9. Beating and breathing
- Describe the role of the airways, lungs and thoracic cavity in breathing
- Explain how pressure gradients, which drive gas movements in to and out of the bloodstream, are produced
- Explain how gas exchange in the lungs and tissue occurs
- Describe the role of the heart and blood vessels in circulation
- Explain what blood pressure is and how it can be varied.
9.1 | The respiratory system – How do we get gases in and out?

Let us now look at the reason we breathe – it is all to do with getting those gases into and out of the blood. Hold your breath. Really! See how long you can hold your breath as you continue reading…How long can you do it? Chances are you are feeling uncomfortable already. A typical human cannot survive without breathing for more than 3 minutes, and even if you wanted to hold your breath longer, your autonomic nervous system would take control. This is because every cell in the body needs to run the oxidative stages (the part that uses oxygen) of cellular respiration, the process by which energy is produced in the form of adenosine triphosphate (ATP). You may be surprised to learn that although oxygen is a critical need for cells, it is actually the accumulation of carbon dioxide that primarily drives your need to breathe. Carbon dioxide is exhaled, and oxygen is inhaled through the respiratory system, which includes muscles to move air into and out of the lungs, passageways through which air moves, and microscopic gas exchange surfaces covered by capillaries. The circulatory system transports gases from the lungs to tissues throughout the body and vice versa. A variety of diseases can affect the respiratory system, such as asthma, emphysema, chronic obstruction pulmonary disorder (COPD), and lung cancer. All of these conditions affect the gas exchange process and result in laboured breathing and other difficulties.
What is the function of the different zones of the respiratory system and how is it related to their structure?
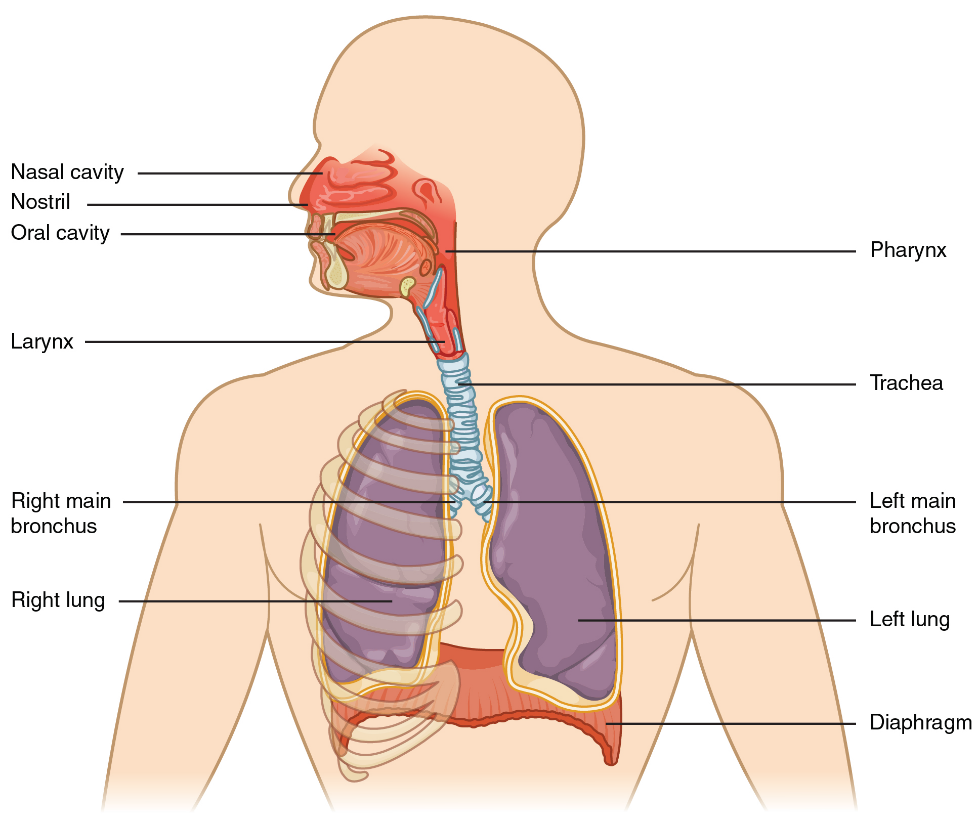
The air enters the body through the nasal cavity located just inside the nose (Figure 9.2). As the air passes through the nasal cavity, the air is warmed to body temperature and humidified by moisture from mucous membranes. These processes help equilibrate the air to the body conditions, reducing any damage that cold, dry air can cause. Particulate matter that is floating in the air is removed in the nasal passages by hairs, mucus, and cilia. Air is also chemically sampled by the sense of smell.
From the nasal cavity, air passes through the pharynx (throat) and the larynx (voice box) as it makes its way to the trachea (Figure 9.3). The main function of the trachea is to funnel the inhaled air to the lungs and the exhaled air back out of the body. The human trachea is a cylinder, about 25 to 30 cm long, which sits in front of the oesophagus and extends from the pharynx into the chest cavity to the lungs. It is made of incomplete rings of cartilage and smooth muscle. The cartilage provides strength and support to the trachea to keep the passage open. The trachea is lined with cells that have cilia and secrete mucus. The mucus catches particles that have been inhaled, and the cilia move the particles toward the pharynx.
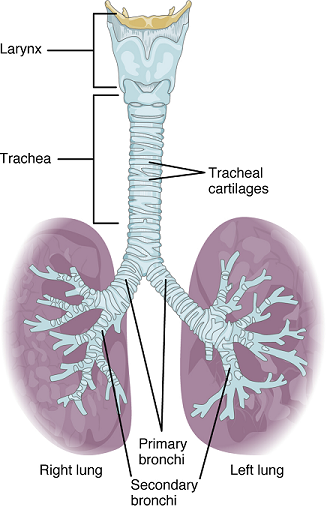
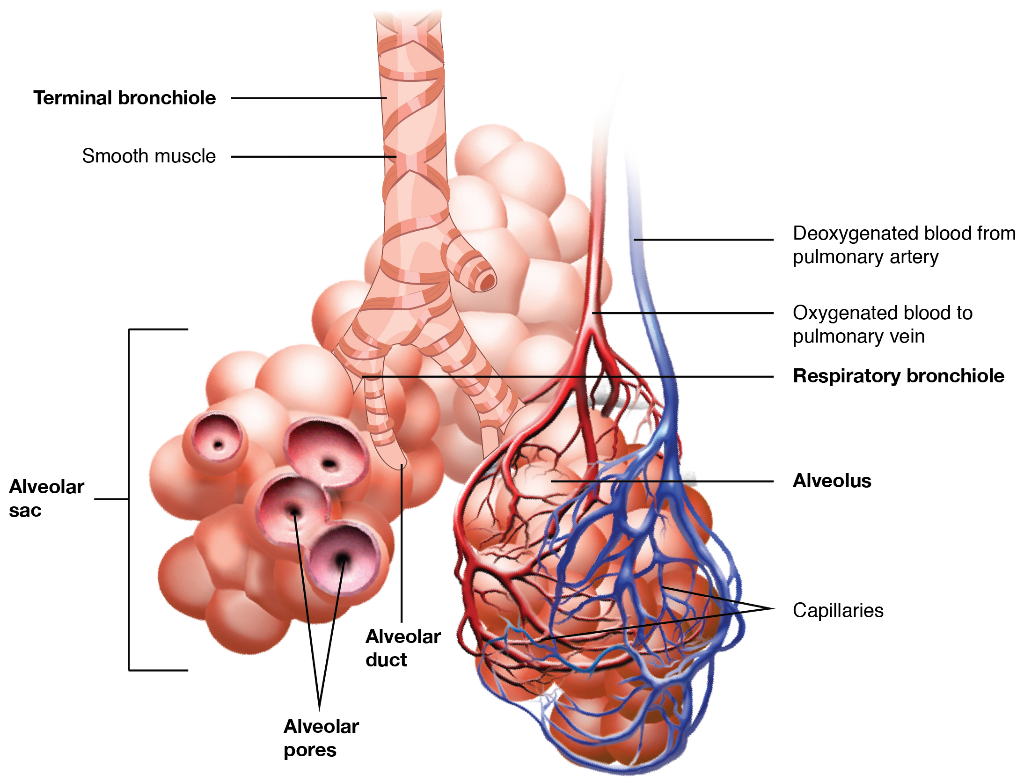
The end of the trachea divides into two bronchi that enter the right and left lung. Air enters the lungs through the primary bronchi. The primary bronchus divides, creating smaller and smaller diameter bronchi until the passages are under 1 mm in diameter when they are called bronchioles as they split and spread through the lung. Like the trachea, the bronchus and bronchioles are made of cartilage and smooth muscle. Bronchi are innervated by nerves of both the parasympathetic and sympathetic nervous systems that control muscle contraction (parasympathetic) or relaxation (sympathetic) in the bronchi and bronchioles, depending on the nervous system’s cues. The final bronchioles are the respiratory bronchioles. Alveolar ducts are attached to the end of each respiratory bronchiole. At the end of each duct are alveolar sacs, each containing 20 to 30 alveoli. Gas exchange occurs only in the alveoli. The alveoli are thin-walled and look like tiny bubbles within the sacs. The alveoli are in direct contact with capillaries of the circulatory system. Such intimate contact ensures that oxygen will diffuse from the alveoli into the blood. In addition, carbon dioxide will diffuse from the blood into the alveoli to be exhaled. The anatomical arrangement of capillaries and alveoli emphasises the structural and functional relationship of the respiratory and circulatory systems. Estimates for the surface area of alveoli in the lungs vary around 100 m2. This large area is about the area of half a tennis court. This large surface area, combined with the thin-walled nature of the alveolar cells, allows gases to easily diffuse across the cells.
