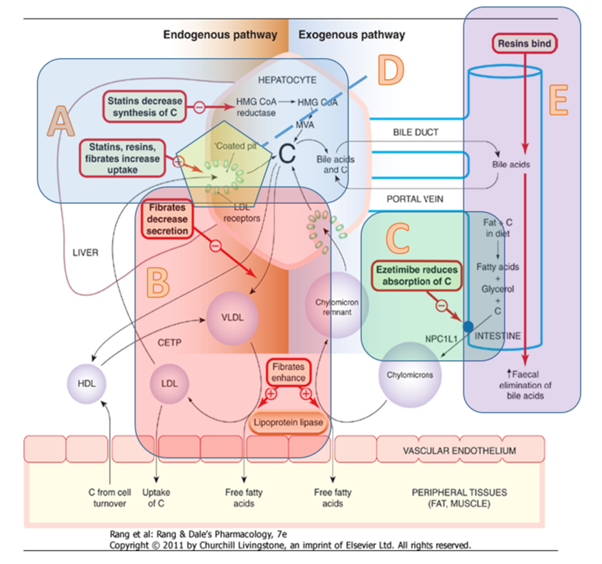
HMG-CoA reductase inhibitors or statins include atorvastatin, fluvastatin, pravastatin, rosuvastatin and simvastatin. They all share a common suffix – ‘statin’, hence they are collectively referred to as ‘statins’. Statins are reversible competitive inhibitors of the enzyme HMG-CoA reductase. The enzyme HMG-CoA reductase is a rate limiting step in the conversion of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) to mevalonate which eventually is used in the synthesis of cholesterol. The conversion of 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) to mevalonate is carried out in the liver and the statins block this conversion leading to reduced hepatic production.
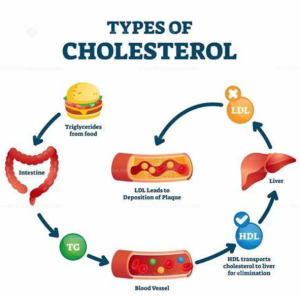
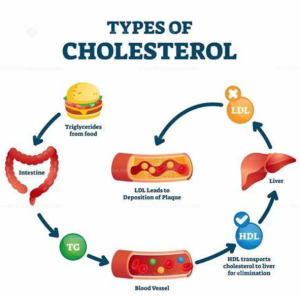
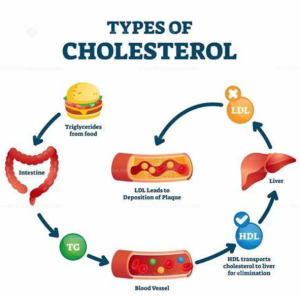
 Cholesterol is necessary for a broad range of physiological functions including the production of hormones, bile, cell membranes, catecholamines and other neurotransmitters. The supply of cholesterol is sourced via two main mechanisms (see figure below):
Cholesterol is necessary for a broad range of physiological functions including the production of hormones, bile, cell membranes, catecholamines and other neurotransmitters. The supply of cholesterol is sourced via two main mechanisms (see figure below):
- Production of endogenous cholesterol by the liver and
- Dietary consumption of cholesterol.
