10. Messages in the body

- Explain the role of cellular communication in monitoring and maintaining homeostasis
- Describe the structure and function of the nervous system
- Explain how a message is passed through the nervous system
- Describe the structure and function of the endocrine system
- Explain how a message is passed through the endocrine system
- Compare and contrast the actions of the endocrine and nervous systems in maintaining homeostasis.
10.1 | Cell communication
Cellular communication is an important process that allows cells to pass signals to one another.
Remember playing the game telephone as a kid? One person started with a message that got passed down the line through whispers. As the message made its way from person to person, it changed into something different and by the end may have had nothing to do with the original statement. This happens because there is a communication problem along the line. It shows you just how important good communication is, even with something as simple as a child’s game.
Your cells also rely on good communication, but unlike a game of telephone, if there is a miscommunication, the consequences can be quite severe!
Cell-to-cell signaling is a critical component of coordinating cellular activities. Through this communication, messages are carried from signaling cells to receiving cells, also known as target cells. This signaling occurs with proteins and other types of signaling molecules. What kinds of processes and activities depend on cell communication? Just about everything you can imagine that happens in your body depends on cell communication – growth and development, cellular reproduction, tissue repair, sensing pain, and much more.
How do cells communicate?
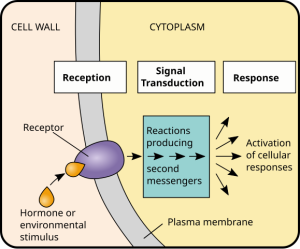
The pathway along which cellular communication occurs is called the signal transduction pathway. It is a series of cellular and molecular changes that help a target cell receive a message and respond accordingly. These pathways are crucial to cellular function because they are the main mode of communication between cells.
Here is how it works. First, a signaling cell secretes a signaling molecule, which then travels to the target cell. Once it reaches the target cell, it binds with a receptor protein in the target cell’s membrane. This is the first step of cell signaling, called reception.
This receptor protein is like the security guard at an entrance gate – it is the designated check-in point for the signaling molecule. When the receptor protein security guard accepts the signaling molecule and binds to it, a relay begins, which is the second step of cell signaling, called transduction. Just like a baton is passed from person to person in a relay race, so is the signal in the target cell through the process of transduction as it passes from relay molecule to relay molecule.
The final relay molecule activates a protein that triggers the final stage of cell signaling, called response. Each response is different because it depends on the message that was carried through the cell.
Communication can be viewed as a process in which a sender transmits signals to one or more receivers to control and coordinate actions. In the human body, two major organ systems participate in relatively long distance communication: the nervous system and the endocrine system. Together, these two systems are primarily responsible for maintaining homeostasis in the body.
10.2 | The nervous system
As you read this, your nervous system is performing several functions simultaneously. The visual system is processing what is seen on the page; the motor system controls your eye movements and the turn of the pages (or click of the mouse); the prefrontal cortex maintains attention. Even fundamental functions, like breathing and regulation of body temperature, are controlled by the nervous system. The nervous system acquires information from sensory organs, processes it and then may initiate a response either through motor function, leading to movement, or in a change in the organism’s physiological state. The nervous system is one of two systems that exert control over all the organ systems of the body; the other is the endocrine system. The nervous system’s control is much more specific and rapid than the hormonal system. It communicates signals through cells and the tiny gaps between them rather than through the circulatory system as in the endocrine system. It uses a combination of chemical and electrochemical signals to cover long distances quickly, rather than purely chemical signals used by the endocrine system.
What are the basic functions of the nervous system?
The nervous system is involved in receiving information about the environment around us (sensation) and generating responses to that information (motor responses). The nervous system can be divided into regions that are responsible for sensation (sensory functions) and for the response (motor functions). But there is a third function that needs to be included. Sensory input needs to be integrated with other sensations, as well as with memories, emotional state, or learning (cognition). Some regions of the nervous system are termed integration or association areas. The process of integration combines sensory perceptions and higher cognitive functions such as memories, learning, and emotion to produce a response.
Sensation: The first major function of the nervous system is sensation—receiving information about the environment to gain input about what is happening outside the body (or, sometimes, within the body). The sensory functions of the nervous system register the presence of a change from homeostasis or a particular event in the environment, known as a stimulus. The senses we think of most are the big five: taste, smell, touch, sight, and hearing. The stimuli for taste and smell are both chemical substances (molecules, compounds, ions, etc.), touch is physical or mechanical stimuli that interact with the skin, sight is light stimuli, and hearing is the perception of sound, which is a physical stimulus similar to some aspects of touch. There are actually more senses than just those, but that list represents the major senses. Those five are all senses that receive stimuli from the outside world, and of which there is conscious perception. Additional sensory stimuli might be from the internal environment (inside the body), such as the stretch of an organ wall or the concentration of certain ions in the blood.
Response: The nervous system produces a response on the basis of the stimuli perceived by sensory structures. An obvious response would be the movement of muscles, such as withdrawing a hand from a hot stove, but there are broader uses of the term. The nervous system can cause the contraction of all three types of muscle tissue. For example, skeletal muscle contracts to move the skeleton, cardiac muscle is influenced as heart rate increases during exercise, and smooth muscle contracts as the digestive system moves food along the digestive tract. Responses also include the neural control of glands in the body as well, such as the production and secretion of sweat by sweat glands found in the skin to lower body temperature.
Responses can be divided into those that are voluntary or conscious (contraction of skeletal muscle) and those that are involuntary (contraction of smooth muscles, regulation of cardiac muscle, and activation of glands). Voluntary responses are governed by the somatic nervous system and involuntary responses are governed by the autonomic nervous system, which are discussed in the next section.
Integration: Stimuli that are received by sensory structures are communicated to the nervous system where that information is processed. This is called integration. Stimuli are compared with, or integrated with, other stimuli, memories of previous stimuli, or the state of a person at a particular time. This leads to the specific response that will be generated. Seeing a baseball pitched to a batter will not automatically cause the batter to swing. The trajectory of the ball and its speed will need to be considered.
How is the nervous system organised?
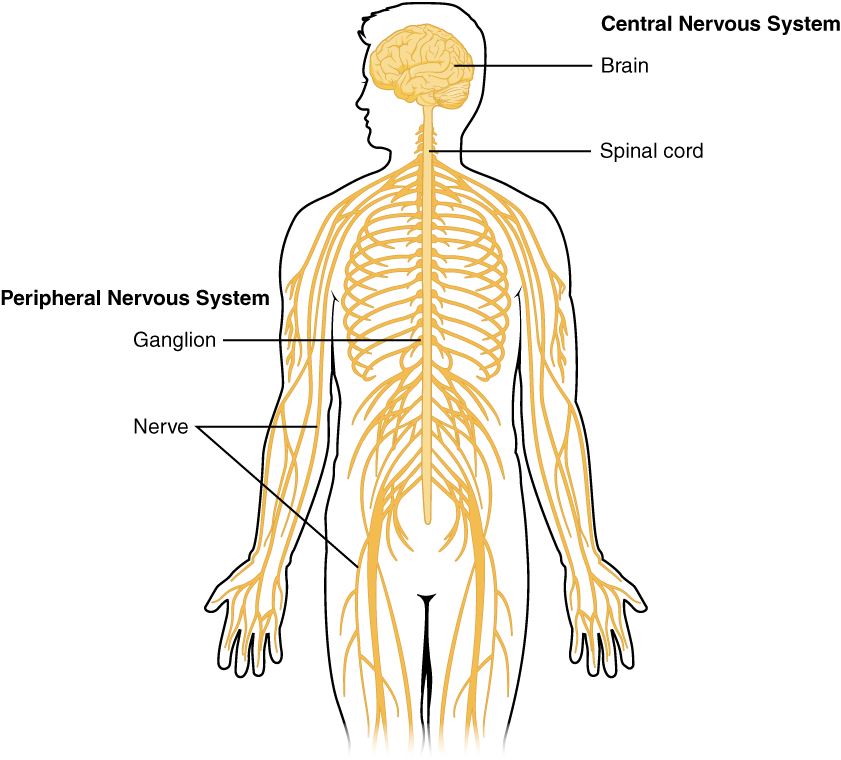
The nervous system can be divided into two major regions: the central and peripheral nervous systems. The central nervous system (CNS) comprises the brain and spinal cord, and the peripheral nervous system (PNS) is everything else (Figure 10.3). The brain is contained within the cranial cavity of the skull, and the spinal cord is contained within the vertebral cavity of the vertebral column. It is a bit of an oversimplification to say that the CNS is what is inside these two cavities and the peripheral nervous system is outside of them, but that is one way to start to think about it. In actuality, there are some elements of the peripheral nervous system that are within the cranial or vertebral cavities. The peripheral nervous system is so named because it is on the periphery—meaning beyond the brain and spinal cord. Depending on different aspects of the nervous system, the dividing line between central and peripheral is not necessarily universal.
Nervous tissue can also be described as grey matter and white matter on the basis of its appearance. These descriptions are more often used in the CNS. Grey matter is where neuronal cell bodies are found and white matter is where the axonal tracts are found. In the PNS, ganglia are basically grey matter and nerves are white matter. Note that a ganglion is a structure containing a number of nerve cell bodies, typically linked by synapses, and often forming a swelling on a nerve fibre.
The central nervous system
The central nervous system (CNS) is made up of the brain and spinal cord and is covered with three layers of protective coverings called meninges (meninges is derived from the Greek and means membranes). The outermost layer is the dura mater, the middle layer is the web-like arachnoid mater, and the inner layer is the pia mater, which directly contacts and covers the brain and spinal cord. The space between the arachnoid and pia maters is filled with cerebrospinal fluid (CSF). The brain floats in CSF, which acts as a cushion and shock absorber.
The brain
The brain contains structurally and functionally defined regions. In mammals, these include the cerebral cortex, basal ganglia, thalamus, hypothalamus, limbic system, cerebellum, and brainstem—although structures in some of these designations overlap. While functions may be primarily localised to one structure in the brain, most complex functions, like language and sleep, involve neurons in multiple brain regions.
Each hemisphere contains regions called lobes that are involved in different functions. The cerebral cortex is a thick piece of nervous system tissue that forms the outermost part of the brain. Each hemisphere of the mammalian cerebral cortex can be broken down into four functionally and spatially defined lobes: frontal, parietal, temporal, and occipital (Figure 10.4).
