3.2 Business and Management – Conflict Management and Negotiation
Conflict Management and Resolution in Healthcare and Pharmacy Practice
This section builds on the Introduction to Management in Year 1 and includes three important areas of management for pharmacy practice – conflict management, managing teams and managing complex and culturally diverse workplaces.
Learning Outcomes
- Describe some of the causes of conflict initiation and maintenance in the context of pharmacy practice
- Develop an approach for resolving a conflict scenario
- Describe the broad skills that you think a pharmacist should possess in order to manage conflict
- Explain the different types of conflict that the pharmacist might encounter in pharmacy practice
- List 5 strategies that the pharmacist might use to resolve conflict.
Conflict is inevitable in healthcare settings due to the complex interactions among healthcare professionals, patients, and their families. In pharmacy practice, the stakes are particularly high, as conflicts can impact patient safety, the quality of care, and the professional relationships that sustain effective healthcare delivery. Conflict management and resolution are essential skills that pharmacists must develop to ensure optimal healthcare outcomes and a positive work environment.
Conflict arises when individuals perceive a threat to their needs, values, or goals. In pharmacy practice, conflicts may stem from disagreements over treatment plans, medication errors, communication breakdowns, or ethical dilemmas. Pharmacists are frequently involved in collaborative care teams and work closely with other healthcare professionals, such as doctors, nurses, and allied health workers. Interprofessional collaboration requires clear communication and alignment of goals, and when these are lacking, conflict can arise.1
Effective conflict management in healthcare is vital for promoting patient-centered care. Mismanaged conflicts can lead to workplace stress, burnout, and a breakdown in teamwork, all of which can negatively affect patient safety and outcomes. Research suggests that unresolved conflict may contribute to medication errors and reduced quality of care, as it disrupts the coordination necessary for safe and effective treatment.2 Therefore, pharmacists must be adept at recognizing, addressing, and resolving conflicts in their day-to-day practice.
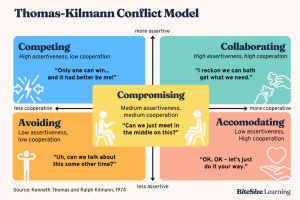
One widely used approach to conflict resolution is the Thomas-Kilmann Conflict Mode Instrument (TKI), which identifies five styles of managing conflict: competing, accommodating, avoiding, compromising, and collaborating.3 In the healthcare setting, the collaborative approach is generally preferred, as it encourages open dialogue, mutual respect, and the shared goal of improving patient care. Collaboration involves acknowledging differing viewpoints and working together to find a solution that satisfies all parties. This approach is especially important in pharmacy, where decisions about medication therapies often require input from multiple healthcare providers.
Pharmacists are also increasingly responsible for patient consultations, particularly in community pharmacy settings. Conflicts may arise during interactions with patients who have concerns about their medications or who are non-compliant with treatment regimens. In such cases, pharmacists must utilize strong communication skills, empathy, and active listening to address patient concerns, educate them about their treatment options, and work towards a resolution that ensures adherence to therapy. Clear communication and building trust are crucial in resolving these conflicts, as they help bridge the gap between the patient’s expectations and the pharmacist’s recommendations.
Another key strategy in conflict resolution is the development of emotional intelligence (EI) among pharmacists. Emotional intelligence, defined as the ability to recognise, understand, and manage one’s own emotions and the emotions of others, plays a critical role in navigating conflicts in healthcare. Pharmacists with high EI are better equipped to manage their emotional responses in stressful situations, engage in compassionate communication, and find solutions that foster cooperation rather than escalation.4
Conflict management and resolution are integral to maintaining effective pharmacy practice and safeguarding patient care. Pharmacists must be proactive in developing conflict resolution skills, fostering collaboration, and enhancing their emotional intelligence. By doing so, they can mitigate the adverse effects of conflict, improve interprofessional relationships, and ensure that patient-centred care remains at the forefront of their practice.
🎧 Listen to the recorded lectures
Working in Teams
Learning Outcomes
Be able to:
- Describe the process of getting the basics right for engagement to build the team in the pharmacy practice context. “One of the key areas for the success of a well‐functioning team is ‘staff engagement’”.
- Describe how you would go about building the team in your practice, highlighting the value of the team.
As pharmacists, we continually engage with multiple different people to ensure the most successful outcome for our patients. This could be as simple as interacting with people within the pharmacy department we work in, but it can also include the patient’s broader healthcare team. Working in teams is important for several reasons, both in professional and personal contexts:
These elements of positive teamwork are crucial across various fields.
The role of the pharmacist manager is to enrich our teams, and build and support them so that our teams can bring out the best in each other and operate as a single unit effectively.
Managing Complex and Culturally Diverse Workplaces:
This lecture is to follow on from the working in teams lecture. This explains managing a team that is complex and culturally diverse.
🌡️Self check quiz
👁️ Watch the following video: Negotiation Skills Top 10 Tips
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.
