4.2.2 Acute Kidney Injury
Learning Outcomes
Be able to:
- Define ‘acute kidney injury’ and how this differs from ‘acute renal failure’ and ‘chronic kidney disease’
- Explain the 3 different types of acute kidney injury (pre-renal, intrinsic, and post-renal), including the common causes of each
- Describe the approach to management of acute kidney injury.
Acute Kidney Injury
Acute kidney injury is an acute or abrupt decline in kidney function, that generally manifests as a fall in urine output and/or as a rise in serum creatinine levels. Generally, reduced urine output occurs before serum creatinine levels rise, because we know that creatinine levels increase slower than GFR decreases. That is, normal serum creatinine does not always represent normal renal function.
An acute kidney injury may present anywhere along a spectrum that extends only from mild kidney impairment, all the way to severe kidney failure (i.e., the AKI may be mild, moderate, or severe). Acute kidney injuries are most commonly asymptomatic. However, they may present with signs and symptoms including:
- Pulmonary or peripheral oedema
- Fatigue
- Confusion
- Nausea
- Seizures or coma
Acute kidney injuries are especially common among patients who are already hospitalised for another reason. Patients in an intensive care unit (ICU) are at particularly high risk, because these patients are critically unwell, and because they are being treated with a multitude of different medications that may be nephrotoxic.
There are a variety of possible risk factors and a variety of possible causes of an acute kidney injury. Less-modifiable risk factors include a history of chronic disease (e.g., chronic kidney disease, diabetes, heart disease, lung disease, liver disease), advancing age, and female gender. Potentially avoidable kidney insults include hypovolaemia and certain medications.
There are 3 main types of acute kidney injury:
- Pre-renal
- Intrarenal (also known as intrinsic), and
- Post-renal
The different causes of acute kidney injury are commonly grouped into 1 of these 3 types of acute kidney injury.
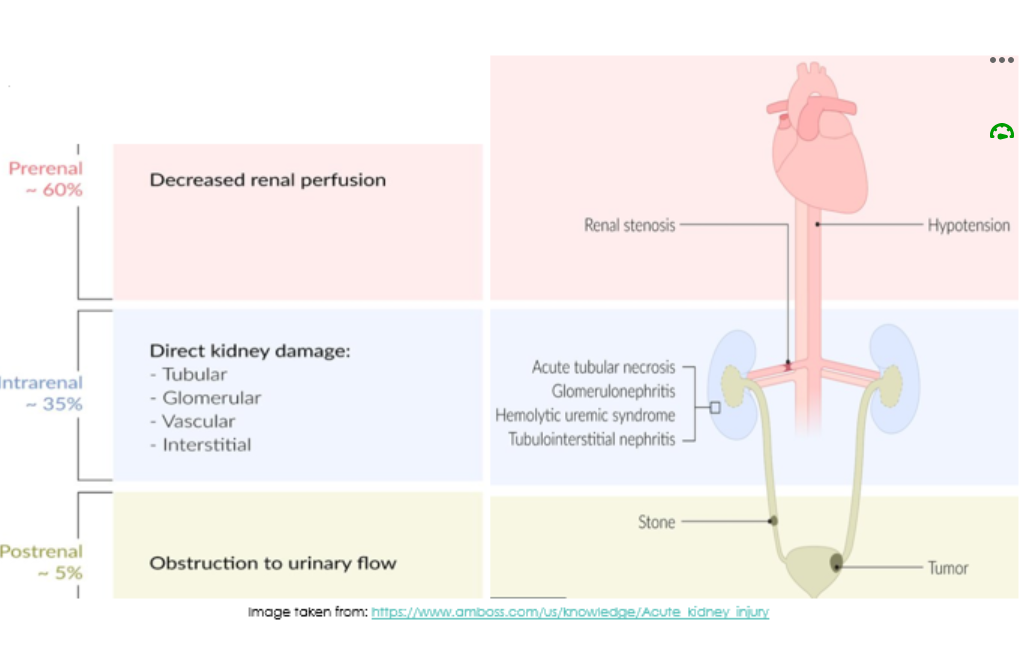 1. Pre-renal
1. Pre-renal
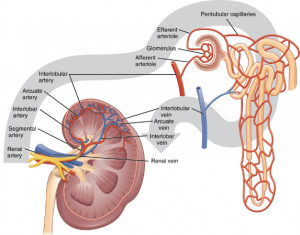
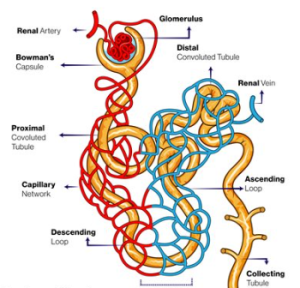
Pre-renal causes of acute kidney injury include factors affecting glomerular perfusion. That is, factors affecting the afferent and efferent renal arterioles, and factors affecting circulating blood volume.