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange. The gas exchange occurs in the respiratory zone.
Conducting zone
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. The conducting zone is made of all structures from the nose down to the terminal bronchioles (Figures 9.3 and 9.4). Included in this zone are the:
- nose
- pharynx
- larynx
- trachea
- bronchial tree
Respiratory zone
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole (Figure 9.5), which then leads to an alveolar duct, opening into a cluster of alveoli.
Alveoli
An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli (Figure 9.6). An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
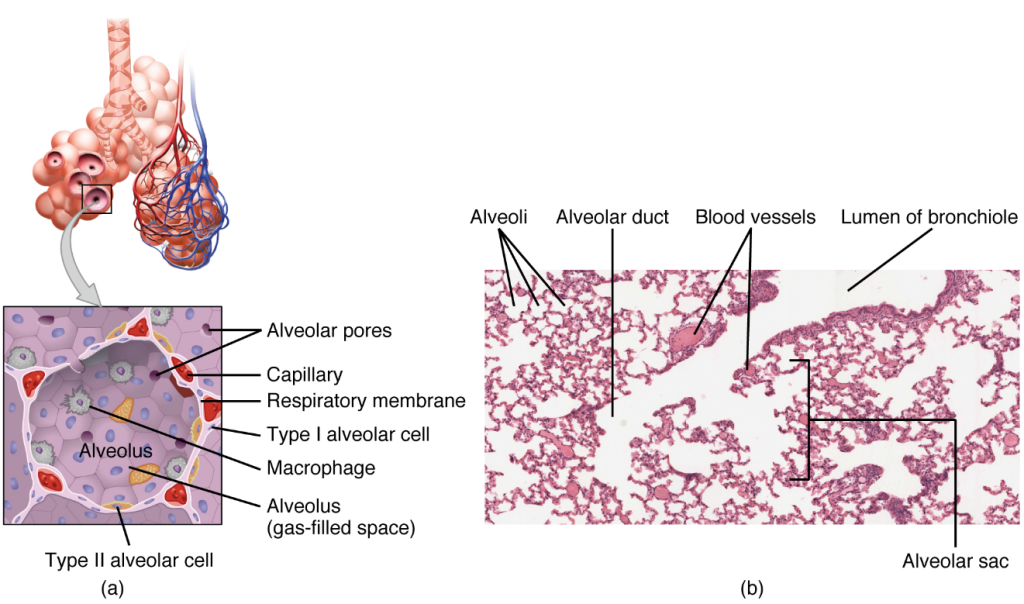
The alveolar epithelium is extremely thin and borders the endothelial membrane of capillaries. Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0.5 mm thick. The respiratory membrane allows gases to cross by simple diffusion, allowing oxygen to be picked up by the blood for transport and carbon dioxide to be released into the air of the alveoli.
Compare and contrast the respiratory and conducting zones. What is unique about each one, what is similar in both? How is the structure of each related to the function it performs?
What is the structure of the lungs?
A major organ of the respiratory system, each lung houses structures of both the conducting and respiratory zones. The main function of the lungs is to perform the exchange of oxygen and carbon dioxide with air from the atmosphere. To this end, the lungs exchange respiratory gases across a very large epithelial surface area—about 70 square meters—that is highly permeable to gases.
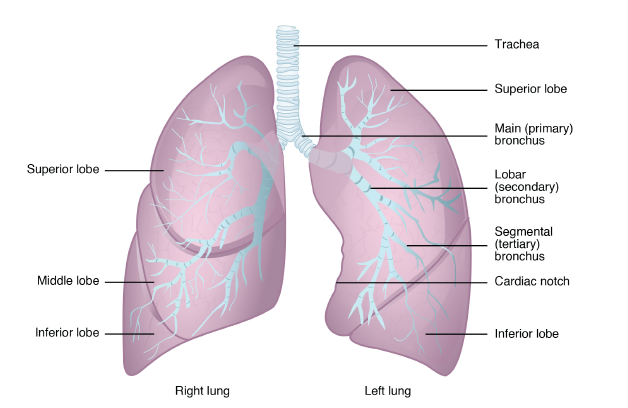
Gross Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi (Figure 9.7); on the inferior surface, the lungs are bordered by the diaphragm. The diaphragm is the flat, dome-shaped muscle located at the base of the lungs and thoracic cavity. Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right consists of three lobes: the superior, middle and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes.
Pleura of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The pleurae consist of two layers. The visceral pleura is the layer that is superficial to the lungs and extends into and lines the lung fissures (Figure 9.8). In contrast, the parietal pleura is the outer layer that connects to the thoracic wall. The pleural cavity is the space between the visceral and parietal layers.
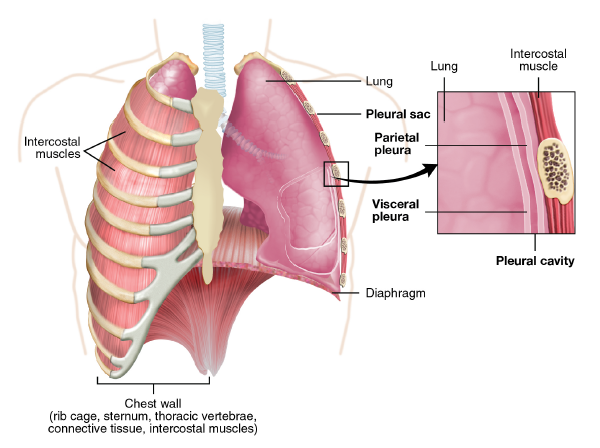
The pleurae produce pleural fluid which acts to lubricate the lung surfaces. This lubrication reduces friction between the two layers to prevent trauma during breathing and creates surface tension that helps maintain the position of the lungs against the thoracic wall. This adhesive characteristic of the pleural fluid causes the lungs to enlarge when the thoracic wall expands during ventilation, allowing the lungs to fill with air.
What causes the air to move in and out of the lungs?
Pulmonary ventilation is the act of breathing, which can be described as the movement of air into and out of the lungs. The major mechanisms that drive pulmonary ventilation are atmospheric pressure (Patm); the air pressure within the alveoli, called alveolar pressure (Palv); and the pressure within the pleural cavity, called intrapleural pressure (Pip).
Mechanisms of breathing
Inspiration (or inhalation) and expiration (or exhalation) are dependent on the differences in pressure between the atmosphere and the lungs. Differences in pressure cause a pressure gradient and gases will move from the area of high pressure to the area of low pressure.
