5.3 Anti-Arrhythmic Drugs and Pharmacokinetics of Amiodarone and Digoxin
Anti-Arrhythmic Drugs and PK of Amiodarone and Digoxin
Learning Outcomes
Be able to:
- Identify and explain the different classifications of the antiarrthymic agents
- Explain the different actions on a particular part of the cardiac action potential of each class
- Identify and describe drugs that do not fit into any of those classes neatly and are classed as ‘other’.
 |
 |
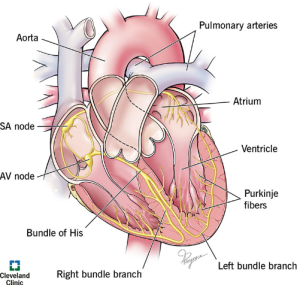
Normal cardiac conduction and electrophysiology
The heart functions via mechanical and electrical activity. Mechanical activity refers to atrial and ventricular contraction, the mechanism by which blood is delivered to tissues. When deoxygenated blood returns to the heart via venous circulation, the blood enters the right atrium. Right atrial contraction and right ventricular pressure changes result in delivery of blood to the right ventricle through the tricuspid valve. Right ventricular contraction pumps blood through the pulmonic valve and through the pulmonary arteries to the lungs, where blood becomes oxygenated. The oxygenated blood then flows through the pulmonary veins into the left atrium. Left atrial contraction and left ventricle (LV) pressure changes result in delivery of blood through the mitral valve into the LV, contraction of which results in pumping of blood through the aortic valve and to the tissues of the body. Mechanical activity is stimulated by the electrical activity of the heart.
The heart possesses an intrinsic electrical conduction system. Normal myocardial contraction cannot occur without normal function of the heart’s electrical conduction system. Depolarization of the atria results in atrial contraction, and ventricular depolarization produces ventricular contraction. Perturbation of the heart’s electrical conduction system may result in dysfunctional atrial and/or ventricular contraction and may reduce cardiac output.
Cardiac Rate and Rhythm
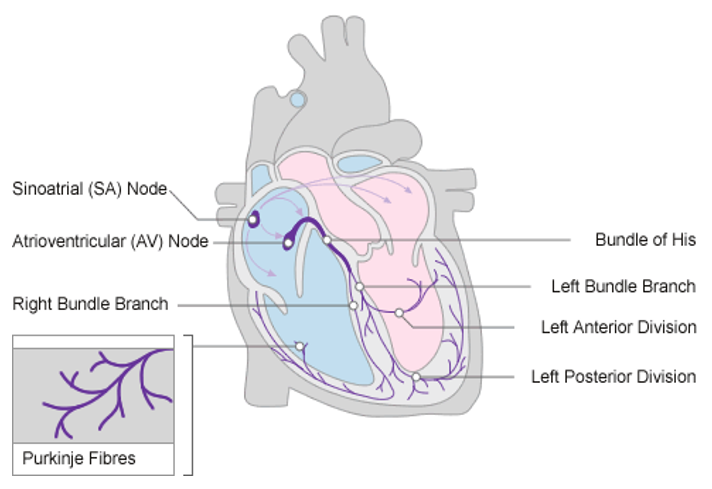
As mentioned above, the chambers of the heart normally contract in a coordinated manner, pumping blood efficiently by a route determined by the valves. Coordination of contraction is achieved by a specialised conducting system. Normal sinus rhythm is generated by pacemaker impulses that arise in the sinoatrial (SA) node and are conducted in sequence through the atria, the atrioventricular (AV) node, bundle of His, Purkinje fibres and ventricles.
Cardiac cells owe their electrical excitability to voltage-sensitive plasma membrane channels selective for various ions, including sodium (Na+), potassium (K+) and calcium ions (Ca2+), the structure and function. The electrophysiological features of cardiac muscle that distinguish it from other excitable tissues include:
- Pacemaker activity
- Absence of fast Na+ current in SA and AV nodes, where slow inward Ca2+ current initiates action potentials
- Long action potential (‘plateau’) and refractory period
- Influx of Ca2+ during the plateau
Several of these special features of cardiac rhythm relate to Ca2+ currents. The heart contains intracellular calcium channels (i.e. ryanodine receptors and inositol trisphosphate-activated calcium channels, which are important in myocardial contraction) and voltage-dependent calcium channels in the plasma membrane, which are important in controlling cardiac rate and rhythm. The main type of voltage-dependent calcium channel in adult working myocardium is the L-type channel, which is also important in vascular smooth muscle; L-type channels are important in specialised conducting regions as well as in working myocardium.
