1.2 Prevalence and Prevention of Cardiovascular Disease
Prevalence of Cardiovascular Disease
 |
 |
 |
Learning Outcomes
Be able to:
- Describe the prevalence of CV disease in Australia
- Predict the influence of SES, age, gender, remoteness and ethnicity on population rates of CV disease
- Identify the major modifiable risk factors for CV disease
- Assess primary cardiovascular risk for an individual using standardized assessment tools
- Provide advice to patients on the reduction of modifiable risk factors.
Cardiovascular disease (CVD) is an umbrella term used to encompass several different diseases that impact the cardiovascular system. Atherosclerotic coronary artery disease (or coronary heart disease) is the leading cause of death in Australia. In 2021 it was responsible for 1 in 10 deaths while stroke accounted for another 5% of all deaths. These figures highlight the significant burden of CVD in Australia. Currently, approximately 4.15 million Australians have some sort of cardiovascular disease, the most common being coronary heart disease (the leading cause of death in Australia), heart attack and heart failure.
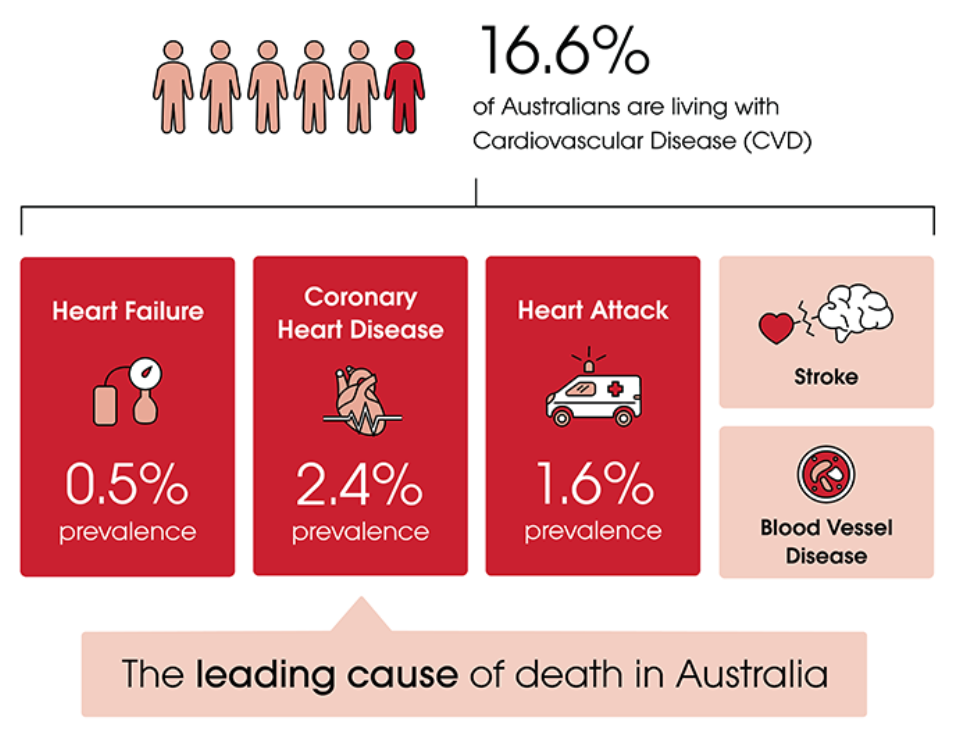 Image from: https://www.heartfoundation.org.au/
Image from: https://www.heartfoundation.org.au/
Cardiovascular disease is very common. However, the incidence of cardiovascular disease changes by patient profile and location. In general,
- The Northern Territory and Queensland have higher rates of hospital admissions for heart disease compared with the national average.
- Aboriginal and Torres Strait Islander people have much higher rate of hospital admissions for heart disease compared with non-Indigenous Australians.
- Males are more likely to be affected by heart disease compared to females.
- The rates of hospital admissions for heart related diseases increases with age.
- The rates of heart disease are much higher the more remote the location and the more socioeconomic disadvantage a person faces
This is very useful information to assess the population risk for cardiovascular disease in your community and develop pharmacist led interventions that can help address the risks of your community. A very helpful source of information is the Interactive Australian Health Maps which allow you to compare heart health indicators across Australia. The data for this website comes from the Australian Institute for Health and Wellbeing and the Australian Bureau of Statistics.
📺Watch the vodcast discussing the prevalence of cardiovascular disease in Australia. (8.34 minutes)
📚 Read/Explore
- Revision activity: Go to the Heart Foundation Interactive Australian Heart Map and answer the following:
- Which state/territory has the best CV health outcomes?
