2.1.1 What is Hypertension?
What is Hypertension?
 |
 |
 |
Hypertension is the term for high blood pressure over a long period of time. The current guidelines define hypertension as a sustained blood pressure that is greater than or equal to a systolic pressure of 140mmHg and/or a diastolic pressure of 90mmHg, though the definition of hypertension is arbitrary. This is because we know that there is a continuous relationship between increasing blood pressure and the incidence of complications associated with high blood pressure.
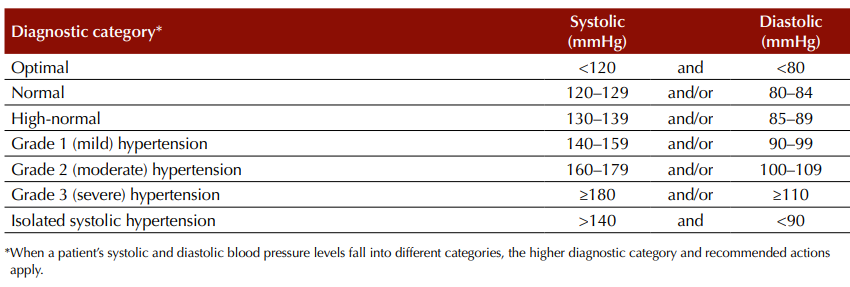
The Heart Foundation Guideline for the diagnosis and management of hypertension in adults 2016 classifies blood pressure into 7 categories:
Consequences of persistent elevated blood pressure
The pathophysiology and perpetuation of the hypertensive state involves structural changes, remodelling, and development of atherosclerosis in arterioles. Endothelial injury hastens the progression of atherosclerotic plaque development, leading to some of the known complications of untreated hypertension that include:
- Coronary artery disease
- Stroke
- Peripheral artery disease.
Non-ischaemic complications of hypertension are often attributable to increased myocardial workload or damage to the fragile microcirculation of the kidneys and eyes. Such complications include:
- Heart failure
- Arrhythmias
- Chronic kidney disease
- Retinopathy
Hence, blood pressure cut-offs for treatment of hypertension may be lower than 140/90mmHg for people with comorbidities that increase their risk of complications associated with hypertension, and/or for people with a high absolute CV risk.
Before deciding on an appropriate course of treatment, BP measurements the clinician must read at least 2 measurements taken ≥ 1 week apart. This information can then be used as part of the absolute CVD risk assessment.
Hypertension and CV Risk
 |
 |
 |
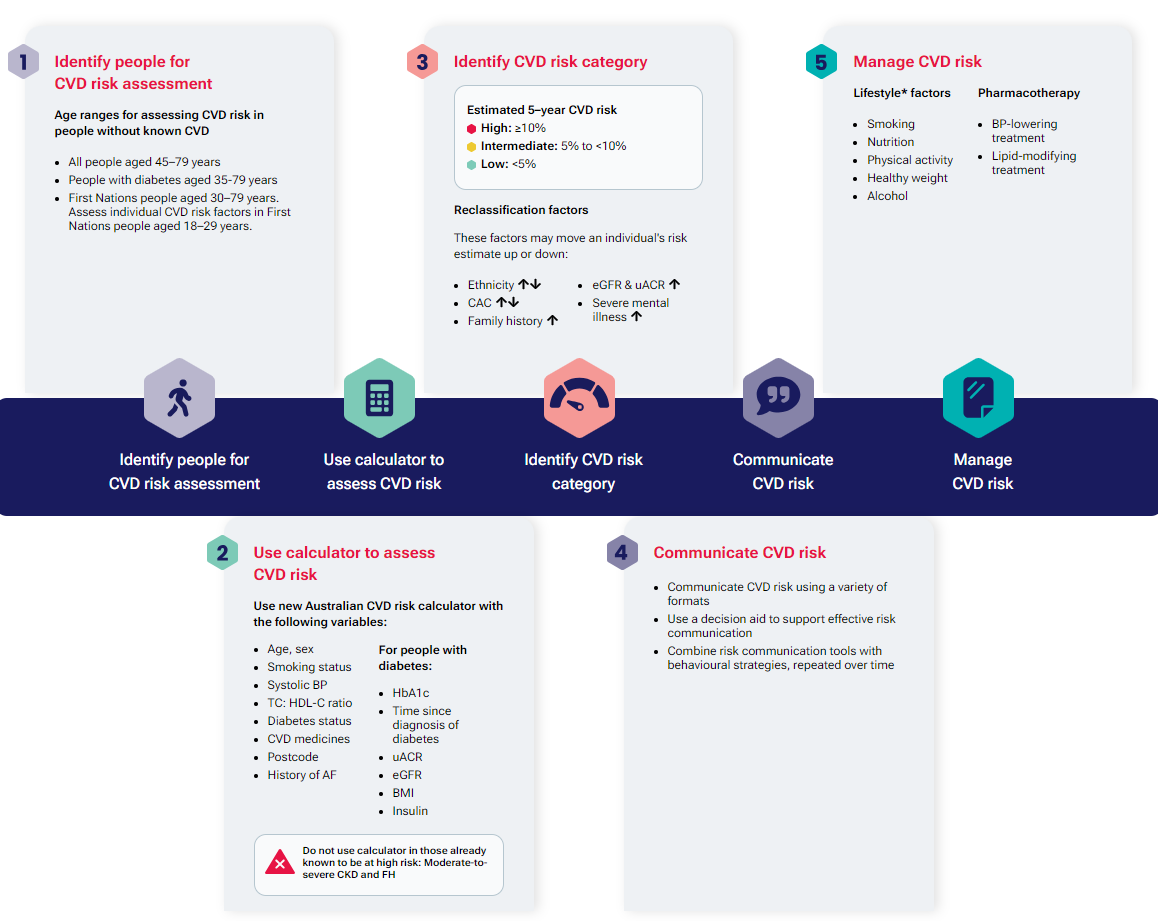
Patients should have their cardiovascular risk calculated to identify appropriate treatment. The Australian guideline and calculator for assessing and managing cardiovascular disease risk identifies 5 steps in the process:
Remember CV risk assessment may be inappropriate if:
- There is known CVD (= automatically high risk)