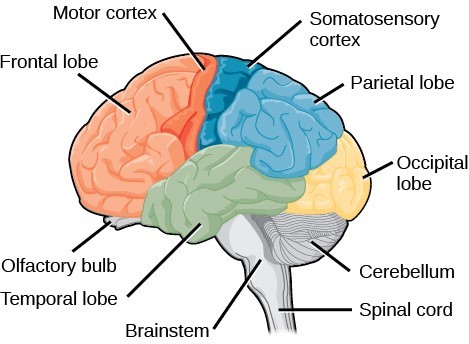
Lobes of the brain
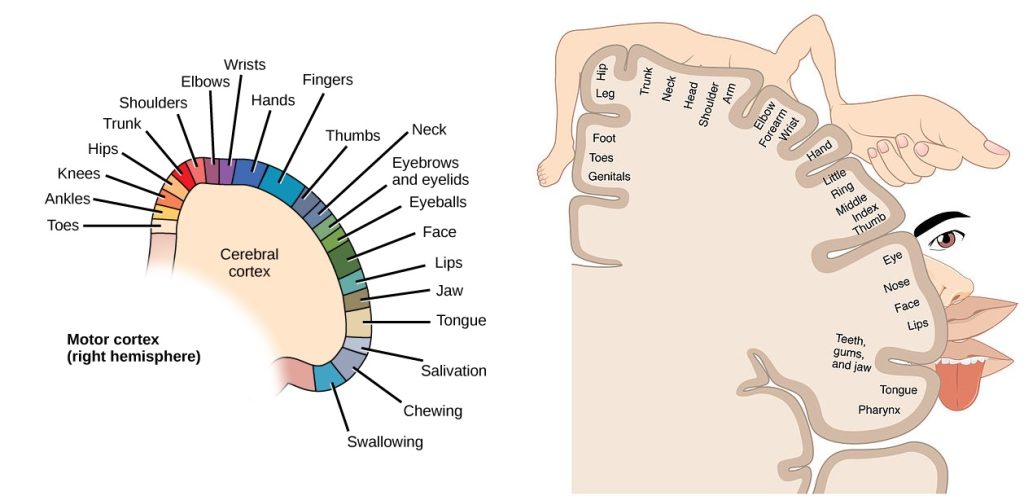
The frontal lobe is located at the front of the brain, over the eyes. This lobe contains the olfactory bulb, which processes smells. The frontal lobe also contains the motor cortex, which is important for planning and implementing movement. Areas within the motor cortex map to different muscle groups (Figure 10.5). This means that stimulation of specific points on the motor cortex will elicit a response in specific areas of the body. From this mapping, it was found that some areas of the body responded to greater areas of the brain. Neurons in the frontal lobe also control cognitive functions like maintaining attention, speech, and decision-making. Studies of humans who have damaged their frontal lobes show that parts of this area are involved in personality, socialisation, and assessing risk.
Watch this video [5:58] to find out more about the development and validity of the homunculus (little man) representation of the motor and somatosensory cortices.
The parietal lobe is located at the top of the brain. Neurons in the parietal lobe are involved in speech and also reading. Two of the parietal lobe’s main functions are processing somatosensation—touch sensations like pressure, pain, heat, cold—and processing proprioception—the sense of how parts of the body are oriented in space. The parietal lobe contains a somatosensory map (Figure 10.12) of the body similar to the motor cortex.
The occipital lobe is located at the back of the brain. It is primarily involved in vision—seeing, recognising, and identifying the visual world.
The temporal lobe is located at the base of the brain and is primarily involved in processing and interpreting sounds.
Other parts of the brain
It also contains the hippocampus (named from the Greek for seahorse, which it resembles in shape) a structure that processes memory formation. The role of the hippocampus in memory was partially determined by studying one famous epileptic patient, HM, who had both sides of his hippocampus removed in an attempt to cure his epilepsy. His seizures went away, but he could no longer form new memories (although he could remember some facts from before his surgery and could learn new motor tasks).
Interconnected brain areas called the basal ganglia play important roles in movement control and posture. The basal ganglia also regulate motivation.
The thalamus acts as a gateway to and from the cortex. It receives sensory and motor inputs from the body and also receives feedback from the cortex. This feedback mechanism can modulate conscious awareness of sensory and motor inputs depending on the attention and arousal state of the animal. The thalamus helps regulate consciousness, arousal, and sleep states.
Below the thalamus is the hypothalamus. The hypothalamus controls the endocrine system by sending signals to the pituitary gland. Among other functions, the hypothalamus is the body’s thermostat—it makes sure the body temperature is kept at appropriate levels. Neurons within the hypothalamus also regulate circadian rhythms, sometimes called sleep cycles.
The limbic system is a connected set of structures that regulates emotion, as well as behaviours related to fear and motivation. It plays a role in memory formation and includes parts of the thalamus and hypothalamus as well as the hippocampus. One important structure within the limbic system is a temporal lobe structure called the amygdala. The two amygdala (one on each side) are important both for the sensation of fear and for recognising fearful faces.
The cerebellum (cerebellum = little brain) sits at the base of the brain on top of the brainstem. The cerebellum controls balance and aids in coordinating movement and learning new motor tasks. The cerebellum of birds is large compared to other vertebrates because of the coordination required by flight (structure and function).
The brainstem connects the rest of the brain with the spinal cord and regulates some of the most important and basic functions of the nervous system including breathing, swallowing, digestion, sleeping, walking, and sensory and motor information integration.
The cerebral cortex, limbic system, and basal ganglia make up the two cerebral hemispheres. A thick fibre bundle called the corpus callosum (corpus = body; callosum = tough) connects the two hemispheres. Although there are some brain functions that are localised more to one hemisphere than the other, the functions of the two hemispheres are largely redundant. In fact, sometimes (very rarely) an entire hemisphere is removed to treat severe epilepsy. While patients do suffer some deficits following the surgery, they can have surprisingly few problems, especially when the surgery is performed on children who have very immature nervous systems.
In other surgeries to treat severe epilepsy, the corpus callosum is cut instead of removing an entire hemisphere. This causes a condition called split-brain, which gives insights into unique functions of the two hemispheres. For example, when an object is presented to patients’ left visual field, they may be unable to verbally name the object (and may claim to not have seen an object at all). This is because the visual input from the left visual field crosses and enters the right hemisphere and cannot then signal to the speech centre, which generally is found in the left side of the brain. Remarkably, if a split-brain patient is asked to pick up a specific object out of a group of objects with the left hand, the patient will be able to do so but will still be unable to verbally identify it.
The spinal cord
The spinal cord is the information superhighway that connects the brain with the rest of the body through its connections with peripheral nerves. It transmits sensory and motor input and also controls motor reflexes. The spinal cord is contained within the meninges and the bones of the vertebral column but is able to communicate signals to and from the body through its connections with spinal nerves (part of the peripheral nervous system).
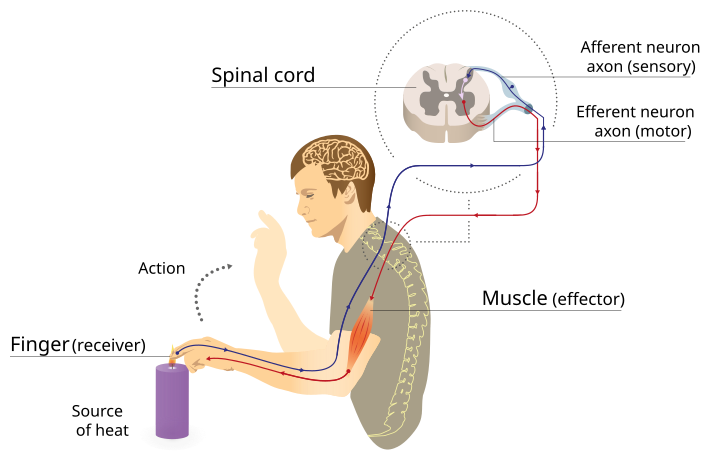
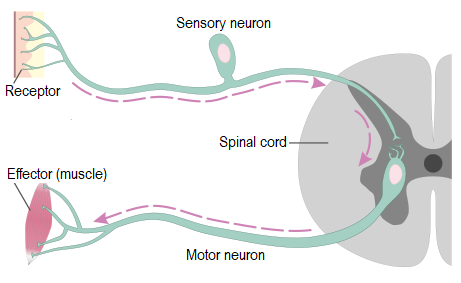
The spinal cord also controls motor reflexes. These reflexes are quick, unconscious movements—like automatically removing a hand from a hot object. Reflexes are so fast because they involve local synaptic connections. For example, the knee reflex that a doctor tests during a routine physical is controlled by a single synapse between a sensory neuron and a motor neuron.
The peripheral nervous system
The peripheral nervous system (PNS) is the connection between the central nervous system and the rest of the body. The PNS can be broken down into the somatic nervous, and the autonomic nervous system. Both of these divisions consist of sensory neurons (afferent neurons) which transmit sensory information from the body (sensation) to the CNS where integration occurs. A message is then sent from the CNS to muscles or glands via the motor neurons (efferent neurons), which causes the response. The main difference between these two divisions is that the autonomic nervous system is largely involuntary or happening automatically, while the somatic nervous system is controlling skeletal muscles, which are mostly voluntary (except for reflexes).
The somatic nervous system
The somatic nervous system is made up of cranial and spinal nerves. These nerve fibres contain both sensory and motor neurons. Recall that sensory neurons transmit sensory information from receptors in the skin, skeletal muscle, and sensory organs to the CNS and motor neurons transmit messages about desired movement from the CNS to the muscles to make them contract.
Voluntary movement
For voluntary movement, the process of integration in the brain is quite complex and requires the input of many different regions of the brain. For example, the frontal lobe is where executive function occurs, so it is where decisions about movement are made; the cerebellum helps to coordinate the movement so, and the some of the basal ganglia are required to initiate and stop movements. Once all of that is processed the messages can be sent to the appropriate muscle to react (Figure 10.6).
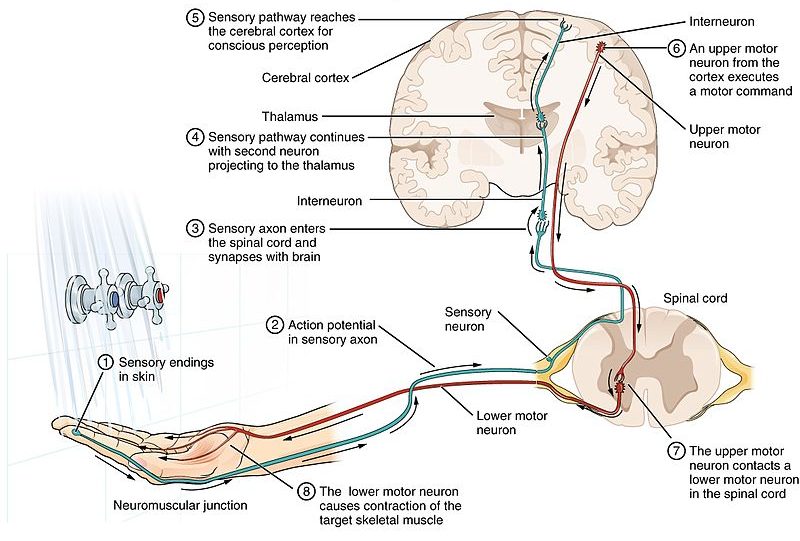
Reflex arc
For reflex movement, such as closing the eyelid to avoid something hitting your eye, the trip reflex, or the knee jerk reflex, information is not integrated in the brain because the time delay might be too long to avoid injury. Instead, integration occurs in the spinal cord. There are a couple of different types of reflexes with regard to the neural pathway involved. Reflexes can involve an interneuron (Figure 10.7) in the spinal cord, which is the link between the sensory neuron and the motor neuron, or they can occur without an interneuron, where the sensory neuron synapses directly with the motor neuron (Figure 10.8). Sensory information is still passed to the brain, so that it knows what has happened.