- Which state/territory has the worst CV health outcomes?
- How do Cairns, Townsville and Mackay compare to each other and the state average?
- What are some factors that might explain the difference in CV outcomes between Cairns, Townsville and Mackay?
- Read the 2023 Australian Guideline for assessing and managing cardiovascular disease risk
While cardiovascular disease has a high prevalence in Australian society, the risk can be reduced at a patient and population level by addressing multiple risk factors. Many people are not aware of the risk factors associated with cardiovascular disease and may not pay particular attention to them. Cardiovascular risks can be divided into modifiable and non-modifiable risks. The table below outlines some modifiable and non-modifiable risk factors for developing cardiovascular disease.
| Non-Modifiable Risk Factors | Modifiable Risk Factors |
| Age (increased age = increased risk) | Obesity/overweight |
| Gender (male higher risk than female) | Smoking status |
| Ethnicity (ATSI higher risk compared with non-Indigenous) | Blood pressure |
| Family history | Elevated lipid (cholesterol) profile |
| Diabetes |
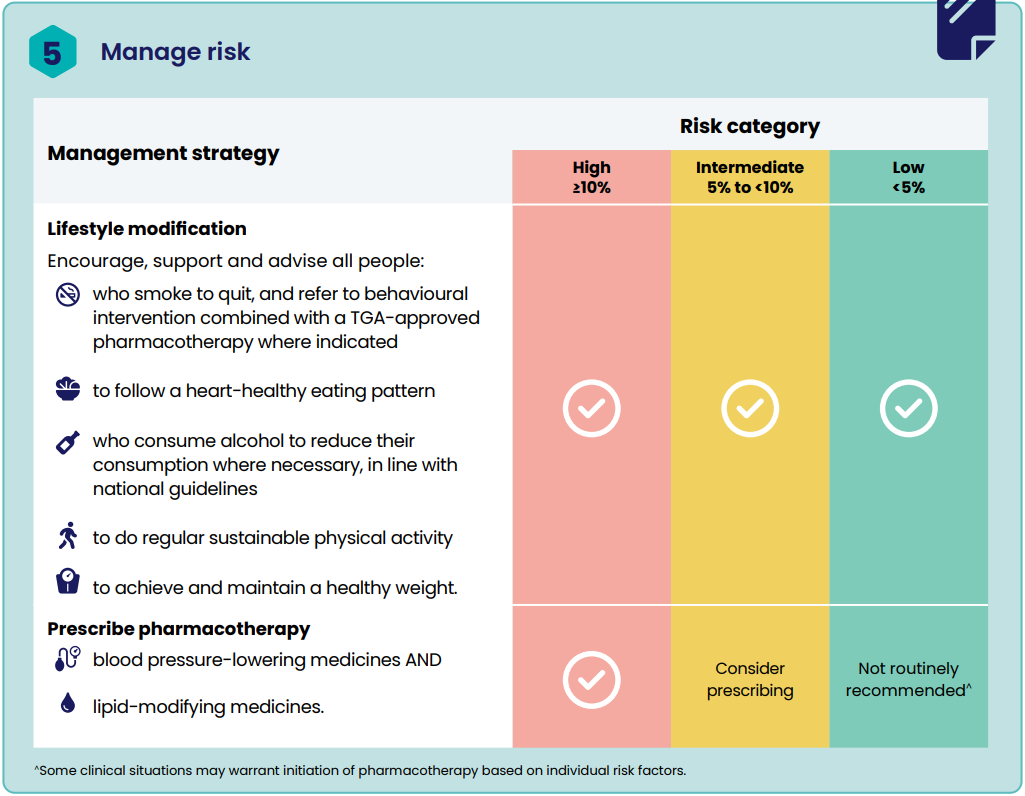
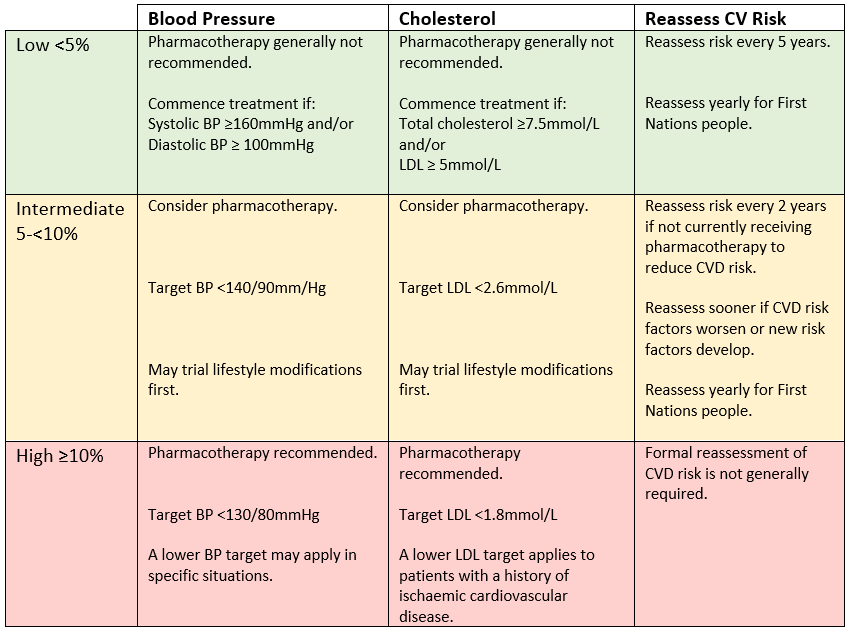
A comprehensive approach to reduction in modifiable risks can have a significant overall reduction of risk of developing cardiovascular disease in the next 5 year period. Research confirms when a comprehensive absolute