- The patient is ineligible for CV risk assessment using the calculators because they are too young (the calculator has not been validated for patients aged less than 30 years (if Aboriginal or Torres Strait Islander) or other patients aged less than 45 years)
Furthermore, oral antihypertensive therapy may be initiated upon presentation if the patient has:
- Elevated BP ≥ 180/110mmHg and symptoms (headache) or evidence of target organ damage.
Next, let’s look at the epidemiology of high blood pressure in Australia.
Rates of Hypertension in Australia
 |
 |
 |
The incidence of high blood pressure in Australia is high. The self-reported rates of high blood pressure (those in the population who have been told they have elevated blood pressure), is much lower than the measured rate of high measured blood pressure (meaning there are many people with undiagnosed hypertension). Over one in ten (11.6% or 3.0 million) Australian adults reported having hypertension in 2022. This represented a 13.7% increase on the previous reporting period 2011–12. (note, this could be because screening has improved or disease rates have worsened or both).
When blood pressure was actually measured, one in five Australians had a high measured blood pressure. Approximately 23.3% of adults had high measured blood pressure and the rate of high measured blood pressure has increased by around 8.3% since the last ABS reporting period (2011-12).
From the figure above, one can see:
- The rates of high blood pressure in Australia is itself…. High.
- The rate of high measured blood pressure in the population increases with age.
- Males have a marginally higher rate of elevated measured blood pressure (though the rates are fairly comparable).
- All age groups are represented in the distribution of high blood pressure in Australia – yes even amongst the young pharmacy and medical students sitting around you.
The high prevalence of hypertension in Australia underscores the importance of public health initiatives focused on promoting healthier lifestyles, regular physical activity, balanced diets, and smoking cessation to reduce the burden of this condition. The rates of undiagnosed high blood pressure underscore the importance and value of regular opportunistic screening undertaken by doctors, nurses and pharmacists as part of primary care disease reduction strategies.