📺 Watch the brief vodcast on the review of action potential and cardiac rhythm (14 minutes)
Arrhythmias – Disturbances of Cardiac Rhythm
Clinically, dysrhythmias are classified according to:
- The site of origin of the abnormality – atrial, junctional or ventricular;
- Whether the rate is increased (>100 beats per minute [bpm] – tachycardia) or decreased (<60 bpm – bradycardia).
Cardiac arrhythmias are caused by (a) abnormal impulse initiation, (b) abnormal impulse conduction, or (c) both.
Abnormal initiation
Abnormal initiation of electrical impulses occurs due to abnormal automaticity. A decrease in sinus node automaticity results in a reduced rate of impulse generation and a slow heart rate (sinus bradycardia). Conversely, an increase in sinus node automaticity results in an increased rate of impulse generation and a rapid heart rate (sinus tachycardia). If other cardiac fibers become abnormally automatic, such that the rate of spontaneous impulse initiation exceeds that of the sinus node, or premature impulses are generated, other tachyarrhythmias may occur. Early after depolarisation (EAD) occurs during phase 2 (Ca2+ channels) or phase 3 (partially recovered Na+ channels) whereas delayed afterdepolarisation (DAD) occurs during phase 4 (high intracellular Ca2+ and inward Na+ current). Many cardiac fibers possess the capability for automaticity, including atrial tissue, the AV node, the Purkinje fibers, and ventricular muscle. In addition, fibers with the capability of initiating and conducting electrical impulses are present in left atrial myocardial sleeves that extend into the pulmonary veins. Abnormal atrial automaticity may result in premature atrial depolarizations or may precipitate atrial tachycardia or atrial fibrillation (AF); abnormal AV nodal automaticity may result in “junctional tachycardia” (so named because the AV node is also sometimes referred to as the AV junction). Abnormal automaticity originating from the pulmonary veins is a precipitant of AF. In addition, abnormal automaticity in the ventricles may result in premature ventricular complexes (PVCs) or may precipitate ventricular tachycardia (VT) or ventricular fibrillation (VF).
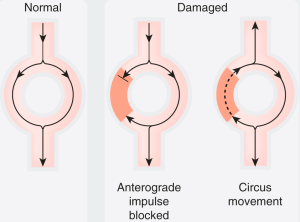
The mechanism of abnormal impulse conduction is referred to as reentry. Reentry is often triggered as a result of an abnormal premature electrical impulse (abnormal automaticity); therefore, in these situations, the mechanism of the arrhythmia is both abnormal impulse formation (automaticity) and abnormal impulse conduction (reentry). For reentry to occur, three conditions must be present. There must be: (a) at least two pathways down which an electrical impulse may travel (which is the case in most cardiac fibers); (b) a “unidirectional block” in one of the conduction pathways (this “unidirectional block” reflects prolonged refractoriness in this pathway, or increased “dispersion of refractoriness,” defined as substantial variation in refractory periods between cardiac fibers); and (c) slowing of the velocity of impulse conduction down the other conduction pathway.
📺 Watch the brief vodcast on Arrhythmias (9 minutes)
Antiarrhythmics
The antiarrhythmic drugs are used to treat and prevent cardiac arrhythmias which can be categorized into two main groups:
- Bradyarrhythmia including atrial-ventricular (AV) block, sick sinus syndrome and sinus bradycardia caused by drugs, hypothyroidism and myocardial function
- Tachyarrhythmia such as sinus tachycardia, atrial fibrillation (AF), atrial flutter, supraventricular tachycardia (SVT), reentry tachycardia, atrial tachycardia, ventricular tachycardias and premature ventricular ectopic beats.