The autonomic nervous system
The autonomic nervous system serves as the relay between the CNS and the internal organs. It controls the lungs, the heart, smooth muscle, and exocrine and endocrine glands. The autonomic nervous system controls these organs largely without conscious control; it can continuously monitor the conditions of these different systems and implement changes as needed. There are two divisions of the autonomic nervous system that often have opposing effects: the sympathetic nervous system and the parasympathetic nervous system (Figure 10.9).
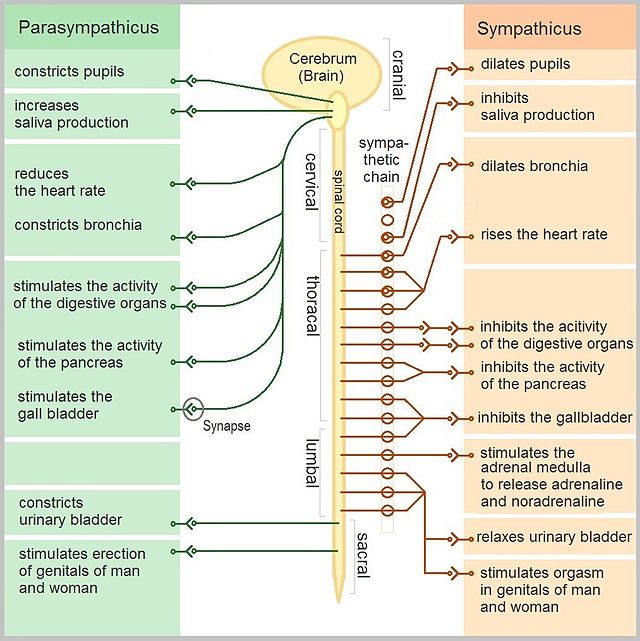
The sympathetic nervous system is responsible for the immediate responses an animal makes when it encounters a dangerous situation. One way to remember this is to think of the fight-or-flight response a person feels when encountering a snake (snake and sympathetic both begin with s). Examples of functions controlled by the sympathetic nervous system include an accelerated heart rate and inhibited digestion. These functions help prepare an organism’s body for the physical strain required to escape a potentially dangerous situation or to fend off a predator. While the sympathetic nervous system is activated in stressful situations, the parasympathetic nervous system allows an animal to rest and digest. One way to remember this is to think that during a restful situation like a picnic, the parasympathetic nervous system is in control (picnic and parasympathetic both start with p). The parasympathetic nervous system resets organ function after the sympathetic nervous system is activated including slowing of heart rate, lowered blood pressure, and stimulation of digestion.
How do nerve cells communicate with each other and the rest of the body?
Communication in the nervous system occurs by way of specialised cells called neurons. Communication signals travel through the neuron and from neuron-to-neuron or neuron to target tissues. The collection of neurons and their support cells makes up the nervous system.
What are the parts of a neuron?
The nervous system is made up of specialised cells – neurons and glia. Glia are non-neuronal cells in the nervous system that support neuronal development and signalling. Neurons are specialised cells that are capable of sending electrical as well as chemical signals. A neuron can have one or more dendrites, which receive these signals, and an axon that sends signals to other neurons or tissues.
Some axons are covered with a special structure called a myelin sheath, which acts as an insulator to keep the electrical signal from dissipating as it travels down the axon. This insulation is important, as the axon from a human motor neuron can be as long as a meter (3.2ft)—from the base of the spine to the toes. The myelin sheath is produced by glial cells. Along the axon there are periodic gaps in the myelin sheath. These gaps are called nodes of Ranvier and are sites where the signal is “recharged” as it travels along the axon (Figure 10.10). When the myelin insulation of axons is compromised, disease results (refer to the section on Diseases of the nervous system later on in this chapter).

To understand how neurons are able to communicate, it is necessary to describe the role of an excitable membrane in generating these signals. The basis of this communication is the generation of electrical signals that arise through sequential changes in the membrane potential.
What is the resting membrane potential?
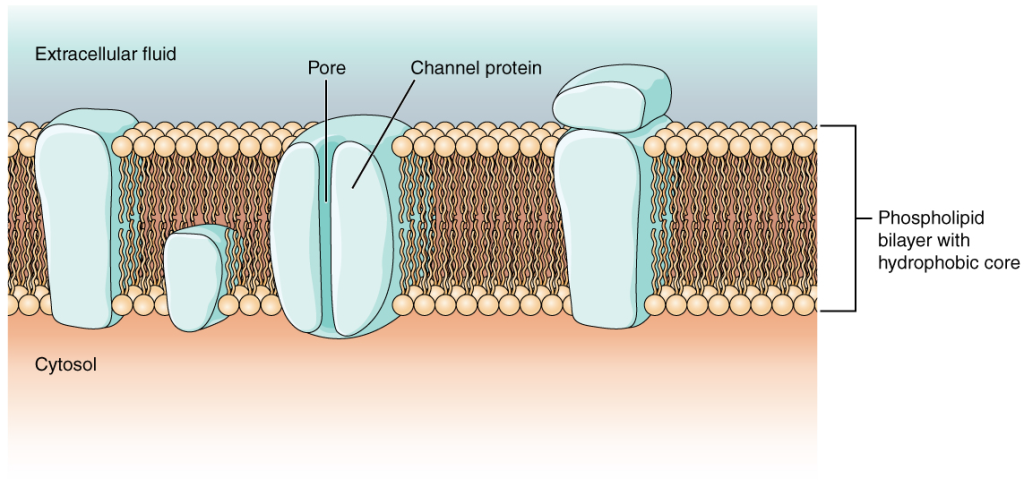
As you learned earlier in Chapter 5: Membrane transport, the cell membrane is primarily responsible for regulating what can cross the membrane and what stays on only one side. The cell membrane is a phospholipid bilayer, so only substances that can pass directly through the hydrophobic core can diffuse through unaided. Charged particles, which are hydrophilic by definition, cannot pass through the cell membrane without assistance (Figure 10.11). Transmembrane proteins, specifically channel proteins, make this possible. These proteins are called ion channels. Several passive transport channels, as well as active transport pumps, are necessary to generate a transmembrane potential and an action potential. Of special interest is the carrier protein referred to as the sodium/ potassium pump that moves sodium ions (Na+) out of a cell and potassium ions (K+) into a cell, thus regulating ion concentration on both sides of the cell membrane.
The sodium/potassium pump requires energy in the form of adenosine triphosphate (ATP). The concentration of Na+ is higher outside the cell than inside, and the concentration of K+ is higher inside the cell than outside. That means that this pump is moving the ions against the concentration gradients for sodium and potassium, which is why it requires energy. In fact, the function of the pump is to maintain those concentration gradients.
A short video description of the action of the sodium-potassium pump [2:26]. By RicochetScience
A potential is a distribution of charge across the cell membrane, measured in millivolts (mV). The standard is to compare the inside of the cell relative to the outside, so the membrane potential is a value representing the charge on the intracellular side of the membrane based on the outside being zero, relatively speaking (Figure 10.12).
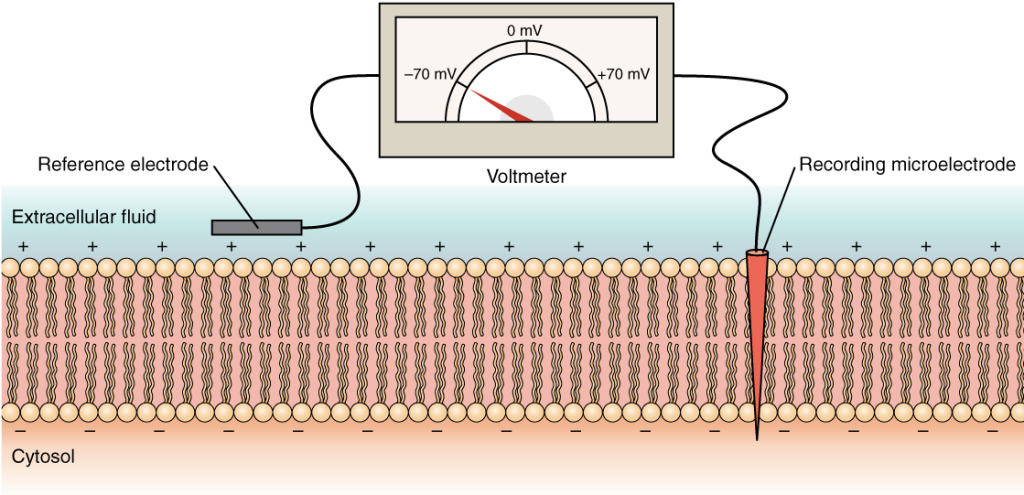
When the cell is at rest, and the ion channels are closed (except for leak channels which randomly open), ions are distributed across the membrane in a very predictable way. The concentration of Na+ outside the cell is 10 times greater than the concentration inside. Also, the concentration of K+ inside the cell is greater than outside. Another important factor to consider is that the cytoplasm contains a high concentration of anions, in the form of phosphate ions and negatively charged proteins. Therefore, overall, the inside of the membrane is negatively charged compared to the outside. If we measure that difference using the equipment in Figure 10.12, we would get a charge -70 mV and this is called the resting membrane potential. When a nerve is stimulated, there is a change in the distribution of ions, and therefore a change in the membrane potential. This generates an action potential, which can be propagated along the axon of the nerve to the axon terminal.
How do ion channels open and close?
To get an electrical signal started, the membrane potential has to change, and this involves the opening of certain types of ion channels.