Pressure relationships
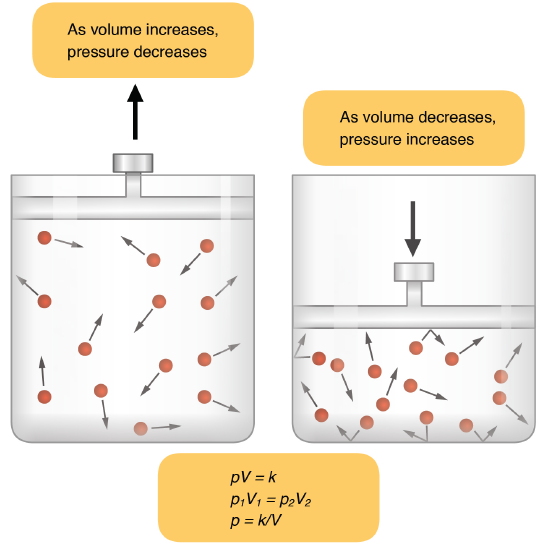
In a gas, pressure is a force created by the movement of gas molecules that are confined. For example, a certain number of gas molecules in a two-litre container has more room to move than the same number of gas molecules in a one-litre container (Figure 9.15). In this case, the force exerted by the movement of the gas molecules against the walls of the two-litre container is lower than the force exerted by the gas molecules in the one-litre container. Therefore, the pressure is lower in the two-litre container and higher in the one-litre container. At a constant temperature, changing the volume occupied by the gas changes the pressure. Boyle’s law describes the relationship between volume and pressure in a gas at a constant temperature. Boyle discovered that the pressure of a gas is inversely proportional to its volume: If volume increases, then pressure decreases. Likewise, if volume decreases, pressure increases. Boyle’s law is expressed by the following formula:
P1V1 = P2V2
An example:
2 litre container at 2 atm = 1 litre container at X atm
Solving for X gives us 4 atm
Therefore, the 1 litre container has a pressure of 4 atmospheres
In this formula, P1 represents the initial pressure and V1 represents the initial volume, whereas the final pressure and volume are represented by P2 and V2, respectively. In Figure 9.9, if the two- and one-litre containers were connected by a tube and the volume of one of the containers were changed, then the gases would move from higher pressure (lower volume) to lower pressure (higher volume).
Boyle’s Law, explained in relation to the respiratory system, is demonstrated in this video by Primal Pictures 3D Human Anatomy.
As previously mentioned, pulmonary ventilation is dependent on three types of pressure: atmospheric, intra-alveolar, and intrapleural. Atmospheric pressure is the amount of force that is exerted by gases in the air surrounding any given surface, such as the body. Atmospheric pressure can be expressed in terms of the unit atmosphere, abbreviated atm, or in millimetres of mercury (mm Hg). One atm is equal to 760 mm Hg, which is the atmospheric pressure at sea level. Typically, for respiration, other pressure values are discussed in relation to atmospheric pressure. Therefore, negative pressure is pressure lower than the atmospheric pressure, whereas positive pressure is pressure that it is greater than the atmospheric pressure. A pressure that is equal to the atmospheric pressure is expressed as zero.
Intra-alveolar pressure is the pressure of the air within the alveoli, which changes during the different phases of breathing (Figure 9.10). Because the alveoli are connected to the atmosphere via the tubing of the airways (similar to the two- and one-litre containers in the example above), the intrapulmonary pressure of the alveoli always equalises with the atmospheric pressure. Thus, air will move into or out of the alveoli.
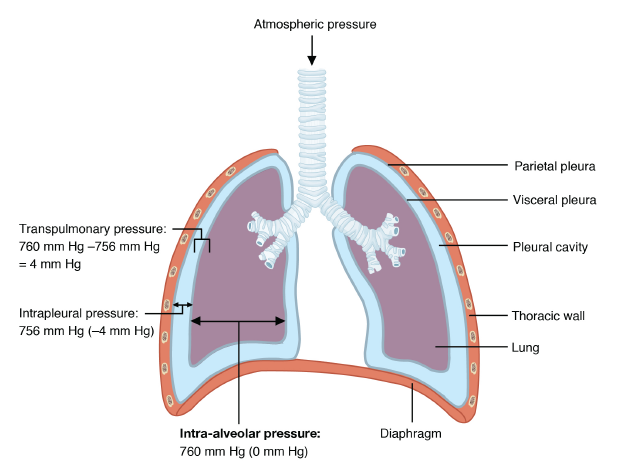
Intrapleural pressure is the pressure of the air within the pleural cavity, between the visceral and parietal pleurae. Similar to intra-alveolar pressure, intrapleural pressure also changes during the different phases of breathing. However, due to certain characteristics of the lungs, the intrapleural pressure is always lower than, or negative to, the intra-alveolar pressure (and therefore also to atmospheric pressure). Although it fluctuates during inspiration and expiration, intrapleural pressure remains approximately –4 mm Hg throughout the breathing cycle.
Physical factors affecting ventilation
In addition to the differences in pressures, breathing is also dependent upon the contraction and relaxation of muscle fibres of both the diaphragm and thorax. The lungs themselves are passive during breathing, meaning they are not involved in creating the movement that helps inspiration and expiration. This is because of the adhesive nature of the pleural fluid, which allows the lungs to be pulled outward when the thoracic wall moves during inspiration. The recoil of the thoracic wall during expiration causes compression of the lungs. Contraction and relaxation of the diaphragm and intercostals muscles (found between the ribs) cause most of the pressure changes that result in inspiration and expiration. These muscle movements and subsequent pressure changes cause air to either rush in or be forced out of the lungs.
Pulmonary ventilation
The difference in pressures drives pulmonary ventilation because air flows down a pressure gradient, that is, air flows from an area of higher pressure to an area of lower pressure. Air flows into the lungs largely due to a difference in pressure; atmospheric pressure is greater than intra-alveolar pressure, and intra-alveolar pressure is greater than intrapleural pressure. Air flows out of the lungs during expiration based on the same principle; pressure within the lungs becomes greater than the atmospheric pressure.
Pulmonary ventilation comprises two major steps: inspiration and expiration. Inspiration is the process that causes air to enter the lungs, and expiration is the process that causes air to leave the lungs (Figure 9.11). A respiratory cycle is one sequence of inspiration and expiration. In general, two muscle groups are used during normal inspiration: the diaphragm and the external intercostal muscles. Additional muscles can be used if a bigger breath is required. When the diaphragm contracts, it moves inferiorly toward the abdominal cavity, creating a larger thoracic cavity and more space for the lungs. Contraction of the external intercostal muscles moves the ribs upward and outward, causing the rib cage to expand, which increases the volume of the thoracic cavity. Due to the adhesive force of the pleural fluid, the expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in intra-alveolar pressure, creating a pressure lower than atmospheric pressure. As a result, a pressure gradient is created that drives air into the lungs.
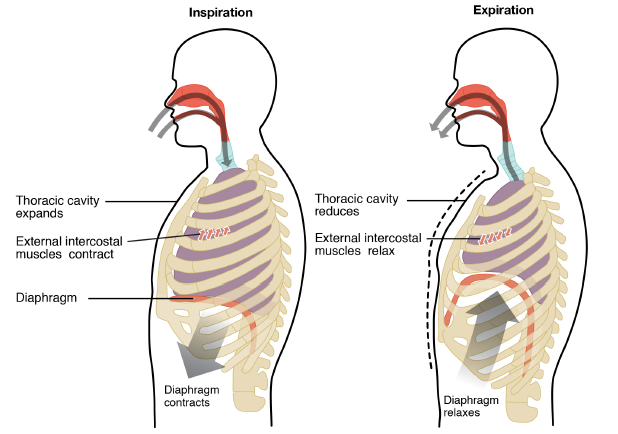
The process of normal expiration is passive, meaning that energy is not required to push air out of the lungs. Instead, the elasticity of the lung tissue causes the lung to recoil, as the diaphragm and intercostal muscles relax following inspiration. In turn, the thoracic cavity and lungs decrease in volume, causing an increase in intrapulmonary pressure. The intrapulmonary pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
ACTIVITY: Make a summary of this information by copying and completing the following table
| INHALATION | EXHALATION | |
| Diaphragm | ||
| Ribs | ||
| Volume | ||
| Pressure | ||
| Air movement |
How do oxygen and carbon dioxide move between the blood and the cells?
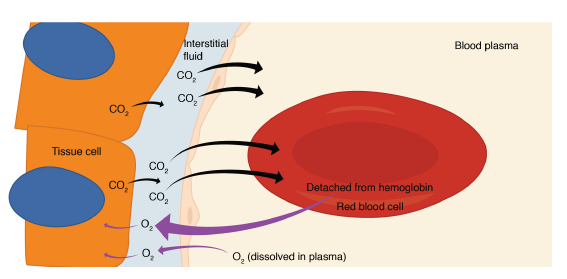
Gas exchange occurs at two sites in the body: in the lungs, where oxygen is picked up and carbon dioxide is released at the respiratory membrane, and at the tissues, where oxygen is released, and carbon dioxide is picked up. External respiration is the exchange of gases with the external environment and occurs in the alveoli of the lungs. Internal respiration is the exchange of gases with the internal environment and occurs in the tissues. The actual exchange of gases occurs due to simple diffusion. Energy is not required to move oxygen or carbon dioxide across membranes. Instead, these gases follow pressure gradients that allow them to diffuse. The anatomy of the lung maximises the diffusion of gases: The respiratory membrane is highly permeable to gases; the respiratory and blood capillary membranes are very thin; and there is a large surface area throughout the lungs.