cardiovascular risk reduction strategy is pursued, that is superior to an approach that reduces a single risk factor. That is, if a patient has multiple risks (for example is obese, smokes, has high blood pressure and hypercholesterolemia), the greatest risk reduction is realized when all 4 risks are targeted.
Who should have their CV risk calculated?
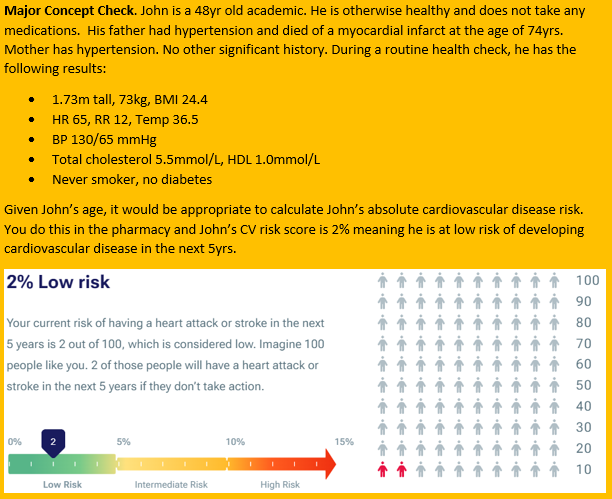
Adults without established cardiovascular disease and who are 45 years or older (or 30 years or older if Aboriginal and Torres Strait Islander) should have their CV risk calculated. Interventions and lifestyle advice to reduce the risk in these people is known as “primary prevention”.
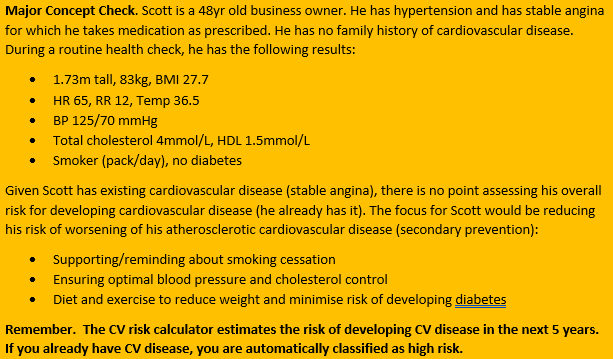
Patients with established cardiovascular disease (eg a prior heart attack or stroke) do not need their risk calculated as they are automatically at high risk. These people still benefit from an absolute risk reduction strategy however it will be “secondary prevention” and likely to be more aggressive in terms of treatment and monitoring than primary prevention.
Patients with moderate to severe kidney disease (eGFR<45ml/min and/or macroalbuminurea) or familial hypercholesterolaemia are also automatically considered high risk. Again, these patients benefit from absolute cardiovascular risk reduction strategies, you just don’t need to use the calculator to calculate their risk because you know they are high risk.
How do we calculate CV risk?