As discussed earlier, ion channels are pores that allow specific charged particles to cross the membrane in response to an existing concentration gradient. Ion channels do not always freely allow ions to diffuse across the membrane. Some are opened by certain events, meaning the channels are gated. Channels can be categorised on the basis of how they are gated. The main types of gated channels are:
- Mechanically-gated channels: opened by pressure /stress (e.g. touch)
- Temperature-gated channels
- Ligand-gated channels – need a chemical messenger
- Voltage-gated channels
- Leak channels: are randomly gated, and need no actual event to open them
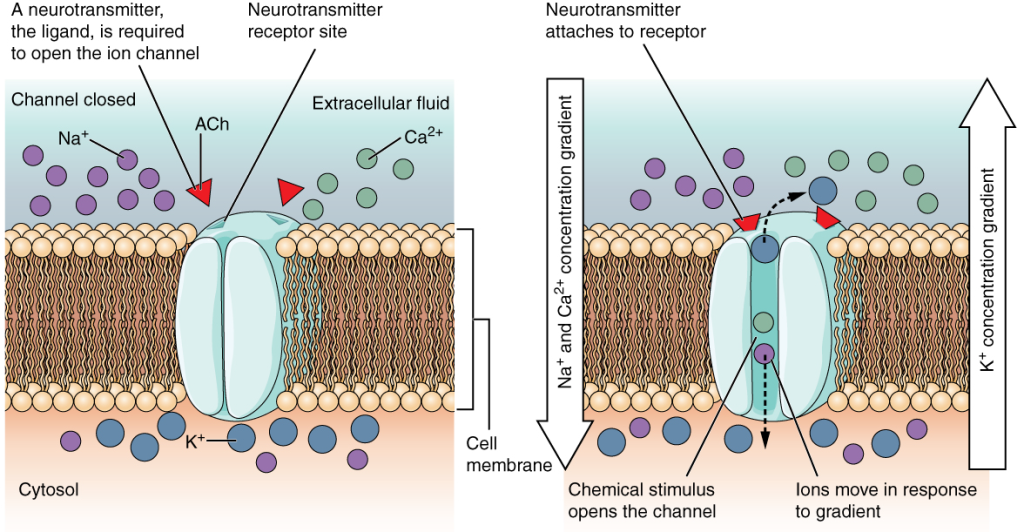
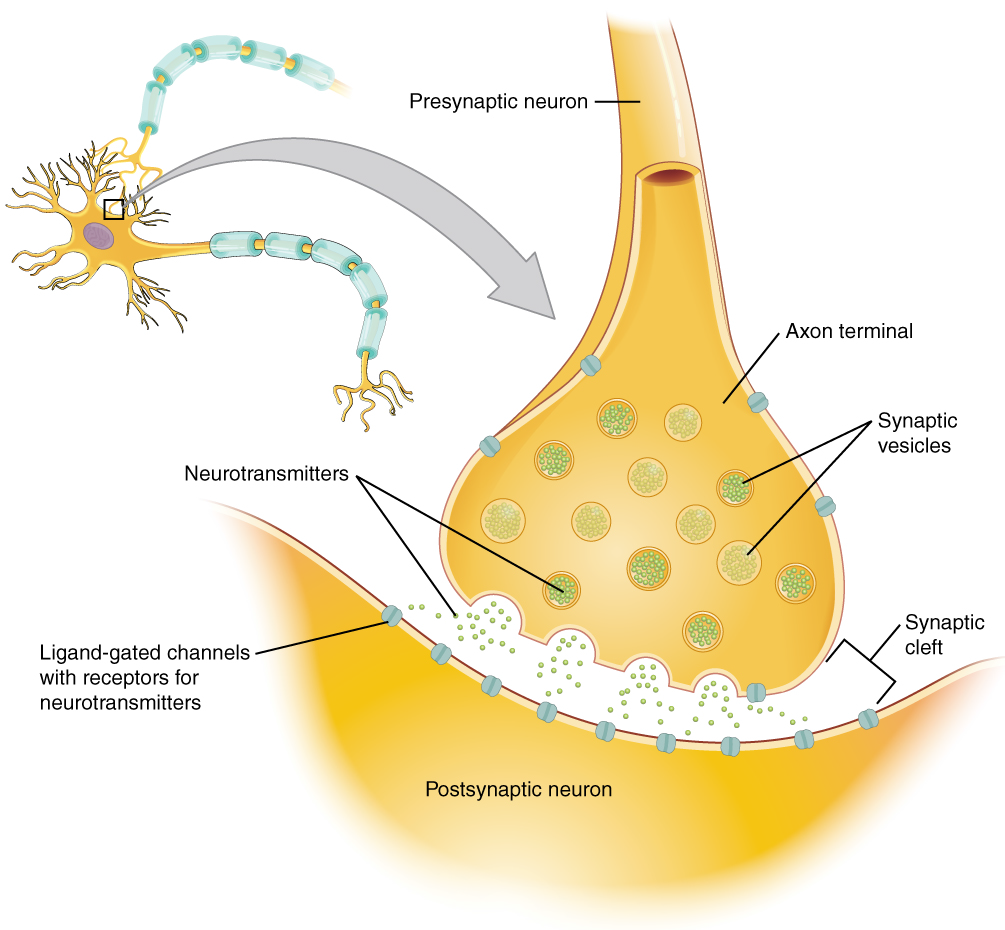
Two gated ion channels involved in the generation of the action potential are ligand-gated channels and voltage-gated channels. A ligand-gated channel opens because a signalling molecule, a ligand, binds to the extracellular region of the channel. When the ligand, known as a neurotransmitter in the nervous system, binds to the protein, ions cross the membrane changing its charge (Figure 10.13).
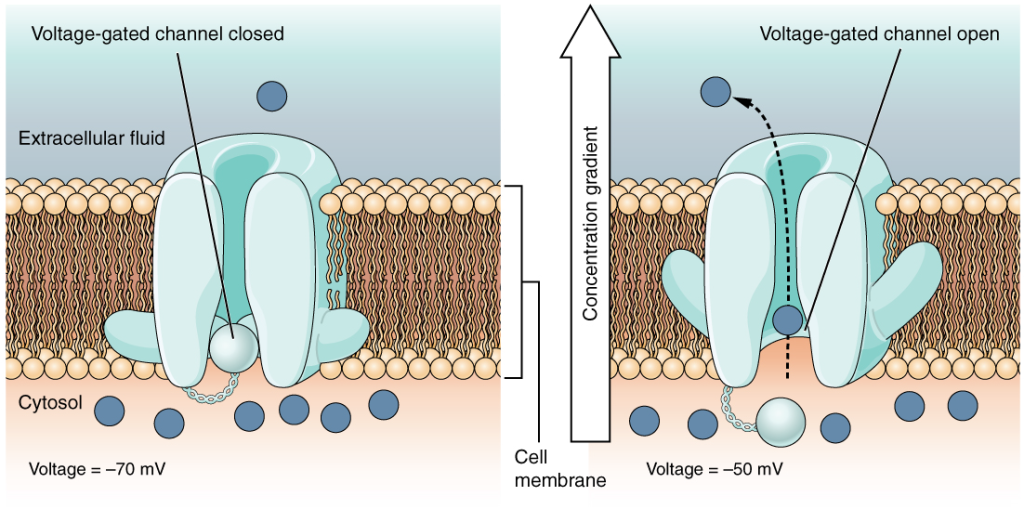
A voltage-gated channel is a channel that responds to changes in the electrical properties of the membrane in which it is embedded. Normally, at rest, the inner portion of the membrane is at a negative voltage. This is called the resting membrane potential. When that voltage becomes less negative, the channel begins to allow ions to cross the membrane (Figure 10.14).
What is an action potential?
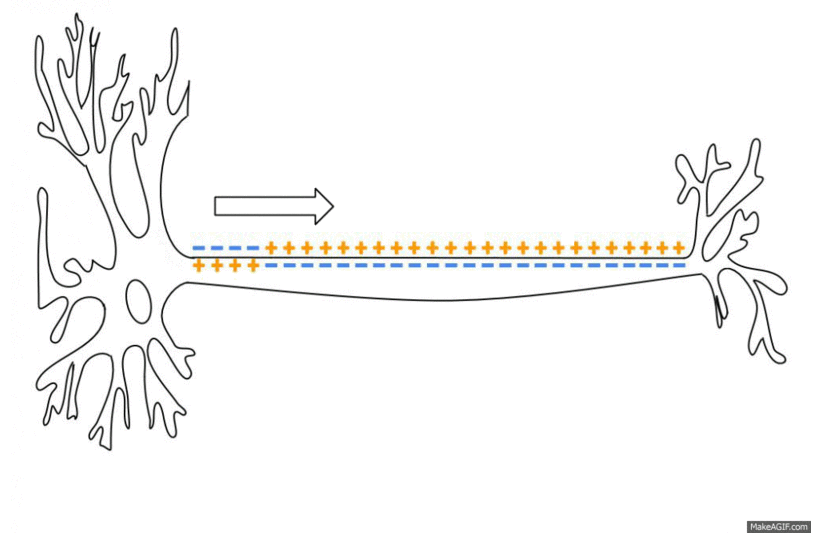
Voltage-gated channels are present along the axon of the neuron (Figure 10.15). Once the ligand-gated channel opens, the Na+ ions rush in (down their concentration gradient), which changes the voltage inside the axon. This causes the first voltage-gated channels to open, allowing more Na+ in. This continues, activating voltage-gated channels along the length of the axon. This is known as the propagation of an action potential. When the electrical signal reaches the axon terminal, it triggers the release of neurotransmitter.
View this animation of what the ions are doing at the membrane during an action potential [10:25]. © Osmosis
How do neurons communicate?
All functions performed by the nervous system require neurons to communicate with one another. The process by which a neuron communicates with another neuron is called neurotransmission (Figure 10.16). Neurons communicate between the axon of one neuron and the dendrites, and sometimes the cell body, of another neuron across the gap between them, known as the synaptic cleft. When an action potential reaches the end of an axon it stimulates the release of neurotransmitter molecules from the presynaptic neuron into the synaptic cleft. The neurotransmitter is released through exocytosis of vesicles containing the neurotransmitter molecules. The neurotransmitter diffuses across the synaptic cleft and binds to receptors in the post-synaptic membrane of the dendrite or soma (cell body) of the next neuron. These receptor molecules are the ligand-gated ion channels, which will open, allowing sodium to enter the cell. If sufficient neurotransmitter has been released an action potential may be initiated in the next cell, but this is not guaranteed. If insufficient neurotransmitter is released the nerve signal will die at this point.
Watch this video to learn about the release of a neurotransmitter [6:27].
Disorders of the nervous system
Multiple sclerosis (MS) is one such disease. It is an example of an autoimmune disease. The antibodies produced by lymphocytes (a type of white blood cell) mark myelin as something that should not be in the body. This causes inflammation and the destruction of the myelin in the central nervous system. As the insulation around the axons is destroyed by the disease, scarring becomes obvious. This is where the name of the disease comes from; sclerosis means hardening of tissue, which is what a scar is. Multiple scars are found in the white matter of the brain and spinal cord. Control of the musculature is compromised, as is control of organs such as the bladder.