2. Intra-renal (Intrinsic)
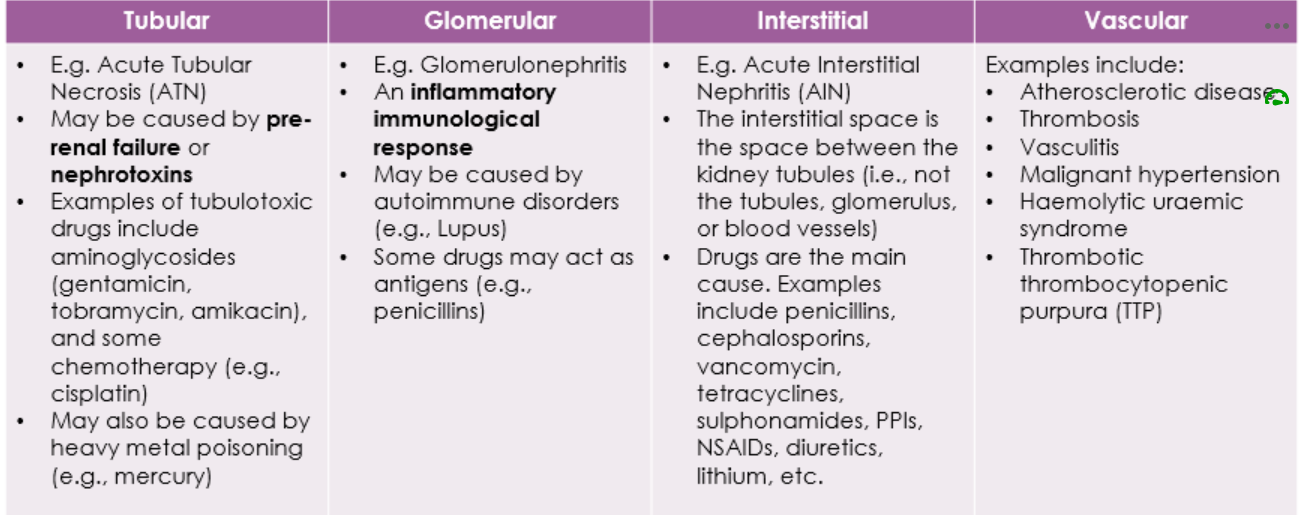
This type of acute kidney injury has 4 different subtypes, but may be multifactorial. See the image below.
Post-renal causes of acute kidney injury include factors that mechanically obstruct urinary outflow. Examples include prostate hyperplasia, urinary retention, and congenital malformations of the urinary tract.
Treatment
It is important that an acute kidney injury is treated quickly and correctly, because AKI is associated with poor patient outcomes, including increased morbidity and mortality rates. With appropriate management there may be complete recovery of renal function. However, for some people, the acute kidney injury progresses to chronic kidney disease that may or may not necessitate dialysis.
Immediate treatment is supportive. It involves:
- Identifying and correcting the underlying cause of the AKI
- Identifying and avoiding nephrotoxic drugs. E.g., NSAIDs, aminoglycoside antibiotics, and iodinated contrast agents
- Withholding other drugs that may worsen renal function. E.g., ACEIs
- Adjusting the doses of renally cleared medications
- Close monitoring of renal function and electrolytes
📺 Watch this video on Acute Kidney Injury (25:45 minutes)
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.