External Respiration: The pulmonary artery carries deoxygenated blood into the lungs from the heart, where it branches and eventually becomes the capillary network composed of pulmonary capillaries. These pulmonary capillaries create the respiratory membrane with the alveoli. As the blood is pumped through this capillary network, gas exchange occurs. Although a small amount of the oxygen is able to dissolve directly into plasma from the alveoli, most of the oxygen is picked up by erythrocytes (red blood cells) and binds to a protein called haemoglobin. Oxygenated haemoglobin is red, causing the overall appearance of bright red oxygenated blood, which returns to the heart through the pulmonary veins. Carbon dioxide is released in the opposite direction of oxygen, from the blood to the alveoli.
Internal respiration is gas exchange that occurs at the level of body tissues (Figure 9.12). Similar to external respiration, internal respiration also occurs as simple diffusion due to a partial pressure gradient. However, the partial pressure gradients are opposite of those present at the respiratory membrane. The partial pressure of oxygen in tissues is low, about 40 mm Hg, because oxygen is continuously used for cellular respiration. In contrast, the partial pressure of oxygen in the blood is about 100 mm Hg. This creates a pressure gradient that causes oxygen to dissociate from haemoglobin, diffuse out of the blood, cross the interstitial space, and enter the tissue. Haemoglobin that has little oxygen bound to it loses much of its brightness, so that blood returning to the heart is more burgundy in colour.
Considering that cellular respiration continuously produces carbon dioxide, the partial pressure of carbon dioxide is lower in the blood than it is in the tissue, causing carbon dioxide to diffuse out of the tissue, cross the interstitial fluid, and enter the blood. It is then carried back to the lungs either bound to haemoglobin, dissolved in plasma, or in a converted form.
How is the respiratory rate controlled?
Breathing usually occurs without thought, although at times you can consciously control it, such as when you swim under water, sing a song, or blow bubbles. The respiratory rate is the total number of breaths, or respiratory cycles, that occur each minute. Respiratory rate can be an important indicator of disease, as the rate may increase or decrease during an illness or in a disease condition. The respiratory rate is controlled by the respiratory centre located within the medulla oblongata in the brain, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood. The normal respiratory rate of a child decreases from birth to adolescence. A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute, but by the time a child is about 10 years old, the normal rate is closer to 18 to 30. By adolescence, the normal respiratory rate is similar to that of adults, 12 to 18 breaths per minute.
How are oxygen and carbon dioxide carried in the blood?
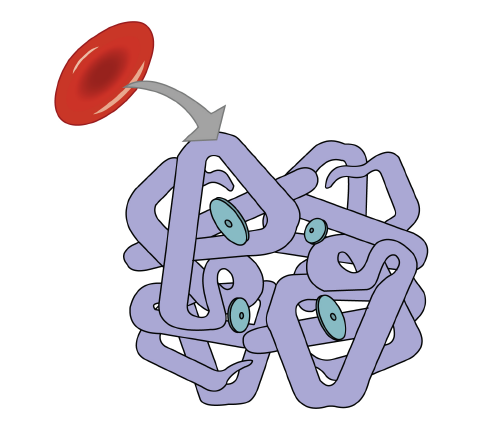
Oxygen transport in the blood
Even though oxygen is transported via the blood, you may recall that oxygen is not very soluble in liquids. A small amount of oxygen does dissolve in the blood and is transported in the bloodstream, but it is only about 1.5% of the total amount. The majority of oxygen molecules are carried from the lungs to the body’s tissues by a specialised transport system, which relies on the erythrocyte—the red blood cell. Erythrocytes contain a metalloprotein, haemoglobin, which serves to bind oxygen molecules to the erythrocyte (Figure 9.13). Heme is the portion of haemoglobin that contains iron, and it is heme that binds oxygen. One erythrocyte contains four iron ions, and because of this, each erythrocyte is capable of carrying up to four molecules of oxygen. As oxygen diffuses across the respiratory membrane from the alveolus to the capillary, it also diffuses into the red blood cell and is bound by haemoglobin. The following reversible chemical reaction describes the production of the final product, oxyhaemoglobin (Hb–O2), which is formed when oxygen binds to haemoglobin. Oxyhemoglobin is a bright red-coloured molecule that contributes to the bright red colour of oxygenated blood.
Hb + O2 ↔ Hb − O2
In this formula, Hb represents reduced haemoglobin, that is, haemoglobin that does not have oxygen bound to it. There are multiple factors involved in how readily heme binds to and dissociates from oxygen.
Carbon dioxide transport in the blood
Carbon dioxide is transported by three major mechanisms. The first mechanism of carbon dioxide transport is by blood plasma, as some carbon dioxide molecules dissolve in the blood. The second mechanism is transport in the form of bicarbonate (HCO3 –), which also dissolves in plasma. The third mechanism of carbon dioxide transport is similar to the transport of oxygen by erythrocytes (Figure 9.14).
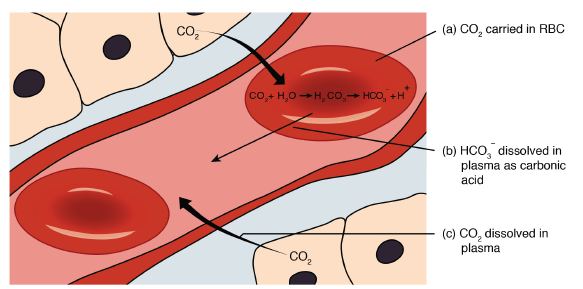
Dissolved carbon dioxide
Although carbon dioxide is not considered to be highly soluble in blood, a small fraction—about 7 to 10 percent—of the carbon dioxide that diffuses into the blood from the tissues dissolves in plasma. The dissolved carbon dioxide then travels in the bloodstream and when the blood reaches the pulmonary capillaries, the dissolved carbon dioxide diffuses across the respiratory membrane into the alveoli, where it is then exhaled during pulmonary ventilation.
Bicarbonate buffer
A large fraction—about 70 percent—of the carbon dioxide molecules that diffuse into the blood is transported to the lungs as bicarbonate. Most bicarbonate is produced in erythrocytes after carbon dioxide diffuses into the capillaries, and subsequently into red blood cells. Carbonic anhydrase (CA) causes carbon dioxide and water to form carbonic acid (H2CO3), which dissociates into two ions: bicarbonate (HCO3 –) and hydrogen (H+). The following formula depicts this reaction:
At the pulmonary capillaries, the chemical reaction that produced bicarbonate (shown above) is reversed, and carbon dioxide and water are the products. Much of the bicarbonate in the plasma re-enters the erythrocytes in exchange for chloride ions. Hydrogen ions and bicarbonate ions join to form carbonic acid, which is converted into carbon dioxide and water by carbonic anhydrase. Carbon dioxide diffuses out of the erythrocytes and into the plasma, where it can further diffuse across the respiratory membrane into the alveoli to be exhaled during pulmonary ventilation.
Carbaminohaemoglobin
About 20 percent of carbon dioxide is bound by haemoglobin and is transported to the lungs. Carbon dioxide does not bind to iron as oxygen does; instead, carbon dioxide binds amino acid moieties on the globin portions of haemoglobin to form carbaminohaemoglobin, which forms when haemoglobin and carbon dioxide bind. When haemoglobin is not transporting oxygen, it tends to have a bluish-purple tone to it, creating the darker maroon colour typical of deoxygenated blood. The following formula depicts this reversible reaction:
CO2 + Hb ↔ HbCO2
Watch this video [3:08] to see the transport of oxygen from the lungs to the tissues. Why is oxygenated blood bright red, whereas deoxygenated blood tends to be more of a purple colour?
Respiratory system: Asthma
Asthma is a common condition that affects the lungs in both adults and children. Approximately 8.2 percent of adults (18.7 million) and 9.4 percent of children (7 million) in the United States suffer from asthma. In addition, asthma is the most frequent cause of hospitalisation in children. Asthma is a chronic disease characterised by inflammation and oedema of the airway, and bronchospasms (that is, constriction of the bronchioles), which can inhibit air from entering the lungs. In addition, excessive mucus secretion can occur, which further contributes to airway occlusion (Figure 9.15). Cells of the immune system, such as eosinophils and mononuclear cells, may also be involved in infiltrating the walls of the bronchi and bronchioles. Bronchospasms occur periodically and lead to an “asthma attack.” An attack may be triggered by environmental factors such as dust, pollen, pet hair, or dander, changes in the weather, mould, tobacco smoke, and respiratory infections, or by exercise and stress.