Hypertension in Indigenous vs. Non-Indigenous Australians
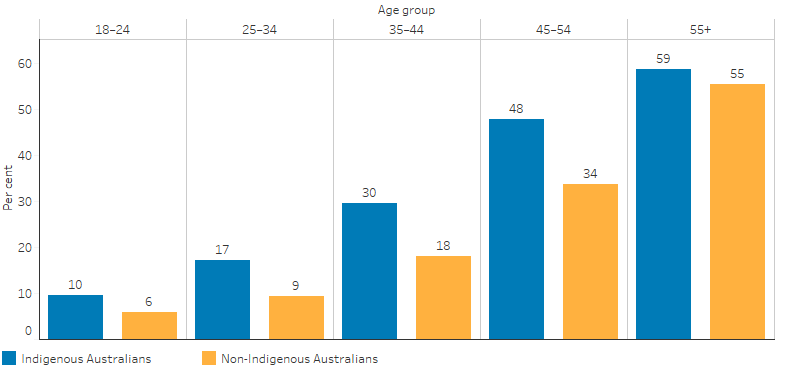
Hypertension, or high blood pressure, is a prevalent health issue in Australia, with notable differences in prevalence between Indigenous and non-Indigenous populations. According to the AIHW Aboriginal and Torres Strait Islander Health Performance Framework (2018–19), an estimated 31% (151,000) of Aboriginal and Torres Strait Islander adults had high blood pressure based on both measured and reported data. This rate is significantly higher compared to non-Indigenous Australians across all age groups.

Indigenous males were more likely to have high measured blood pressure (25%) compared to Indigenous females (21%). Additionally, a higher percentage of Indigenous males (76%) had high measured blood pressure that they did not report, compared to Indigenous females (74%). This underreporting indicates a potential gap in awareness and diagnosis of hypertension within the Indigenous male population.
The rate of high blood pressure among Indigenous adults was similar in both remote (32%) and non-remote areas (31%), suggesting that location does not significantly influence the prevalence of hypertension in these communities. This uniformity across different settings highlights systemic issues that transcend geographic boundaries, such as access to healthcare and socioeconomic factors.
When comparing the prevalence of hypertension between Indigenous and non-Indigenous Australians, Indigenous Australians consistently showed higher rates of high blood pressure across all age groups. The most significant disparity was observed in the 45–54 age group, where the difference was 14 percentage points. This substantial gap underscores the need for targeted interventions to address the unique health challenges faced by Indigenous communities.
Indigenous Australians are more likely to experience high blood pressure, with particular disparities among males and in specific age groups. Addressing these differences requires comprehensive public health strategies that focus on improving healthcare access, increasing awareness, and promoting healthier lifestyles within Indigenous communities.
The data highlights that a significant number of adults in both Indigenous and non-Indigenous Australian populations have undiagnosed high blood pressure. The prevalence of measured high blood pressure among Indigenous adults is approximately 1.2 times higher than that of non-Indigenous adults. Indigenous Australians have over double the hospitalisation rate for hypertension compared to non-Indigenous Australians, even though high blood pressure accounts for a similar percentage of GP consultations in both groups. This suggests a gap in primary health care for Indigenous Australians, where early detection and management of high blood pressure could reduce hospitalisations for more severe conditions.
Among Indigenous Australians aged 45–54 years, the disparity in high blood pressure prevalence and hypertension-related hospitalisations compared to non-Indigenous Australians of the same age is the most pronounced. Early, targeted assessment, education, and advice on cardiovascular risk factors for Indigenous Australians, starting in adolescence, are essential.
Effective diagnosis and management of high blood pressure among Indigenous Australians require access to primary health care with systems that identify Indigenous clients, enabling the use of Indigenous-specific Medicare items for health assessments and chronic disease management.
What causes hypertension?
 |
 |
 |
Hypertension is a significant health issue in Australia, affecting a substantial portion of the population. The causes of hypertension are multifactorial and include genetic, lifestyle, and environmental factors. Hypertension is treatable with relevant pharmacology and lifestyle changes.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.