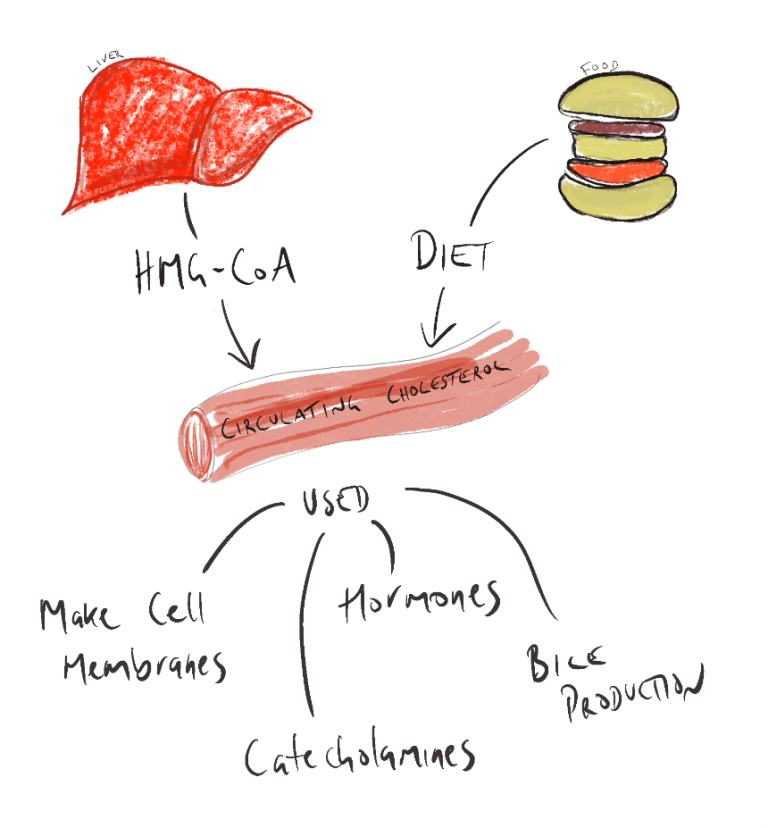
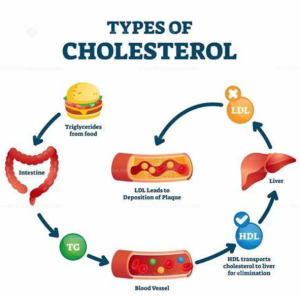
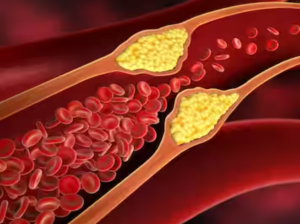
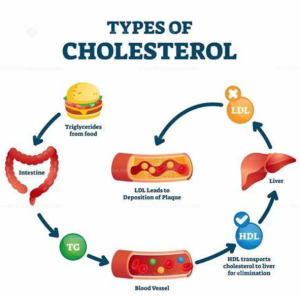
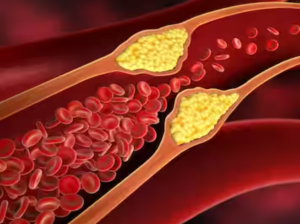
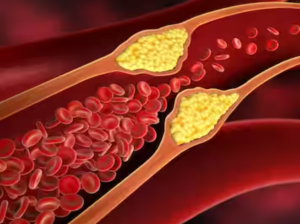
When dietary supply of cholesterol is in excess, statins can be used to reduce the endogenous (liver) production of cholesterol. Reduced liver production of cholesterol makes total blood cholesterol scarcer. More cholesterol is scavenged from the circulating blood thereby reducing circulating plasma cholesterol levels. Because there is less circulating cholesterol, there is a reduction of build-up of cholesterol containing fatty plaques is the arteries.
Common side effects of statins include myalgia, mild and transient GI symptoms, insomnia, nightmares, dizziness and elevated aminotransferase levels. Statins are associated with myalgia, myopathy and a particularly serious expression of myalgia – rhabdomyolysis.
Rhabdomyolysis is the breakdown of skeletal muscle fibers with the resultant degraded products released into the bloodstream. Symptoms of rhabdomyolysis included:
- severe unexplainable severe muscle pain – typically in the larger muscles
- muscle weakness
- dark brown or red urine.
This may be accompanied by reduced urine output. While rare, rhabdomyolysis is a serious condition and should be treated without delay.