Glioblastomas represent most brain tumours and are caused by mutations in glia. While glial cells are often thought of as the supporting cast of the nervous system, the number of glial cells in the brain actually outnumbers the number of neurons by a factor of 10. Neurons would be unable to function without the vital roles that are fulfilled by these glial cells. Glia guide developing neurons to their destinations, buffer ions and chemicals that would otherwise harm neurons, and provide myelin sheaths around axons.
Career Connection: Neurophysiologist
Understanding how the nervous system works could be a driving force in your career. Studying neurophysiology is a very rewarding path to follow. It means that there is a lot of work to do, but the rewards are worth the effort.
The career path of a research scientist can be straightforward: university: undergraduate degree, postgraduate degree, postdoctoral research, academic research position at a university. A Bachelor’s degree in science will get you started, and for neurophysiology that might be in biology, psychology, computer science, engineering, or neuroscience. But the real specialisation comes in your during your postgraduate years. There are many different programs out there to study the nervous system, not just neuroscience itself. Many postgraduate programs are doctoral, and at least three years are dedicated to finding a research topic and pursuing that with a near single-mindedness. The research will usually result in a few publications in scientific journals, which will make up the bulk of a doctoral dissertation. After graduating with a Ph.D., researchers will go on to find specialised work called a postdoctoral fellowship within established labs. In this position, a researcher starts to establish their own research career with the hopes of finding an academic position at a research university.
Other options are available if you are interested in how the nervous system works. Especially for neurophysiology, a medical degree might be more suitable so you can learn about the clinical applications of neurophysiology and possibly work with human subjects. An academic career is not a necessity. Biotechnology firms are eager to find motivated scientists ready to tackle the tough questions about how the nervous system works so that therapeutic chemicals can be tested on some of the most challenging disorders such as nervous system disorders such Alzheimer’s disease or Parkinson’s disease, or spinal cord injury.
Others with a medical degree and a specialisation in neuroscience go on to work directly with patients, diagnosing and treating mental disorders. You can do this as a psychiatrist, a neuropsychologist, a neuroscience nurse, or a neurodiagnostic technician, among other possible career paths.
10.3 | The endocrine system
Communication is a process in which a sender transmits signals to one or more receivers to control and coordinate actions. In the human body, two major organ systems participate in relatively long distance communication: the nervous system and the endocrine system. Together, these two systems are primarily responsible for maintaining homeostasis in the body. When you look at the model for the feedback loops from Chapter 2: Maintaining a balance, these systems are the way that the message is passed from one part of the loop to the next.
As discussed above, the nervous system uses two types of intercellular communication—electrical and chemical signalling—either by the direct action of an electrical potential, or in the latter case, through the action of chemical neurotransmitters such as serotonin or acetylcholine. Neurotransmitters act locally and rapidly.
In contrast, the endocrine system uses just one method of communication: chemical signalling. These signals are sent by the endocrine organs, which secrete chemicals—the hormone—into the extracellular fluid. Hormones are transported primarily via the bloodstream throughout the body, where they bind to receptors on target cells, inducing a characteristic response. The number of receptors on a target cell can increase or decrease in response to hormone activity.
Hormone levels are primarily controlled through negative feedback, in which rising levels of a hormone inhibit its further release. The endocrine system produces hormones that function to control and regulate many different body processes. Many of the hormones are secreted in response to signals from the nervous system, thus the two systems act in concert to effect changes in the body.
What are hormones?
Maintaining homeostasis within the body requires the coordination of many different systems and organs. One mechanism of communication between neighbouring cells, and between cells and tissues in distant parts of the body, occurs through the release of chemicals called hormones. The hormones of the human body can be divided into two major groups on the basis of their chemical structure: those derived from amino acids; and those derived from lipids (often called steroid hormones).
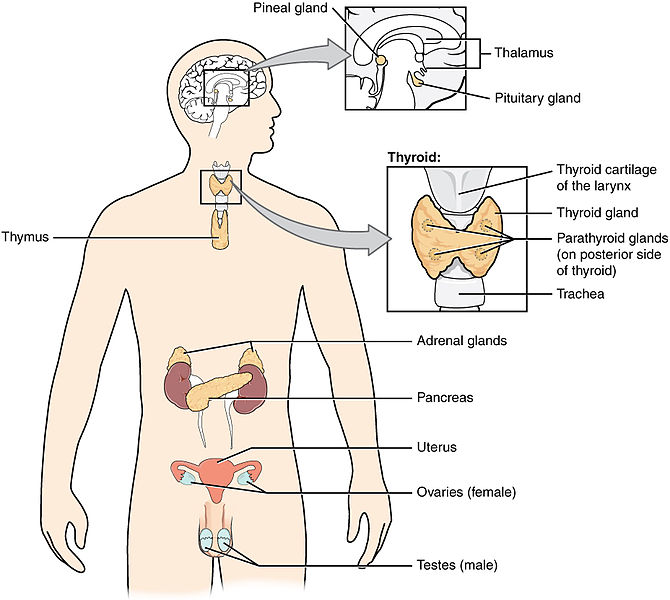
Hormones are released into body fluids, usually blood, which carries them to their target cells where they elicit a response. The cells that secrete hormones are often located in specific organs, called endocrine glands, and the cells, tissues, and organs that secrete hormones make up the endocrine system. Examples of endocrine organs include the pancreas, which produces the hormones insulin and glucagon to regulate blood-glucose levels, the adrenal glands, which produce hormones such as adrenaline (epinephrine) and noradrenaline (norepinephrine) that regulate responses to stress, and the thyroid gland, which produces thyroid hormones that regulate metabolic rates.
The endocrine glands differ from the exocrine glands. Exocrine glands secrete chemicals through ducts that lead outside the gland (not to the blood). For example, sweat produced by sweat glands is released into ducts that carry sweat to the surface of the skin. The pancreas has both endocrine and exocrine functions because besides releasing hormones into the blood. It also produces digestive juices, which are carried by ducts into the small intestine
What causes hormones to be released?
There are three mechanisms by which endocrine glands are stimulated to synthesise and release hormones: humoral stimuli, hormonal stimuli and neural stimuli.
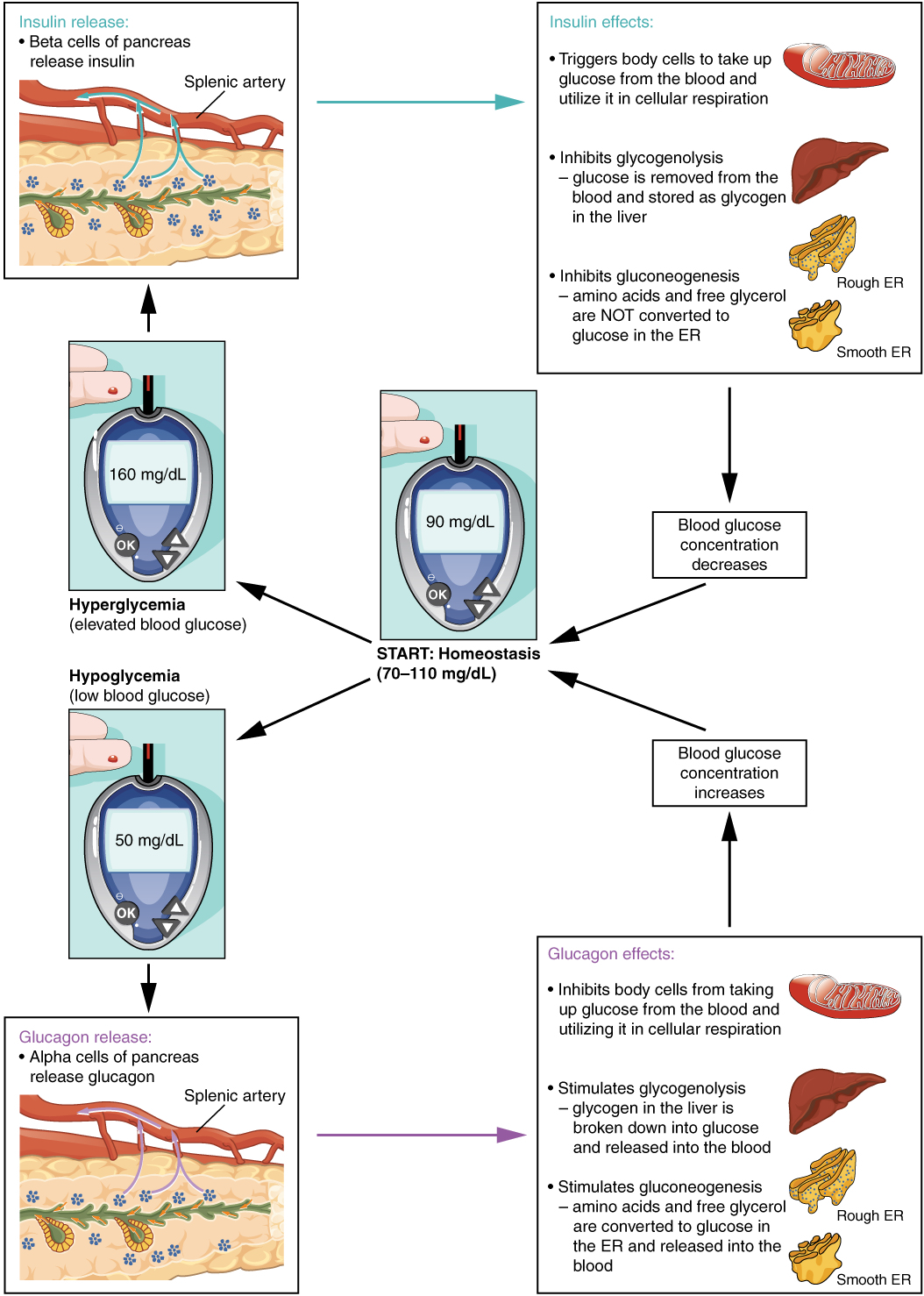
The term humoral is derived from the term humor, which refers to bodily fluids such as blood. A humoral stimulus refers to the control of hormone release in response to changes in extracellular fluids such as blood or the ion concentration in the blood. For example, a rise in blood glucose levels triggers the pancreatic release of insulin. Insulin causes blood glucose levels to drop, which signals the pancreas to stop producing insulin in a negative feedback loop.