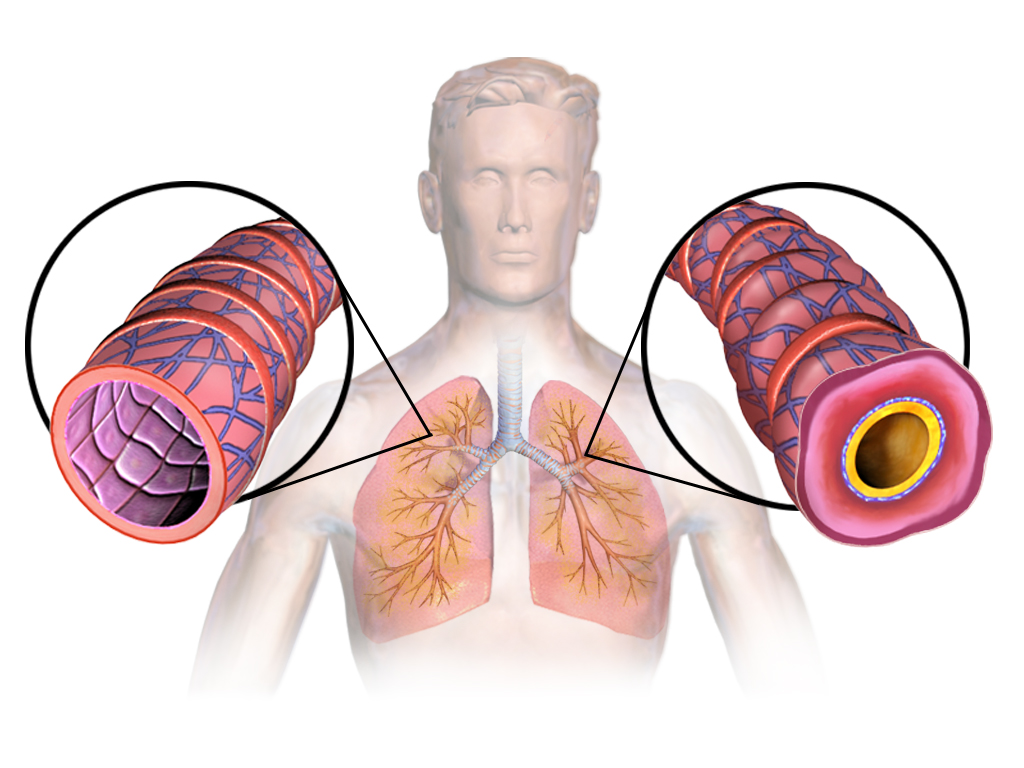
Symptoms of an asthma attack involve coughing, shortness of breath, wheezing, and tightness of the chest. Symptoms of a severe asthma attack that requires immediate medical attention would include difficulty breathing that results in blue (cyanotic) lips or face, confusion, drowsiness, a rapid pulse, sweating, and severe anxiety. The severity of the condition, frequency of attacks, and identified triggers influence the type of medication that an individual may require. Longer-term treatments are used for those with more severe asthma. Short-term, fast-acting drugs that are used to treat an asthma attack are typically administered via an inhaler. For young children or individuals who have difficulty using an inhaler, asthma medications can be administered via a nebuliser.
In many cases, the underlying cause of the condition is unknown. However, recent research has demonstrated that certain viruses, such as human rhinovirus C (HRVC), and the bacteria Mycoplasma pneumoniae and Chlamydia pneumoniae that are contracted in infancy or early childhood, may contribute to the development of many cases of asthma.
Watch the video [1:01] to learn more about what happens during an asthma attack.
9.2| The circulatory system – How do we get nutrients, gases and wastes to and from the cells?
What is the structure and function of the heart?
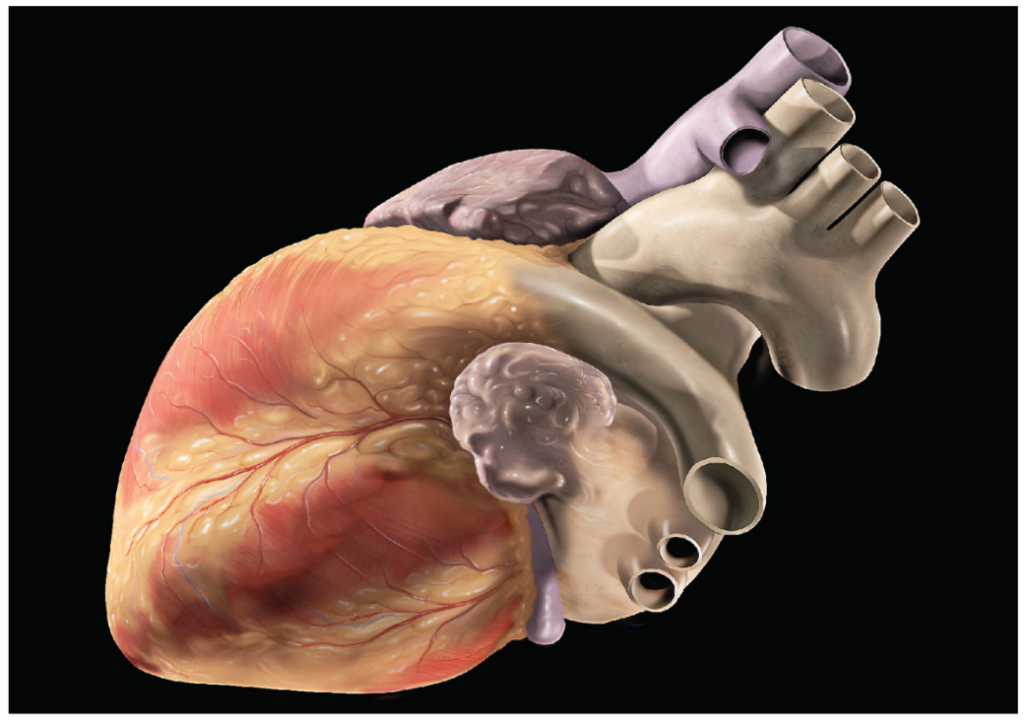
In this section, you will explore the remarkable pump that propels the blood into the vessels. There is no single better word to describe the function of the heart other than pump, since its contraction develops the pressure that ejects blood into the major vessels: the aorta and pulmonary trunk. From these vessels, the blood is distributed to the remainder of the body. Although the connotation of the term pump suggests a mechanical device made of steel and plastic, the anatomical structure is a living, sophisticated muscle. As you read this section try to keep these twin concepts in mind: pump and muscle.
The vital importance of the heart is obvious. If one assumes an average rate of contraction of 75 contractions per minute, a human heart will contract approximately 108,000 times in one day, more than 39 million times in one year, and nearly 3 billion times during a 75-year lifespan. Each of the major pumping chambers of the heart ejects approximately 70 mL blood per contraction in a resting adult. This would be equal to 5.25 litres of fluid per minute and approximately 14,000 litres per day. Over one year, that would equal 10,000,000 litres of blood sent through roughly 95, 000km of vessels. In order to understand how that happens, it is necessary to understand the anatomy and physiology of the heart.
Location of the heart
The human heart is located within the thoracic cavity, medially between the lungs in the space known as the mediastinum. Figure 9.17 shows the position of the heart within the thoracic cavity. Within the mediastinum, the heart is separated from the other mediastinal structures by a tough membrane known as the pericardium, or pericardial sac, and sits in its own space called the pericardial cavity. It is important to remember the position and orientation of the heart when placing a stethoscope on the chest of a patient and listening for heart sounds, and also when looking at images taken from a mid-sagittal perspective. The slight deviation of the apex to the left is reflected in a depression in the medial surface of the inferior lobe of the left lung, called the cardiac notch.