The AusCVDRisk was developed by the Australian Heart Foundation and other professional organisations and was released in 2023. The calculations are based on the NZ PREDICT-1 equation, which was formulated from a large, New Zealand patient cohort from 2002-2015. Some adjustments were made to account for differences in Australian rates of CVD and other differences between the Australian and New Zealand population. It is what we use to estimate patients’ risk of suffering a cardiovascular event in the next 5 years. Variables such as age, diabetes history, cholesterol, systolic BP, sex, smoking status and current cardiovascular medications are taken into account. For people with diabetes, information such as microalbuminurea, renal function, BMI, HbA1c, insulin use, time since diagnosis can also be included to better estimate the risk. The AusCVDRisk expresses the patients’ risk of suffering a cardiovascular event in the next 5 years as a percentage and stratifies the risk into 3 categories. The categories are low, intermediate and high risk. This calculation guides treatment and monitoring recommendations.
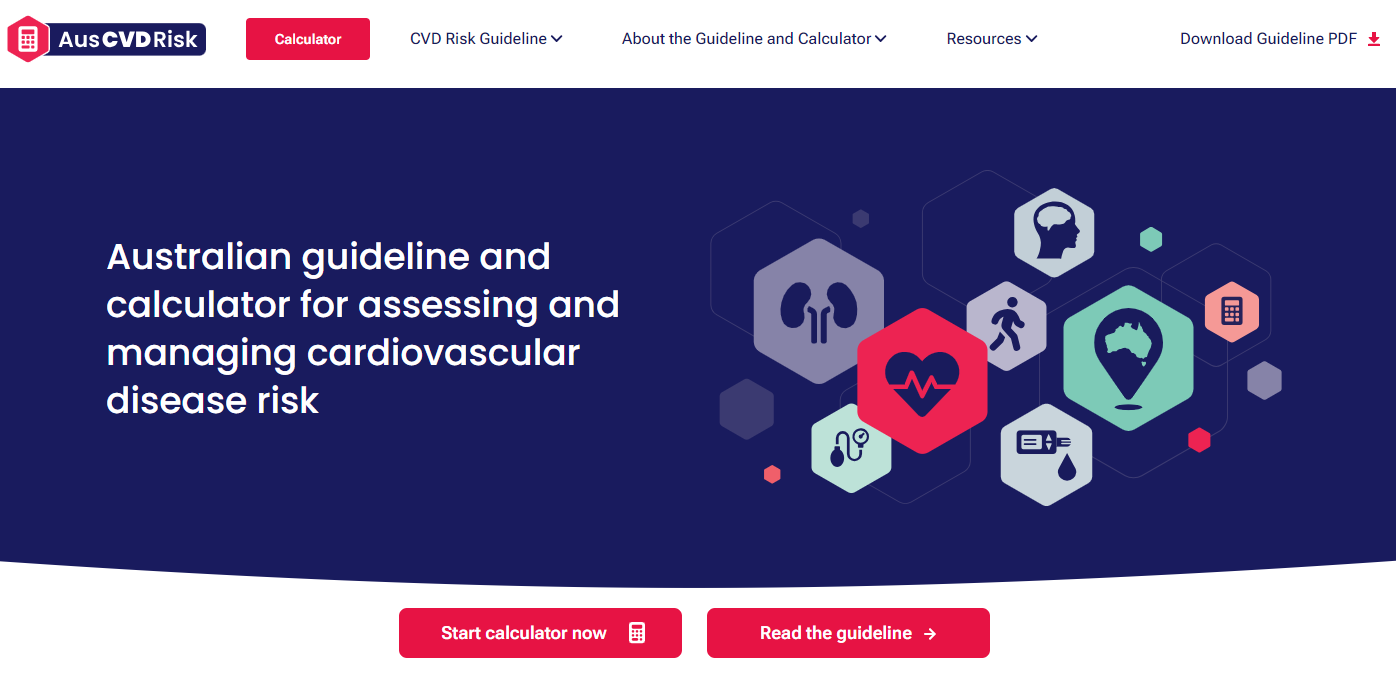 The AusCVDRisk online tool allows for individualisation/reclassification of risk following the initial calculation. It allows the result to be adjusted, based on:
The AusCVDRisk online tool allows for individualisation/reclassification of risk following the initial calculation. It allows the result to be adjusted, based on:
- Ethnicity (increase or decrease)
- Family history of premature CVD (increase)
- Chronic kidney disease (increase)
- Severe mental illness (increase)
- Coronary artery calcium score (increase or decrease)
These factors are of particular importance for patients who receive a borderline % risk score and may influence a decision to commence (or not) pharmacotherapy. For example, a patient with intermediate risk and family history of premature CVD is more likely to receive pharmacotherapy than a patient with intermediate risk and a coronary artery calcium score of 0.