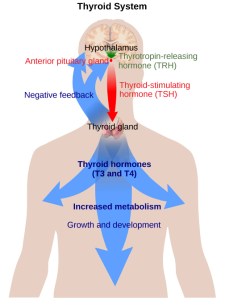
Hormonal stimuli refer to the release of a hormone in response to another hormone. A number of endocrine glands release hormones when stimulated by hormones released by other endocrine glands. For example, the hypothalamus produces hormones that stimulate the anterior portion of the pituitary gland. The anterior pituitary in turn releases hormones that regulate hormone production by other endocrine glands. The anterior pituitary releases the thyroid-stimulating hormone, which then stimulates the thyroid gland to produce the hormones T3 and T4. As blood concentrations of T3 and T4 rise, they inhibit both the pituitary and the hypothalamus in a negative feedback loop (see Figure 10.17).
In some cases, the nervous system directly stimulates endocrine glands to release hormones, which is referred to as neural stimuli. Recall that in a short-term stress response, the hormones epinephrine and norepinephrine are important for providing the bursts of energy required for the body to respond. Here, neuronal signalling from the sympathetic nervous system directly stimulates the adrenal medulla to release the hormones epinephrine and norepinephrine in response to stress.
How do hormones work?
Hormones cause changes in target cells by binding to specific cell-surface or intracellular hormone receptors, molecules embedded in the cell membrane or floating in the cytoplasm with a binding site that matches a binding site on the hormone molecule. Using the information above, can you guess which hormones will need cell-surface receptors, and which ones can use intracellular receptors? In this way, even though hormones circulate throughout the body and come into contact with many different cell types, they only affect cells that possess the necessary receptors. Receptors for a specific hormone may be found on or in many different cells or may be limited to a small number of specialised cells. For example, thyroid hormones act on many different tissue types, stimulating metabolic activity throughout the body. Cells can have many receptors for the same hormone but often also possess receptors for different types of hormones. The number of receptors that respond to a hormone determines the cell’s sensitivity to that hormone, and the resulting cellular response. Additionally, the number of receptors available to respond to a hormone can change over time, resulting in increased or decreased cell sensitivity. In up-regulation, the number of receptors increases in response to declining hormone levels, making the cell more sensitive to the hormone and allowing for more cellular activity. When the number of receptors decreases in response to rising hormone levels, called down-regulation, cellular activity is reduced. This process allows cells to be more sensitive to the hormone that is present. Cells can also alter the sensitivity of the receptors themselves to various hormones.
What are the endocrine glands?
The endocrine glands secrete hormones into the surrounding interstitial fluid; those hormones then diffuse into blood and are carried to various organs and tissues within the body (Figure 10.17). A very brief overview of some of the endocrine glands and their hormones follows.
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts. Examples of exocrine glands include the sebaceous and sweat glands of the skin and salivary glands. The secretions from these glands are not hormones.
Endocrine Gland |
Associated Hormones |
Effect |
| Pituitary (anterior) | growth hormone | promotes growth of body tissues |
| prolactin | promotes milk production | |
| thyroid-stimulating hormone | stimulates thyroid hormone release | |
| adrenocorticotropic hormone | stimulates hormone release by adrenal cortex | |
| follicle-stimulating hormone | stimulates gamete production | |
| luteinizing hormone | stimulates androgen production by gonads in males; stimulates ovulation and production of estrogen and progesterone in females | |
| Pituitary (posterior) | antidiuretic hormone | stimulates water absorption by kidneys |
| oxytocin | stimulates uterine contractions during childbirth | |
| Thyroid | thyroxine, triiodothyronine | stimulates metabolism |
| calcitonin | reduces blood Ca2+ levels | |
| Parathyroid | parathyroid hormone | increases blood Ca2+ levels |
| Adrenal (cortex) | aldosterone | increases blood Na+ levels |
| cortisol, corticosterone, cortisone | increase blood-glucose levels | |
| Adrenal (medulla) | epinephrine, norepinephrine | stimulate fight-or-flight response |
| Pancreas | insulin | reduces blood-glucose levels |
| glucagon | increases blood-glucose levels |
The pituitary gland is often referred to as the Master Gland, because it secretes a number of hormones that influence the secretion of hormones from other glands. In reality, the hypothalamus–pituitary complex can be thought of as the command centre of the endocrine system. The hypothalamus is the control centre of a number of feedback loops. It secretes two hormones that directly produce responses in target tissues (see Table 10.1). As an example, ADH (antidiuretic hormone) is produced by neurosecretory cells of the hypothalamus and released from the posterior pituitary. ADH acts directly on the kidney (effector) to influence water reabsorption (response). In addition to targeting tissues directly, neurosecretory cells of the hypothalamus produce hormones that promote or inhibit secretion of hormones from the anterior pituitary. These anterior pituitary hormones act on other endocrine glands. This produces a more complex negative feedback loop, which can be influenced at both the level of the hypothalamus and the level of the anterior pituitary gland.
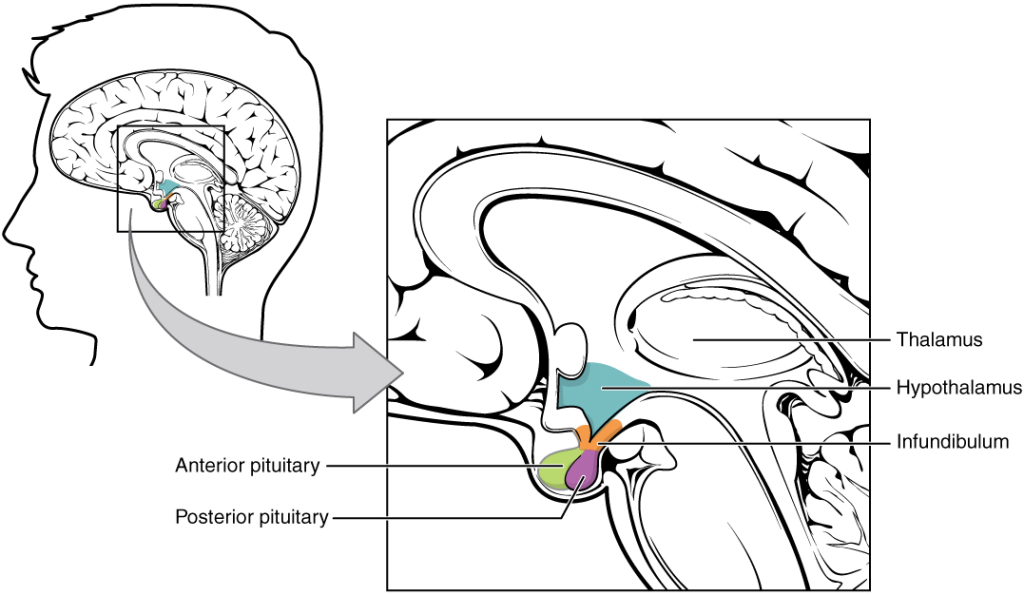
Pituitary gland
The pituitary gland is located at the base of the brain (Figure 10.18). It is attached to the hypothalamus by a stalk-like infundibulum. The posterior pituitary gland is significantly different in structure from the anterior pituitary, it is a part of the brain, extending down from the hypothalamus, and contains mostly nerve fibres that extend from the hypothalamus to the posterior pituitary which stores and releases the hormones oxytocin and antidiuretic hormone (ADH) that were produced by the hypothalamus. The anterior pituitary on the other hand responds to hormones produced by the hypothalamus by producing its own hormones , most of which in turn regulate other hormone-producing glands, for instance Thyroid stimulating hormone stimulates the thyroid gland (refer to Table 10.2).
Posterior pituitary
Oxytocin (tocia- = childbirth) stimulates uterine contractions and dilation of the cervix. Throughout most of pregnancy, oxytocin hormone receptors are not expressed at high levels in the uterus. Toward the end of pregnancy, the synthesis of oxytocin receptors in the uterus increases, and the smooth muscle cells of the uterus become more sensitive to its effects. Oxytocin is continually released throughout childbirth through a positive feedback mechanism.
Antidiuretic Hormone (ADH) is released from the posterior pituitary in response to high blood osmolarity during dehydration or following a very salty meal. The osmoreceptors signal the posterior pituitary to release ADH. The target cells of ADH are located in the tubular cells of the kidneys. Its effect is to increase epithelial permeability to water, allowing increased water reabsorption. The more water reabsorbed from the filtrate, the greater the amount of water that is returned to the blood and the less that is excreted in the urine.
Anterior pituitary
The anterior pituitary produces six hormones: growth hormone, prolactin, thyroid-stimulating hormone, adrenocorticotropic hormone, follicle-stimulating hormone, and luteinising hormone. Growth hormone stimulates cellular activities like protein synthesis that promote growth. Prolactin stimulates the production of milk by the mammary glands. The other hormones produced by the anterior pituitary regulate the production of hormones by other endocrine tissues (Table 10.2).
Growth Hormone (GH): its primary function is anabolic; it promotes protein synthesis and tissue building through direct and indirect mechanisms. GH levels are controlled by the release of factors from the hypothalamus. GH indirectly mediates growth and protein synthesis by triggering the liver and other tissues to produce a group of proteins that stimulate cellular multiplication and growth.
Dysfunction of the endocrine system’s control of growth can result in several disorders. For example, gigantism is a disorder in children that is caused by the secretion of abnormally large amounts of GH, resulting in excessive growth. A similar condition in adults is acromegaly, a disorder that results in the growth of bones in the face, hands, and feet in response to excessive levels of GH in individuals who have stopped growing. Abnormally low levels of GH in children can cause growth impairment—a disorder called pituitary dwarfism (also known as growth hormone deficiency).
Thyroid gland
Thyroid stimulating hormone (TSH) from the anterior pituitary stimulates the thyroid gland which is located in the neck, just below the larynx and in front of the trachea (Figure 10.17). It is a butterfly-shaped gland with two lobes that are connected. The thyroid follicle cells synthesise and release the hormone thyroxine (T4), and triiodothyronine (T3). Both T3 and T4 have the effect of stimulating metabolic activity in the body and increasing energy use. A third hormone, calcitonin, is also produced by the thyroid. Calcitonin is released in response to rising calcium ion concentrations (stimulus) in the blood and has the effect of reducing those levels (response).
Thyroid
Iodine Deficiency, Hypothyroidism, and Hyperthyroidism: Dietary iodine is required for the synthesis of T3 and T4. But for much of the world’s population, foods do not provide adequate levels of this mineral, because the amount varies according to the level in the soil in which the food was grown, as well as the irrigation and fertilisers used. Marine fish and shrimp tend to have high levels because they concentrate iodine from seawater, but many people in landlocked regions lack access to seafood. Thus, the primary source of dietary iodine in many countries is iodized salt.
Dietary iodine deficiency can result in the impaired ability to synthesise T3 and T4, leading to a variety of severe disorders. When T3 and T4 cannot be produced, TSH is secreted in increasing amounts. As a result of this hyperstimulation, thyroglobulin accumulates in the thyroid gland follicles, increasing their deposits of colloid. The accumulation of colloid increases the overall size of the thyroid gland, a condition called a goitre (Figure 10.19). A goitre is only a visible indication of the deficiency. Other iodine deficiency disorders include impaired growth and development, decreased fertility, and prenatal and infant death. Moreover, iodine deficiency is the primary cause of preventable mental retardation worldwide.