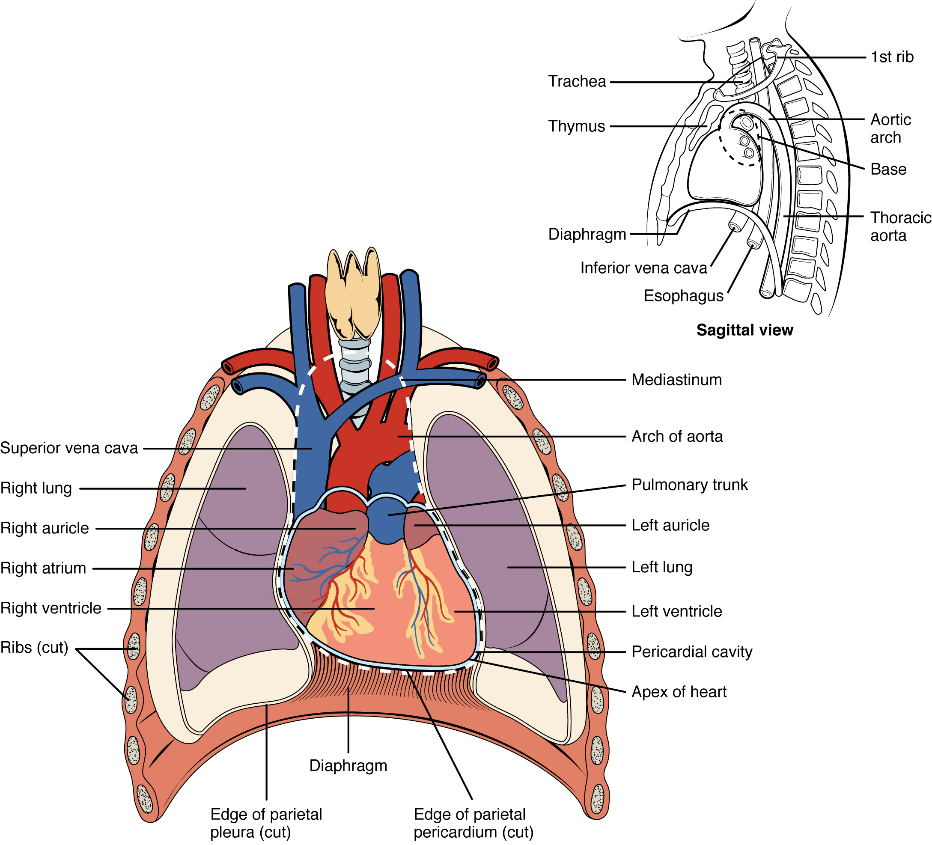
Shape and size of the heart
The shape of the heart is similar to a pinecone, rather broad at the superior surface and tapering to the apex (see Figure 9.17). A typical heart is approximately the size of your fist: 12 cm (5 in) in length, 8 cm (3.5 in) wide, and 6 cm (2.5 in) in thickness. Given the size difference between most members of the sexes, the weight of a female heart is approximately 250–300 grams (9 to 11 ounces), and the weight of a male heart is approximately 300–350 grams (11 to 12 ounces). The heart of a well-trained athlete, especially one specialising in aerobic sports, can be considerably larger than this. Cardiac muscle responds to exercise in a manner similar to that of skeletal muscle. That is, exercise results in the addition of protein myofilaments that increase the size of the individual cells without increasing their numbers, a concept called hypertrophy. Hearts of athletes can pump blood more effectively at lower rates than those of non-athletes. Enlarged hearts are not always a result of exercise; they can result from pathologies, such as hypertrophic cardiomyopathy. The cause of an abnormally enlarged heart muscle is unknown, but the condition is often undiagnosed and can cause sudden death in apparently otherwise healthy young people.
Chambers and circulation through the heart
The human heart consists of four chambers: The left side and the right side each have one atrium and one ventricle (Figure 9.18). Each of the upper chambers, the right atrium (plural = atria) and the left atrium, acts as a receiving chamber and contracts to push blood into the lower chambers, the right ventricle and the left ventricle. The ventricles serve as the primary pumping chambers of the heart, propelling blood to the lungs or to the rest of the body.
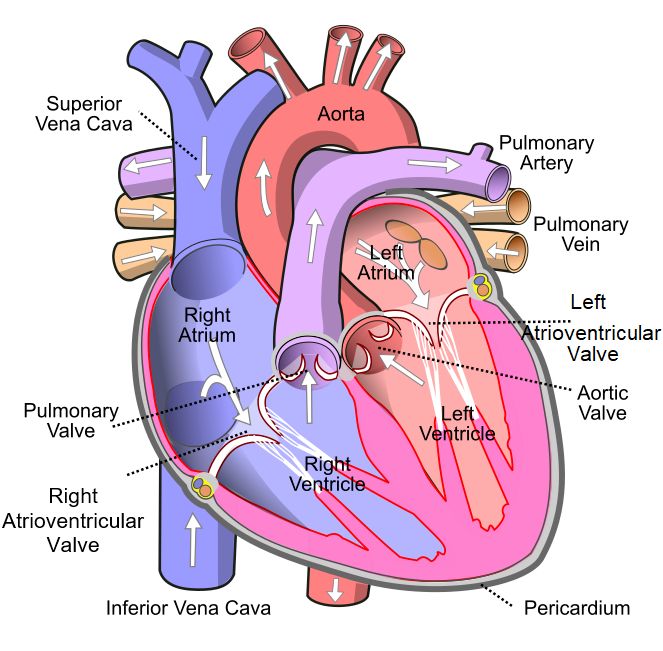
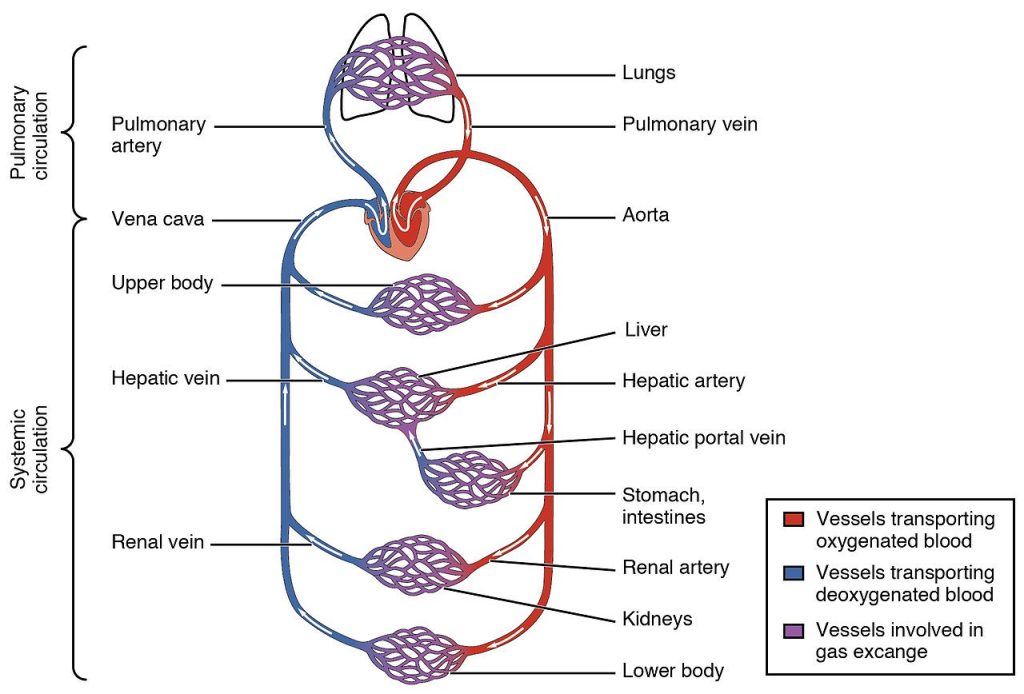
There are two distinct but linked circuits in the human circulation called the pulmonary and systemic circuits (Figure 9.19). Although both circuits transport blood and everything it carries, we can initially view the circuits from the point of view of gases.
The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation. The systemic circuit transports oxygenated blood to virtually all of the tissues of the body and returns relatively deoxygenated blood and carbon dioxide to the heart to be sent back to the pulmonary circulation.
The right ventricle pumps deoxygenated blood into the pulmonary trunk, which leads toward the lungs and bifurcates into the left and right pulmonary arteries. These vessels in turn branch many times before reaching the pulmonary capillaries, where gas exchange occurs: Carbon dioxide exits the blood and oxygen enters. The pulmonary trunk arteries and their branches are the only arteries that carry relatively deoxygenated blood. Highly oxygenated blood returning from the pulmonary capillaries in the lungs passes through a series of vessels that join together to form the pulmonary veins—the only veins that carry highly oxygenated blood. The pulmonary veins conduct blood into the left atrium, which pumps the blood into the left ventricle, which in turn pumps oxygenated blood into the aorta and on to the many branches of the systemic circuit. Eventually, these vessels will lead to the systemic capillaries, where exchange with the tissue fluid and cells of the body occurs. In this case, oxygen and nutrients exit the systemic capillaries to be used by the cells in their metabolic processes, and carbon dioxide and waste products will enter the blood.