There is a large range of antidysrhythmic drugs. In this chapter we will touch on only five as they are examples of a particular class of antiarrhythmic drug and are the more commonly used antidysrhythmic agents. Antidysrhythmic drugs are classified by their action using the following structure:
- Class 1a
- Class 1b
- Class 1c
- Class II
- Class III
- Class IV
All antidysrhythmic drugs have the potential to be pro-arrhythmic and so should be used with caution, particularly in higher doses.
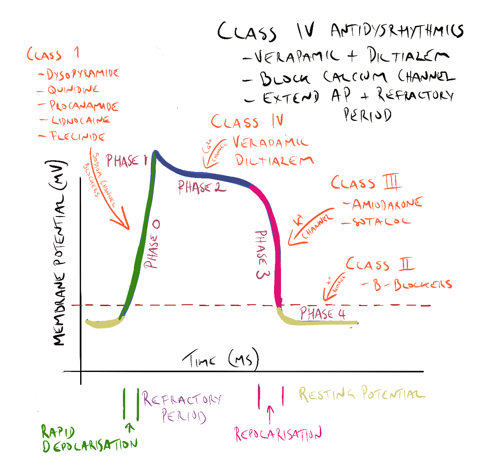
Class 1a, 1b and 1c antidysrhythmic drugs
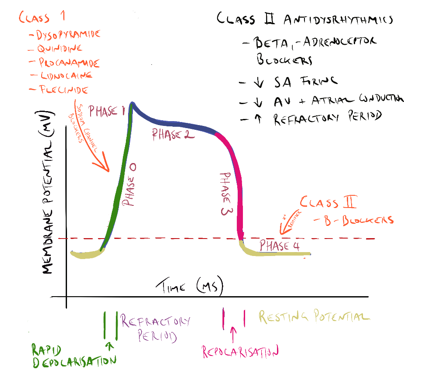
All class 1 drugs block voltage-sensitive sodium channels and interfere with the rapid influx of sodium into the cell in phase 0 of the cardiac cycle. They typically bind to the sodium channel when it is open or in the refractory phase. There are differences between the drugs in this class (hence the sub-classes) but these are not so important for the purpose of this module. What is important is they all affect sodium influx (by altering the fast sodium channel) in phase 0 of the cardiac cycle (see Figure 1). Class 1 antidysrhythmics include quinidine, procainamide, disopyramide, lidnocaine, mexiletine and flecinide.
Class II antidysrhythmic drugs
Class II drugs include atenolol, esmolol and metoprolol (discussed earlier). As discussed in a previous section, beta-adrenoceptor antagonists reduce excessive sympathetic activity by blocking the effects of catecholamines at the beta2-receptor. They also interfere with potassium concentration correction that returns intracellular potassium concentration back to normal in phase 4 of the action potential (see figure below). It is this action that increases the functional refractory period of the action potential.
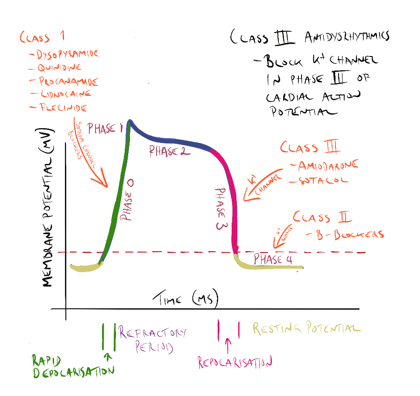
Class III antidysrhythmic drugs
Class III antidysrhythmic agents include amiodarone and sotolol. These drugs block the potassium channels in phase 3 of the cardiac cycle, effectively prolonging the action potential and increasing the refractory period of the cardiac cycle in the AV node and atrial and ventricular tissue. Amiodarone also has some effect on the sodium channels in phase 0. Amiodarone is used in the treatment of serious tachyarrhythmia’s including ventricular tachycardia AF and Supraventricular tachycardia (SVT). Amiodarone has a very long half-life. It can cause thyroid dysfunction, pulmonary toxicity and reversible corneal micro deposits. Therapeutic drug monitoring can identify compliance and toxicity but is rarely required. Amiodarone can also expose patients to skin photosensitivity manifesting in severe sunburn with limited sun exposure. Sotolol is a non-selective beta-blocker that prolongs the refractory period of the atria and ventricles and bypass tract. Sotalol also blocks the potassium channels in phase 3 of the cardiac action potential, again prolonging the action potential and increasing the effective refractory period in atrial and ventricular tissue and the AV node.