In areas of the world with access to iodized salt, dietary deficiency is rare. Instead, inflammation of the thyroid gland is the more common cause of low blood levels of thyroid hormones. Called hypothyroidism, the condition is characterised by a low metabolic rate, weight gain, cold extremities, constipation, reduced libido, menstrual irregularities, and reduced mental activity. In contrast, hyperthyroidism—an abnormally elevated blood level of thyroid hormones—is often caused by a pituitary or thyroid tumour. Hyperthyroidism can lead to an increased metabolic rate, excessive body heat and sweating, diarrhoea, weight loss, tremors, and increased heart rate. The person’s eyes may bulge (called exophthalmos) as antibodies produce inflammation in the soft tissues of the orbits. The person may also develop a goitre.
Adrenal glands
The adrenal glands are located on top of each kidney (Figure 10.20). The adrenal glands consist of an outer adrenal cortex and an inner adrenal medulla. These regions secrete different hormones.
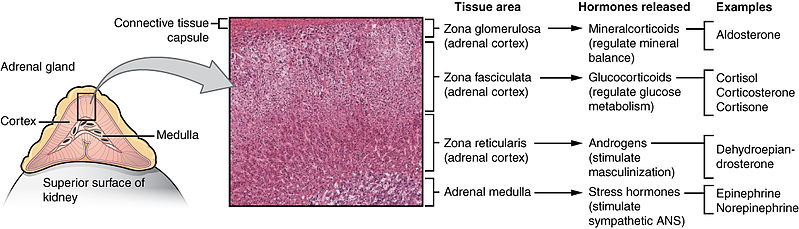
The adrenal cortex produces corticosteroid hormones and androgens. The main mineralocorticoid produced by the cortex is aldosterone, which regulates the concentration of ions in urine, sweat, and saliva. Aldosterone release from the adrenal cortex is stimulated by a decrease in blood concentrations of sodium ions, blood volume, or blood pressure, or by an increase in blood potassium levels. The most important glucocorticoid is cortisol, which plays a part in the stress response by increasing glucose synthesis from fats and proteins and interacting with epinephrine to cause vasoconstriction.
The adrenal medulla contains two types of secretory cells: one that produces epinephrine (adrenaline) and another that produces norepinephrine (noradrenaline). Epinephrine and norepinephrine cause immediate, short-term changes in response to stressors, inducing the so-called fight-or-flight response. The responses include increased heart rate, breathing rate, cardiac muscle contractions, and blood-glucose levels. They also accelerate the breakdown of glucose in skeletal muscles and stored fats in adipose tissue, and redirect blood flow toward skeletal muscles and away from skin and viscera. The release of epinephrine and norepinephrine is stimulated by neural impulses from the sympathetic nervous system that originate from the hypothalamus. Refer to Table 10.2 for a summary of the source and effects of adrenal gland hormones.
| Adrenal gland | Associated hormones | Chemical class | Effect |
| Adrenal cortex | Aldosterone | Steroid | Increase blood Na+ levels |
| Adrenal cortex | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
| Adrenal medulla | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
Pancreas
The pancreas is an elongate organ located between the stomach and the proximal portion of the small intestine (Figure 10.21). It contains both exocrine cells that excrete digestive enzymes, and endocrine cells that release hormones.
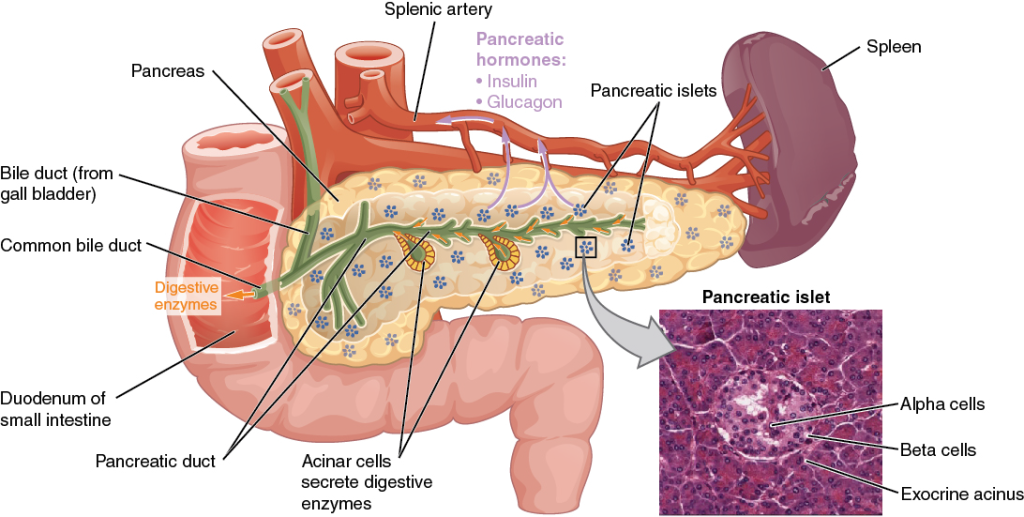
The endocrine cells of the pancreas form clusters called pancreatic islets or the islets of Langerhans. Among the cell types in each pancreatic islet are the alpha cells, which produce the hormone glucagon, and the beta cells, which produce the hormone insulin. These hormones act antagonistically (opposite to each other) to regulate blood-glucose levels. Alpha cells release glucagon as blood-glucose levels decline. When blood-glucose levels rise, beta cells release insulin. Glucagon causes the release of glucose to the blood from the liver (effector), and insulin facilitates the uptake of glucose by the body’s cells (effector) (Figure 10.22). Note that glycogenolysis refers to breakdown of glycogen to glucose, and gluconeogenesis refers to the synthesis of glucose.
Dysfunction of insulin production and secretion, as well as the target cells’ responsiveness to insulin, can lead to a condition called diabetes mellitus. An increasingly common disease, diabetes mellitus has been diagnosed in more than 18 million adults in the United States, and more than 200,000 children. It is estimated that up to 7 million more adults have the condition but have not been diagnosed. In addition, approximately 79 million people in the US are estimated to have pre-diabetes, a condition in which blood glucose levels are abnormally high, but not yet high enough to be classified as diabetes.
Gonads
The gonads – the male testes and female ovaries-produce steroid hormones. The testes produce androgens, testosterone being the most prominent, which allow for the development of secondary sex characteristics and the production of sperm cells. The ovaries produce oestrogen and progesterone, which cause secondary sex characteristics, regulate production of eggs, control pregnancy, and prepare the body for childbirth. The effects of these hormones are summarised in Table 10.3.
| Gonad | Associated hormones | Chemical class | Effect |
| Testes | Testosterone | Steroid | Stimulates development of male secondary sex characteristics and sperm production |
| Testes | Inhibin | Protein | Inhibits FSH release from pituitary |
| Ovaries | Oestrogens and progesterone | Steroid | Stimulate development of female secondary sex characteristic can prepare the body for childbirth |
| Placenta | Human chorionic gonadotropin | Protein | Promotes progesterone synthesis during pregnancy and inhibits immune response against foetus |
Non-endocrine organs with an endocrine function
There are several organs whose primary functions are non-endocrine but that also possess endocrine functions. These include the heart, kidneys, intestines, thymus, and adipose tissue. The heart has endocrine cells in the walls of the atria that release a hormone in response to increased blood volume. It causes a reduction in blood volume and blood pressure, and reduces the concentration of Na+ in the blood.
The gastrointestinal tract produces several hormones that aid in digestion. The endocrine cells are located in the mucosa of the GI tract throughout the stomach and small intestine. The hormones trigger the release of gastric juices, which help to break down and digest food in the GI tract.
The kidneys also possess endocrine function. Two of these hormones regulate ion concentrations and blood volume or pressure. Erythropoietin (EPO) is released by kidneys in response to low oxygen levels. EPO triggers the formation of red blood cells in the bone marrow. EPO has been used by athletes to improve performance. But EPO doping has its risks, since it thickens the blood and increases strain on the heart; it also increases the risk of blood clots and therefore heart attacks and stroke.
How is hormone production regulated?
To prevent abnormal hormone levels and a potential disease state, hormone levels must be tightly controlled. The body maintains this control by balancing hormone production and degradation. Feedback loops govern the initiation and maintenance of most hormone secretion in response to various stimuli. The release of hormones can be caused by changes in blood parameters (humoral) by the action of other hormones (hormonal) or by signals from nerves (neural).
Hormone production and release are primarily controlled by negative feedback, as described previously in the discussion on homeostasis. Negative feedback is characterised by the inhibition of further secretion of a hormone in response to adequate levels of that hormone. This allows blood levels of the hormone to be regulated within a narrow range. For example, the anterior pituitary signals the thyroid to release thyroid hormones. Increasing levels of these hormones in the blood then give feedback to the hypothalamus and anterior pituitary to inhibit further signaling to the thyroid gland (Figure 10.23).
Positive feedback loops are characterised by the release of additional hormone in response to an original hormone release. The release of oxytocin during childbirth is a positive feedback loop. The initial release of oxytocin begins to signal the uterine muscles (effector) to contract (response), which pushes the foetus toward the cervix, causing it to stretch (stimulus). This, in turn, signals the pituitary gland to release more oxytocin, causing labour contractions to intensify. The release of oxytocin decreases after the birth of the child.
Career Connection: Endocrinologist
An endocrinologist is a medical doctor who specialises in treating endocrine disorders. An endocrine surgeon specialises in the surgical treatment of endocrine diseases and glands. Some of the diseases that are managed by endocrinologists include disorders of the pancreas (diabetes mellitus), disorders of the pituitary (gigantism, acromegaly, and pituitary dwarfism), disorders of the thyroid gland (goitre and Graves’ disease), and disorders of the adrenal glands (Cushing’s disease and Addison’s disease).
Endocrinologists are required to assess patients and diagnose endocrine disorders through extensive use of laboratory tests. Many endocrine diseases are diagnosed using tests that stimulate or suppress endocrine organ functioning. Blood samples are then drawn to determine the effect of stimulating or suppressing an endocrine organ on the production of hormones. For example, to diagnose diabetes mellitus, patients are required to fast for 12 to 24 hours. They are then given a sugary drink, which stimulates the pancreas to produce insulin to decrease blood-glucose levels. A blood sample is taken one to two hours after the sugar drink is consumed. If the pancreas is functioning properly, the blood-glucose level will be within a normal range.