Myopathy vs rhabdomyolysis
Stop statin if CK conc is 10x ULN or persistent unexplained muscle pain (even if CK is normal)
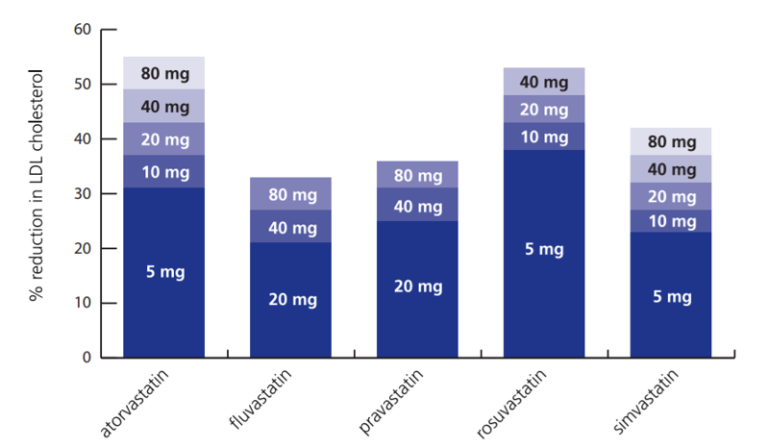
Comparative information – statins
LDL Lowering Effects
- Atorvastatin, Rosuvastatin and Simvastatin are more potent than Fluvastatin or Pravastatin.
- Administration but the strongest cholesterol (LDL-C) lowering effect are to be found with atorvastatin and rosuvastatin.
- Shorter acting statins (fluvastatin, pravastatin and simvastatin) should be taken in the evening (Maximises levels when liver is most active in producing cholesterol), however – this is not too important if taking dose in the evening effects compliance.
- Nighttime dose is not necessary with longer acting stations (atorvastatin or rosuvastatin). Mainly beneficial for very short acting statins such as simvastatin and fluvastatin.
Dosage
📺 Watch video: Mechanism of action of statins. (11:21 min)
Fibrates
 |
 |
 |
The two fibrates are fenofibrate and gemfibrozil. The action of fibrates are not totally understood. The fibrates act by four main mechanisms:
- Reduce the availability of substrate for triglyceride synthesis in the liver;
- promotion of the action of lipoprotein lipase which degrades circulating lipoproteins in the blood therefore reducing the circulating levels of circulating triglycerides
- modulation of low-density lipoprotein (LDL) receptor/ligand interaction and
- stimulation of reverse cholesterol transport which is the main pathway for the return of excess cholesterol from peripheral tissues to the liver for excretion in bile.
The overall effect is to reduce circulating cholesterol but this class of cholesterol lowering medicines is not as effective as the statins.
Use
Fibrates, used primarily to manage lipid disorders, require careful consideration in specific patient populations. They are contraindicated in individuals with severe renal or hepatic impairment and during pregnancy. Additionally, caution is advised when fibrates are used in conjunction with statins due to the increased risk of myopathy and related complications.
Side effects and precautions
Generally well tolerated, fibrates can cause some changes in liver function tests (LFTs), though there is little evidence to suggest progression to severe liver conditions such as liver failure or hepatitis.
Common adverse effects, occurring in more than 1% of patients, include gastrointestinal disturbances and a reversible increase in serum creatinine levels.
Less frequently, affecting 0.1-1% of patients, fibrates may lead to gallstones, pancreatitis, and photosensitivity.
Rarely, occurring in fewer than 0.1% of cases, adverse effects can include cholestatic jaundice, anemia, leucopenia, myopathy, rhabdomyolysis, and allergic reactions such as angioedema.
In practice, it is recommended to monitor aminotransferase levels every three months during the first year of fenofibrate therapy, discontinuing the drug if levels exceed three times the upper limit of normal (ULN).
📺 Watch video: Fibrate pharmacology. (2:21 min)
Ezetimibe
 |
 |
 |
The brush border enzyme inhibitor, ezetimibe works by blocking the intestinal absorption of cholesterol. It achieves this by selectively inhibiting transport mechanisms within the brush-border surface of the intestinal epithelial cells, specifically targeting the Niemann-Pick C1-Like 1 (NPC1L1) protein. See action in part c of figure below.
 As a result, when cholesterol absorption is reduced, the liver compensates by increasing the uptake of cholesterol from the circulation, thereby lowering serum cholesterol levels. When used as monotherapy, ezetimibe primarily reduces LDL cholesterol levels by up to 15-25%, with minimal impact on HDL and triglyceride levels. However, when combined with a statin, ezetimibe can produce an additional 20% reduction in serum LDL concentrations, along with a reduction in triglyceride levels and a slight increase in HDL levels.