Class IV antidysrhythmic drugs
Class IV antidysrhythmic agents include the calcium channel blockers verapamil and diltiazem. These drugs have been previously discussed.
📺 Watch the brief vodcast on Antiarrhythmics from Class I to Class IV (20 minutes)
Atropine, adenosine and digoxin are used in arrhythmias. Digoxin is the final antidysrhythmic agent to be briefly examined.
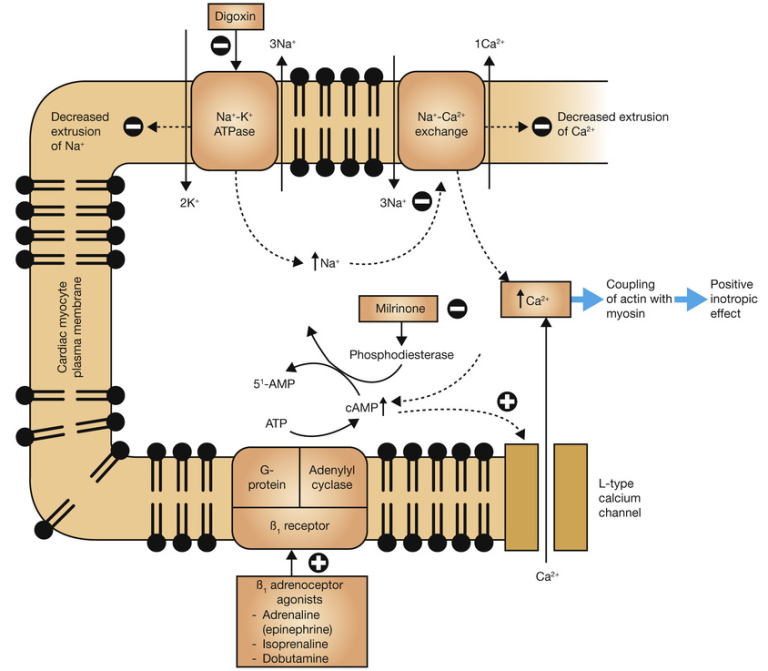
Digoxin is a cardiac glycoside used in atrial fibrillation, atrial flutter, and atrial tachycardia’s and sometimes in heart failure. Digoxin slows ventricular rate and also increases contractility of the heart. Digoxin is an inhibitor of the sodium/potassium pump in the myocardial cell. This pump is responsible for expelling intracellular sodium from the cell during repolarization – returning the cell to its original pre-depolarisation state. The binding of digoxin to the NA+/K+ ATPase inhibits its action. Elevated intracellular sodium levels prevent the removal of calcium ions making more calcium available for uptake by the sarcoplasmic reticulum (See figure below). The blockade of the NA+/K+ ATPase increases the refractory period in the atrial and AV nodal tissue (slowing heart rate) and the increased amount of calcium available to initiate actin-myosin binding increases the force of contraction.
Digoxin has a narrow therapeutic index and digoxin toxicity can be present within the normal therapeutic range for the drug. It is common for patients taking digoxin to be monitored for signs of toxicity or undergo therapeutic drug monitoring.
📺 Watch final vodcast on arrhythmias and antiarrhythmics (15 minutes)
Pharmacokinetics of Amiodarone and Digoxin
Learning Outcomes
Be able to:
- Outline the mechanism of action for Amiodarone and Digoxin
- List the Amiodarone and Digoxin Indications
- Describe the Dosages and formulations available for Amiodarone and Digoxin
- Detail the Adverse effects of Amiodarone and Digoxin
- Explain the Pharmacokinetic parameters and related chemical structures for Amiodarone and Digoxin
- Clarify the need for therapeutic drug monitoring for Amiodarone and Digoxin
- identify the Drug interactions for Amiodarone and Digoxin
- Explain Digoxin use in special populations.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.