Once a disease such as diabetes has been diagnosed, endocrinologists can prescribe lifestyle changes and medications to treat the disease. Some cases of diabetes mellitus can be managed by exercise, weight loss, and a healthy diet; in other cases, medications may be required to enhance insulin’s production or effect. If the disease cannot be controlled by these means, the endocrinologist may prescribe insulin injections.
In addition to clinical practice, endocrinologists may also be involved in primary research and development activities. For example, ongoing islet transplant research is investigating how healthy pancreas islet cells may be transplanted into diabetic patients. Successful islet transplants may allow patients to stop taking insulin injections.
action potential change in voltage of a cell membrane in response to a stimulus that results in transmission of an electrical signal; unique to neurons and muscle fibres
autonomic nervous system (ANS) functional division of the nervous system that is responsible for homeostatic reflexes that coordinate control of cardiac and smooth muscle, as well as glandular tissue
axon single process of the neuron that carries an electrical signal (action potential) away from the cell body toward a target cell
axon terminal end of the axon, where there are usually several branches extending toward the target cell
brain the large organ of the central nervous system composed of white and grey matter, contained within the cranium and continuous with the spinal cord
brainstem connects rest of the brain with the spinal cord, regulates basic functions like breathing swallowing, blood pressure
central nervous system (CNS) anatomical division of the nervous system located within the cranial and vertebral cavities, namely the brain and spinal cord
cerebellum sits at the base of the brain, controls balance, coordination, motor tasks
cerebral cortex outermost layer of grey matter in the brain, where conscious perception takes place
cerebrospinal fluid (CSF) circulatory medium within the CNS
corpus callosum fibre bundle which connects up the two cerebral hemispheres
dendrite one of many branchlike processes that extends from the neuron cell body and functions as a contact for incoming signals (synapses) from other neurons or sensory cells
excitable membrane cell membrane that regulates the movement of ions so that an electrical signal can be generated
frontal lobe area of cerebral cortex located at the front of the brain, control cognitive functions
ganglion localised collection of neuron cell bodies in the peripheral nervous system
gated property of a channel that determines how it opens under specific conditions, such as voltage change or physical deformation
glial cell one of the various types of neural tissue cells responsible for maintenance of the tissue, and largely responsible for supporting neurons
grey matter regions of the nervous system containing cell bodies of neurons with few or no myelinated axons; actually may be more pink or tan in colour, but called grey in contrast to white matter
integration nervous system function that combines sensory perceptions and higher cognitive functions (memories, learning, emotion, etc.) to produce a response
leak channel ion channel that opens randomly and is not gated to a specific event, also known as a non-gated channel
ligand-gated channel an ion channel that opens up after the binding of a ligand
mechanically gated channel ion channel that opens when a physical event directly affects the structure of the protein
membrane potential distribution of charge across the cell membrane, based on the charges of ions
meninges the three layers of protective covering of the central nervous system
motor neuron a neuron from the CNS or a ganglion that conducts a nerve impulse to a muscle that results in movement
myelin sheath lipid-rich layer of insulation that surrounds an axon, formed by oligodendrocytes in the CNS and Schwann cells in the PNS; facilitates the transmission of electrical signals
nerve cord-like bundle of axons located in the peripheral nervous system that transmits sensory input and response output to and from the central nervous system
neuron neural tissue cell that is primarily responsible for generating and propagating electrical signals into, within, and out of the nervous system
neurotransmission process by which one neuron communicates with another neuron
neurotransmitter chemical signal that is released from the synaptic end bulb of a neuron to cause a change in the target cell
occipital lobe part of the cerebral cortex, located at the back of the brain, involved in vision
parasympathetic system part of the autonomic system that allows an animal to “rest and digest”
parietal lobe part of the cerebral cortex located at the top of the brain, processes somatosensation
peripheral nervous system (PNS) anatomical division of the nervous system that is largely outside the cranial and vertebral cavities, namely all parts except the brain and spinal cord
presynaptic membrane part of axon terminal that forms a synapse with postsynaptic membrane of a dendrite or muscle
propagation movement of an action potential along the length of an axon
reception the first step in cell signaling when a signaling molecule binds to its receptor on the target cell’s membrane
response nervous system function that causes a target tissue (muscle or gland) to produce an event as a consequence to stimuli OR the final stage in cell signaling
resting membrane potential the difference in voltage measured across a cell membrane under steady-state conditions, typically -70 mV
sensation nervous system function that receives information from the environment and translates it into the electrical signals of nervous tissue
signal transduction pathway a set of chemical reactions triggered by the binding of a molecule such as a neurotransmitter or hormone to a receptor on the cell membrane
somatic nervous system (SNS) functional division of the nervous system that is concerned with conscious perception, voluntary movement, and skeletal muscle reflexes
spinal cord organ of the central nervous system found within the vertebral cavity and connected with the periphery through spinal nerves; mediates reflex behaviours
stimulus an event in the external or internal environment that registers as activity in a sensory neuron
sympathetic nervous system part of the autonomic system, which is responsible for the “fight-or-flight” response
synapse narrow junction across which a chemical signal passes from neuron to the next, initiating a new electrical signal in the target cell
synaptic cleft small gap between cells in a chemical synapse where neurotransmitter diffuses from the presynaptic element to the postsynaptic element
temporal lobe located at the base of the brain, processes and interprets sound
threshold membrane voltage at which an action potential is initiated
voltage gated channel responds to changes in voltage across the membrane it is embedded in
voltage-gated channel ion channel that opens because of a change in the charge distributed across the membrane where it is located
white matter regions of the nervous system containing mostly myelinated axons, making the tissue appear white because of the high lipid content of myelin
adrenal glands endocrine glands located at the top of each kidney that are important for the regulation of the stress response, blood pressure and blood volume, water homeostasis, and electrolyte levels
adrenaline primary and most potent catecholamine hormone secreted by the adrenal medulla in response to short term stress; also called epinephrine
aldosterone hormone produced and secreted by the adrenal cortex that stimulates sodium and fluid retention and increases blood volume and blood pressure
antidiuretic hormone (ADH) hypothalamic hormone that is stored by the posterior pituitary and that signals the kidneys to reabsorb water
cortisol glucocorticoid important in gluconeogenesis, the catabolism of glycogen, and downregulation of the immune system
diabetes mellitus condition caused by destruction or dysfunction of the beta cells of the pancreas or cellular resistance to insulin that results in abnormally high blood glucose levels
downregulation decrease in the number of hormone receptors, typically in response to chronically excessive levels of a hormone
endocrine gland tissue or organ that secretes hormones into the blood and lymph without ducts such that they may be transported to organs distant from the site of secretion
endocrine system cells, tissues, and organs that secrete hormones as a primary or secondary function and play an integral role in normal bodily processes
epinephrine primary and most potent catecholamine hormone secreted by the adrenal medulla in response to short term stress; also called adrenaline
Erythropoietin (EPO) released by kidneys in response to low oxygen levels and triggers the formation of red blood cells in the bone marrow.
exocrine system cells, tissues, and organs that secrete substances directly to target tissues via glandular ducts
glucagon pancreatic hormone that stimulates the catabolism of glycogen to glucose, thereby increasing blood glucose levels
goitre enlargement of the thyroid gland either as a result of iodine deficiency or hyperthyroidism
hormone secretion of an endocrine organ that travels via the bloodstream or lymphatics to induce a response in target cells or tissues in another part of the body
hormone receptor protein within a cell or on the cell membrane that binds a hormone, initiating the target cell response
hyperglycaemia abnormally high blood glucose levels
hypoglycaemia abnormally low blood glucose levels
hypothalamus–pituitary complex structural and functional connection between the hypothalamus and pituitary
insulin pancreatic hormone that enhances the cellular uptake and utilisation of glucose, thereby decreasing blood glucose levels
norepinephrine secondary catecholamine hormone secreted by the adrenal medulla in response to short-term stress; also called noradrenaline
pancreas organ with both exocrine and endocrine functions located posterior to the stomach that is important for digestion and the regulation of blood glucose
pancreatic islets specialised clusters of pancreatic cells that have endocrine functions; also called islets of Langerhans
pituitary gland bean-sized organ suspended from the hypothalamus that produces, stores, and secretes hormones in response to hypothalamic stimulation (also called hypophysis)
Thyroid stimulating hormone (TSH) hormone from the anterior pituitary gland that stimulates the thyroid gland
upregulation increase in the number of hormone receptors, typically in response to chronically reduced levels of a hormone
Review Questions
Chapter attribution
Content adapted from:
Anatomy and Physiology 2e (2022), by J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble and Peter DeSaix, is published by OpenStax https://openstax.org/details/books/anatomy-and-physiology-2e, and used under a CC BY licence.
Concepts of Biology (2013), by Samantha Fowler, Rebecca Roush and James Wise, is published by OpenStax https://openstax.org/details/books/concepts-biology, and used under a CC BY licence.
Microbiology (2016), by Nina Parker, Mark Schneegurt, Anh-Hue Thi Tu, Philip Lister and Brian M. Forster, is published by OpenStax https://openstax.org/details/books/microbiology, and used under a CC BY licence.
Media Attributions
- Figure 10.1 A nerve © Eleanor Smith, available under a Pixabay licence
- 1Signal_Transduction_Pathways_Model.svg © Yaneeporn is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 10.3 Central and peripheral nervous system © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.4 The lobes of the cerebral cortex © Charles Molnar & Jane Gair is licensed under a CC BY (Attribution) license
- Figure 10.5 Motor and sensory cortices © (Left) Rose M. Spielman, William J. Jenkins & Marilyn D. Lovett. (Right) J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix adapted by Vicki Dunk is licensed under a CC BY (Attribution) license
- Figure 10.6 Testing the water © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Imgnotraçat_arc_reflex_eng.svg © MartaAguayo is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 10.8 Knee jerk reflex © Helixitta is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 10.9 Autonomic nervous innervation © Geo-Science International is licensed under a CC0 (Creative Commons Zero) license
- Figure 10.10 Parts of a neuron © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.11 Cell membrane and transmembrane proteins © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.12 Measuring charge across a membrane © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.13 Ligand gated channels © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.14 Voltage gated channels © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.15 Propagation of an action potential © Laurentaylorj is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 10.16 The synapse © K. A. Young, J. A. Wise, P. DeSaix, D. H. Kruse, B. Poe, E. Johnson, J. E. Johnson, O. Korol, J. G. Betts, & M. Womble is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 10.17 Endocrine system © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.18 Hypothalamus-Pituitary Axis © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.19 A goitre © Almazi is licensed under a Public Domain license
- Figure 10.20 The adrenal gland © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix. Micrograph by University of Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 10.21 Anatomy of the pancreas © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix. Micrograph by University of Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 10.22 Homeostatic regulation of blood glucose levels © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 10.23 The thyroid system © Mikael Häggström is licensed under a Public Domain license