As a result, when cholesterol absorption is reduced, the liver compensates by increasing the uptake of cholesterol from the circulation, thereby lowering serum cholesterol levels. When used as monotherapy, ezetimibe primarily reduces LDL cholesterol levels by up to 15-25%, with minimal impact on HDL and triglyceride levels. However, when combined with a statin, ezetimibe can produce an additional 20% reduction in serum LDL concentrations, along with a reduction in triglyceride levels and a slight increase in HDL levels.
Currently, ezetimibe is used in two main scenarios. First, it is used in combination with a statin in patients who have not reached their therapeutic goals with statin monotherapy. Second, it is used as monotherapy in patients who are intolerant of statin therapy.
Precautions
- Concurrent treatment with Fenofibrate
- Increased risk of gallbladder disease
- Hepatic impairment
- Manufacturer discourages usage in moderate/severe impairment
- Elderly
- Monitor carefully – some reports of depression in the elderly
- Pregnancy/Breastfeeding/Children – Currently no human data
Adverse effects
- Headache, diarrhoea
- Myalgia, Raised ALT/AST>3xULN
- Allergic reactions such as angioedema etc, pancreatitis, myopathy.
📺 Watch video: Ezetimibe pharmacology. (23.28 min)
PCSK9 Inhibitors
 |
 |
 |
Alirocumab (‘ali-roc-u-mab’) and Evolocumab (‘evo-loc-u-mab’)
Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors are a class of drugs that reduce circulating cholesterol levels, particularly low-density lipoprotein cholesterol (LDL-C). PCSK9 is a protein that binds to LDL receptors (LDLR) on the surface of liver cells. Normally, LDL receptors capture LDL-C particles from the bloodstream and internalize them into liver cells, where they are degraded and removed from circulation. However, when PCSK9 binds to LDL receptors, it leads to their degradation, reducing the number of receptors available to clear LDL-C from the blood.
PCSK9 inhibitors, such as monoclonal antibodies, work by binding to PCSK9 and preventing it from attaching to LDL receptors. This inhibition spares the LDL receptors from degradation, allowing them to recycle back to the liver cell surface. With more LDL receptors available, the liver can remove more LDL-C from the bloodstream, thereby significantly lowering the levels of circulating LDL-C. This mechanism is particularly beneficial for patients who have not achieved target LDL-C levels with statins alone or who are intolerant to statins.
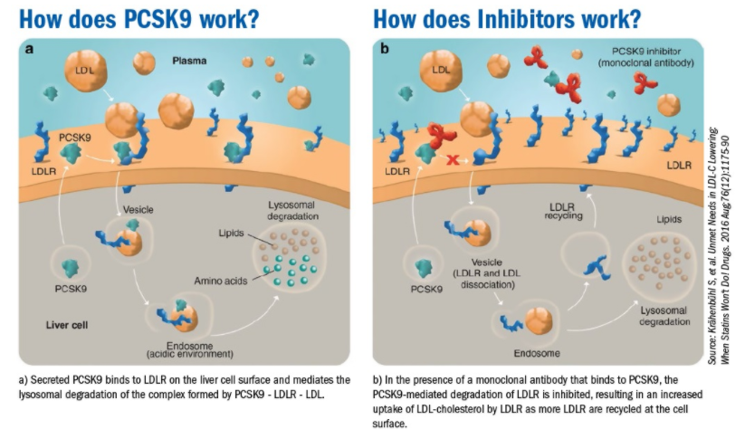 The PSCK9 inhibitors are monoclonal antibody-type drugs, therefore adverse effects include injection site reactions, rashes, nasopharyngitis, infections (e.g. ‘flu, URTIs, gastroenteritis), hypersensitivity reactions.
The PSCK9 inhibitors are monoclonal antibody-type drugs, therefore adverse effects include injection site reactions, rashes, nasopharyngitis, infections (e.g. ‘flu, URTIs, gastroenteritis), hypersensitivity reactions.
Small Interfering RNA (siRNA) Drugs
 |
 |
 |
Inclisiran (‘in-clis-eran’)
Inclisiran is a small interfering RNA (siRNA) drug designed to reduce the expression of the proprotein convertase subtilisin/kexin type 9 (PCSK9) gene. It targets and binds to the messenger RNA (mRNA) encoding PCSK9, preventing its translation into the PCSK9 protein.