The blood exiting the systemic capillaries is lower in oxygen concentration than when it entered. The capillaries will ultimately unite to form venules, joining to form ever-larger veins, eventually flowing into the two major systemic veins, the superior vena cava and the inferior vena cava, which return blood to the right atrium. The blood in the superior and inferior venae cava flows into the right atrium, which pumps blood into the right ventricle. This process of blood circulation continues as long as the individual remains alive. Understanding the flow of blood through the pulmonary and systemic circuits is critical to all health professions (Figure 9.20).
How does the blood get around the body?

In this section, you will learn about the vascular part of the cardiovascular system, that is, the vessels that transport blood throughout the body and provide the physical site where gases, nutrients, and other substances are exchanged with body cells. When vessel functioning is reduced, blood-borne substances do not circulate effectively throughout the body. As a result, tissue injury occurs, metabolism is impaired, and the functions of every bodily system are threatened.
Blood is carried through the body via blood vessels. An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels. Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart. Figure 9.21 shows a comparison of the size and structure of these different vessels.
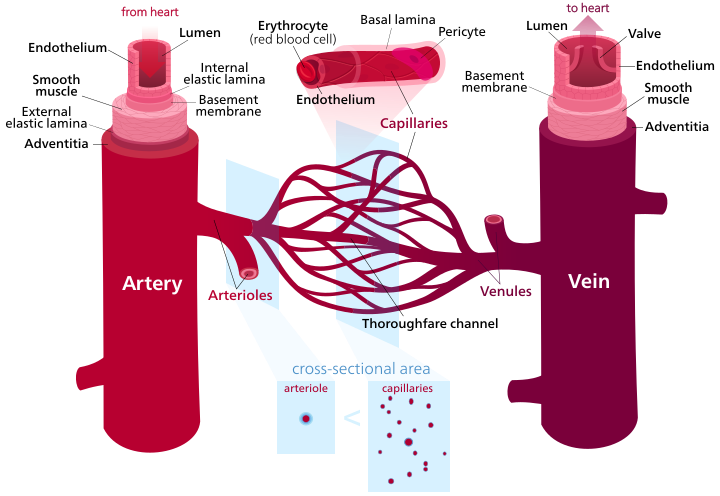
Structure and function of vessels
Different types of blood vessels vary slightly in their structures, but they share the same general features. Arteries and arterioles have thicker walls than veins and venules because they are closer to the heart and receive blood that is surging at a far greater pressure (Figure 9.6). Each type of vessel has a lumen—a hollow passageway through which blood flows. Arteries have smaller lumens than veins, a characteristic that helps to maintain the pressure of blood moving through the system. Together, their thicker walls and smaller diameters give arterial lumens a more rounded appearance in cross-section than the lumens of veins.
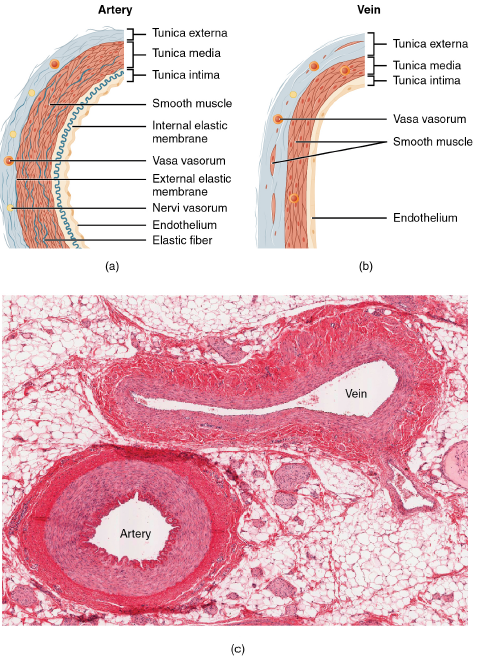
By the time blood has passed through capillaries and entered venules, the pressure initially exerted upon it by heart contractions has diminished. In other words, in comparison to arteries, venules and veins withstand a much lower pressure from the blood that flows through them. Their walls are considerably thinner, and their lumens are correspondingly larger in diameter, allowing more blood to flow with less vessel resistance. In addition, many veins of the body, particularly those of the limbs, contain valves that assist the unidirectional flow of blood toward the heart. This is critical because blood flow becomes sluggish in the extremities, as a result of the lower pressure and the effects of gravity.
Both arteries and veins have the same three distinct tissue layers, called tunics (from the Latin term tunica). From the most interior layer to the outer, these tunics are the tunica intima, the tunica media, and the tunica externa (see Figure 9.22).
ACTIVITY: Make a summary of this information by copying and completing the following table
| Characteristic | Arteries | Veins | Capillaries |
| Wall thickness | |||
| Permeability | |||
| Lumen | |||
| Valves | |||
| Pressure | |||
| Muscle and Elastic Fibres | |||
| Function |
Blood flow through the heart Crossword Puzzle
What is blood pressure?
The flow of blood through the blood vessels causes pressure to be exerted on the walls of the blood vessels – this is what we measure as blood pressure. Blood pressure varies depending on activity and the tissue’s demand for blood supply. A number of homeostatic mechanisms alter the diameter of the blood vessels or change heart rate to alter blood pressure to meet demand and return to normal levels.
Blood pressure may be measured in capillaries and veins, as well as the vessels of the pulmonary circulation; however, the term blood pressure without any specific descriptors typically refers to systemic arterial blood pressure—that is, the pressure of blood flowing in the arteries of the systemic circulation. In clinical practice, this pressure is measured in mm Hg and is usually obtained using the brachial artery of the arm.
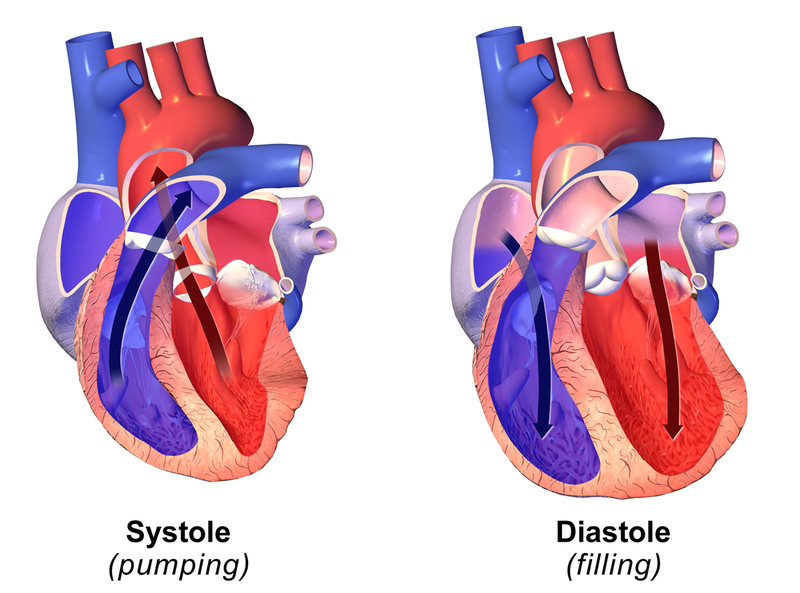
When systemic arterial blood pressure is measured, it is recorded as a ratio of two numbers (e.g., 120/80 is a normal adult blood pressure), expressed as systolic pressure over diastolic pressure. The systolic pressure is the higher value (typically around 120 mm Hg) and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole. The diastolic pressure is the lower value (usually about 80 mm Hg) and represents the arterial pressure of blood during ventricular relaxation, or diastole. The actions of the heart at each of these times is shown in Figure 9.23
Blood pressure must be great enough to enable blood to reach all of the body tissues, and yet low enough to ensure that the delicate blood vessels can withstand the friction and force of the blood against the vessel walls.
How is blood pressure regulated?
In order to maintain homeostasis in the cardiovascular system and provide adequate blood to the tissues, blood flow must be redirected continually to the tissues as they become more active. In a very real sense, the cardiovascular system engages in resource allocation, because there is not enough blood flow to distribute blood equally to all tissues simultaneously. For example, when an individual is exercising, more blood will be directed to skeletal muscles, the heart, and the lungs. Following a meal, more blood is directed to the digestive system. Only the brain receives a more or less constant supply of blood whether you are active, resting, thinking, or engaged in any other activity.
Blood pressure is maintained via negative feedback loops. The cardiovascular centres in the medulla oblongata respond to changes in blood pressure, as well as blood concentrations of oxygen, carbon dioxide and hydrogen ions. Blood pressure can be regulated over the short term or over a longer term. An example of short-term blood pressure regulation is the baroreceptor reflex. Baroreceptor is the general term for a receptor that detects changes in pressure. In the blood pressure baroreceptor reflex, they are stretch receptors located within the aortic and carotid sinuses and in the venae cava and right atrium.