Once inclisiran enters liver cells, it incorporates into the RNA-induced silencing complex (RISC). The RISC-inclisiran complex binds to the PCSK9 mRNA, leading to its cleavage and degradation. This reduces the production of the PCSK9 protein.
With lower PCSK9 levels, the degradation of low-density lipoprotein receptors (LDLRs) on liver cells decreases. Normally, PCSK9 binds to LDL receptors and promotes their degradation, reducing the liver’s ability to remove LDL-C from the blood.
The reduction in PCSK9 levels results in more LDL receptors being available on the surface of liver cells. These receptors bind and remove more LDL-C from the bloodstream, leading to a significant reduction in circulating LDL-C levels.
By this mechanism, inclisiran effectively lowers LDL-C levels, offering a promising therapeutic option for patients with hypercholesterolemia and those at high risk of cardiovascular diseases.
📺 Watch video: PSCK9 inhibitor and inclisiran pharmacology. (2:09 min)
Comparison of LDL-C Lowering Potential of Lipid-lowering Medicines
 |
 |
 |
Of the 3 classes of lipid lowering drugs – statins, ezetimibe and PSCK9 inhibitors, the PSCK9 inhibitors are the most potent at reducing circulating LDL-C levels. They can reduce circulating LDL-C levels by between 30-60%.
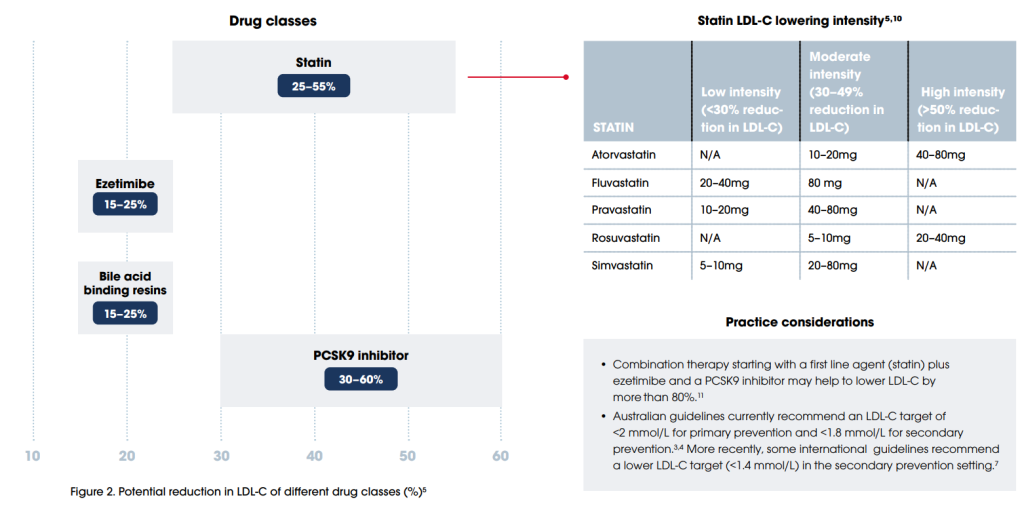 Next most potent class of cholesterol lowering thearpy are the statin class which can achieve a LDL-C lowering effect of between 25-55%. It is noteworthy that atorvastain and rosuvastatin, the two most potent statins have the greatest effect on lowering LDL-C.
Next most potent class of cholesterol lowering thearpy are the statin class which can achieve a LDL-C lowering effect of between 25-55%. It is noteworthy that atorvastain and rosuvastatin, the two most potent statins have the greatest effect on lowering LDL-C.
Last is ezetimibe which can achieve a 15-25% reduction in circulating LDL-C levels.
If the patient has triglyceridemia, probably the most effective drug treatment are the fibrates. Fibrates can reduce triglycerides by 40-80% with a LDL reduction benefit of 5-15%.
Cost
It is worth understanding the cost of lipid-lowering therapies to the patient or the PBS. The following information provides a comparison of the cost to treat eleveated cholesterol for the first 6 months of treatment for hypercholesterolemia.
Download the lecture notes here:
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.