When blood pressure increases or decreases the signal sent from the baroreceptors to the cardiovascular centres changes and triggers a reflex that maintains homeostasis.
For this short-term control of blood pressure there are two main effectors that can be varied quickly: the heart (via increased/decreased heart rate or increased/decreased force of contraction) or the vessels (via vasoconstriction or vasodilation).
An increase in heart rate or force of contraction will cause greater pressure on the vessel walls which will lead to an increase in blood pressure. A decrease in either will reduce the pressure on the vessel walls and lead to a decrease in blood pressure. Similarly, vasoconstriction causes the vessel diameter to decrease, which will increase the pressure; and vasodilation causes the vessel diameter to increase, which will lower the pressure.
An example of the baroreceptor reflex happening quickly is when you rise quickly after having been lying down. If you’ve done this, you may have experienced a moment of light headedness on standing, this is called orthostatic hypotension (hypo=below, tension=pressure – you can probably guess that high blood pressure is called hypertension). The sudden change in body position can mean that gravity can cause blood pressure to fall. The baroreceptor reflex is rapidly activated to restore your blood pressure.
Blood volume and blood viscosity also affect blood pressure. These are usually longer-term effects and are mainly regulated by the endocrine and renal systems.
So, the heart pumps blood through two circuits: the pulmonary and systemic circuits. One of the most important tasks this flow of blood through the body achieves is the distribution of nutrients, including gases and what we eat, through the body, as well as the collection of waste gases and other substances for expulsion from the body.
Perfusionists are specialised clinical measurement scientists who operate the heart-lung bypass machine (also known as cardiopulmonary bypass) during heart surgery to maintain a safe and stable condition while the heart is stopped for repair. Perfusion is the technology of organ preservation by the circulation of oxygenated blood outside the body, using a heart-lung bypass machine. Some perfusionists specifically train to work in paediatrics. Perfusionists may operate a range of equipment during any medical situation where it is necessary to support or temporarily replace the patient’s cardio-pulmonary or circulatory function, including: Cardiopulmonary bypass during cardiac surgery (perfusion), Intra-aortic balloon counter-pulsation to assist circulation, Mechanical circulatory support (using ventricular assist devices), Blood salvaging and auto transfusion in a variety of surgical procedures, Extracorporeal life support (ECLS also known as ECMO), Isolated limb perfusion, Bypass for liver surgery, Organ procurement for heart or heart/lung transplantation, or Research and development associated with all of the above procedures.Perfusionists work in operating theatres in public and private hospitals (tertiary hospitals employ a team of perfusionists). Their main work is performed within a cardiac operating theatre, but they also work in intensive care units; general, orthopaedic, vascular and neurosurgical operating theatres; cardiac catheter laboratories and research laboratories.In order to practise, perfusionists must meet the following requirements: Must hold a Bachelor of Science or equivalent degree; successfully complete a recognised two- or three-year training course in perfusion theory and practice; successfully complete an examination to receive the Certificate of Clinical Perfusion awarded by the Australasian Board of Cardiovascular perfusion; and, complete continuing professional development and continuously meet the profession’s ethics and standards. For more information, see the Australian and New Zealand College of Perfusionists website.
atmospheric pressure the amount of pressure that is exerted by gases in the air surrounding any given surface
atrium (plural atria) one of two upper chambers through which blood enters the heart
alveolar duct a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli
alveolus (plural alveoli) a small air containing bag of the lung in which the bronchioles terminate
bronchi branch from the trachea into the lungs
bronchiole one of the very small tubes that branch out from the bronchi and connect to the alveoli
conducting zone organs and structures of the respiratory system not directly involved with gas exchange
expiration the process that causes air to leave the lungs
inspiration the process that causes air to enter the lungs
intra-alveolar pressure the pressure of the air within the alveoli
parietal pleura serous membrane that is the outer layer of the lungs and connects to the thoracic wall
pericardium serous membrane or sac that surrounds the heart
peristalsis wavelike contractions by the muscles of the oesophagus, or other canals of the digestive tract, to push the food towards the stomach
pleural cavity the space between the visceral and parietal layers
pulmonary circuit the path deoxygenated blood takes from the right side of the heart to the lungs and returns oxygenated blood to the left side of the heart
pulmonary ventilation the act of breathing, which can be described as the movement of air into and out of the lungs
respiratory membrane where the epithelium of the alveolus come together with the endothelium of the capillary to form a very thin membrane to allow for gas exchange
respiratory zone structures of the respiratory system directly involved in gas exchange
serous membranes thin membranes that line internal body cavities and allow for frictionless movement of organs
systemic circuit path oxygenated blood takes from the left side of the heart to most of the body’s organs and tissues and returns deoxygenated blood to the right side of the heart
ventricle one of two lower chambers of the heart through which blood is expelled from the heart
visceral pleura the serous membrane layer that is superficial to the lungs, and extends into and lines the lung fissures
Review Questions
Chapter attribution
Content adapted from:
Anatomy and Physiology 2e (2022), by J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble and Peter DeSaix, is published by OpenStax https://openstax.org/details/books/anatomy-and-physiology-2e, and used under a CC BY licence.
Concepts of Biology (2013), by Samantha Fowler, Rebecca Roush and James Wise, is published by OpenStax https://openstax.org/details/books/concepts-biology, and used under a CC BY licence.
Microbiology (2016), by Nina Parker, Mark Schneegurt, Anh-Hue Thi Tu, Philip Lister and Brian M. Forster, is published by OpenStax https://openstax.org/details/books/microbiology, and used under a CC BY licence.
Media Attributions
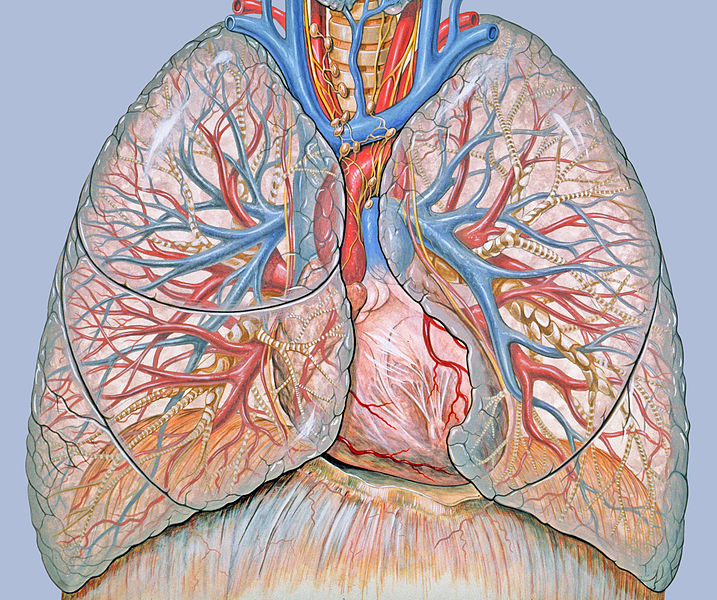
- Figure 9.0 Heart and lungs © Patrick J Lynch is licensed under a CC BY (Attribution) license
- Figure 9.2 Mountain climbers © Bayu Syaits, available under an Usplash licence
- Figure 9.3 Major respiratory structures © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.4 Bronchial tree © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.5 Respiratory zone © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.6 Structures of the respiratory zone © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix. Micrograph by University of Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 9.7 Gross anatomy of the lungs © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.8 Parietal and visceral pleurae of the lungs © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.9 Boyle’s law © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.10 Intra and interpleural pressure © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.11 Inspiration and expiration © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.12 Internal respiration © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble, Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.13 Erythrocyte and haemoglobin © OpenStax is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.14 Carbon dioxide transport © OpenStax is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.15 Normal and bronchial asthma tissues © Bruce Blaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.16 Human heart © Patrick J Lynch is licensed under a CC BY (Attribution) license
- Figure 9.17 Position of the heart in the thorax © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.18 Anatomy of the human heart © Wapcaplet is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.19 Circulatory system © J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix is licensed under a CC BY (Attribution) license
- Figure 9.20 Forearm © Colin Davis is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.21 Structure of blood vessels © Kelvinsong is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9.22 Structure of arteries and veins © Top image: J. Gordon Betts, Kelly A. Young, James A. Wise, Eddie Johnson, Brandon Poe, Dean H. Kruse, Oksana Korol, Jody E. Johnson, Mark Womble & Peter DeSaix. Micrographs by University of Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Figure 9.23 Pumping of the heart © Bruce Blaus is licensed under a CC BY-SA (Attribution ShareAlike) license

