5.2 Prevention and Management of DVT and PE
Prevention and Management of DVT and PE
Learning Outcomes
Be able to:
- Relate the pathophysiology DVT and PE to the disease and risks of untreated thrombosis.
- Identify risk factors for DVT in different patient populations
- Apply preventative strategies to reduce risk of DVT and PE in different patient populations
- Justify recommendations for the treatment of DVT and PE.
 |
 |
Introduction
We are now going to consider the two most common forms of venous thromboembolic conditions, including Deep vein Thrombosis (DVT) and Pulmonary Embolism (PE). In the last chapter we reviewed the mechanism of action of antiplatelet drugs and discussed in detail the action of anti-coagulants and the thrombolytics. This information will be helpful to understand why and how these drugs are used in the prevention and management of DVT and PE.
 Watch the introductory video on how Deep Vein Thrombosis forms. (2.06mins)
Watch the introductory video on how Deep Vein Thrombosis forms. (2.06mins)
What is a deep vein and what veins are we talking about?
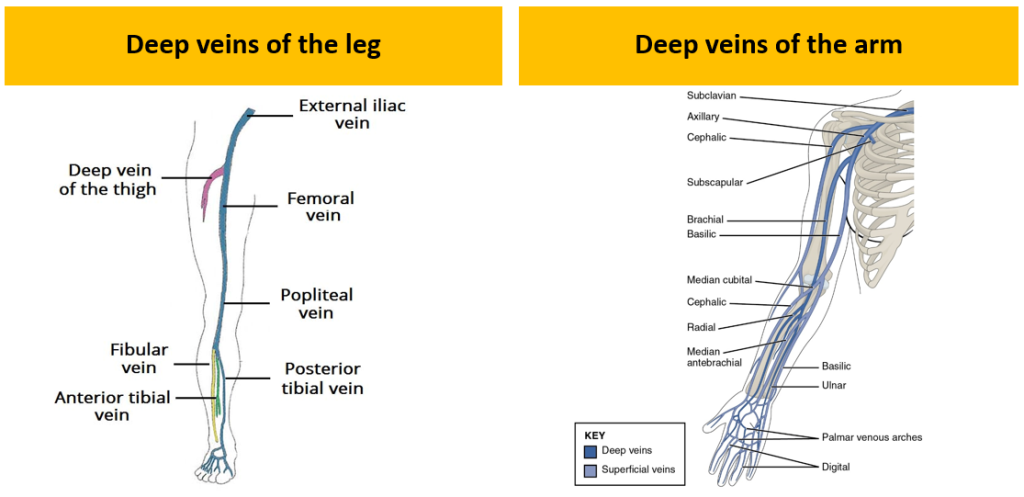
Deep veins are the veins that are deep in the body and not superficial or on the surface of the limbs and core of the body. Deep veins often run parallel to the major arteries and often share similarities in the name. The most common site for deep vein thrombus formation is in the distal or proximal deep veins of the leg show on the left hand side of the figure below. The deep veins of the arm are shown on the right of the same diagram.
Formation of Blood Clots in Distal Veins
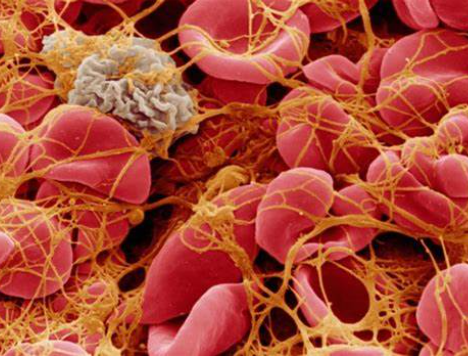
Endothelial injury to the deep vein exposes collagen and if blood stasis or hypercoagulability is present, platelet aggregation and triggering of the coagulation system occurs. This leads to thrombus formation, and a subsequent risk of emboli. Most venous thrombi begin in the valve cusps of the deep calf veins (usually due to a combination of the aforementioned risk factors). Tissue thromboplastin is released, forming thrombin and fibrin, and trap red blood cells and propagate as a red or fibrin thrombus which is the predominant venous lesion. The venous lesion is described as a ‘red clot’ as the clot is predominantly formed by red blood cells plus fibrin from the coagulation pathway. The involvement of platelets in a venous clot is much less compared to an arterial clot. The figure below shows the formation of a deep vein thrombosis on the distal side of the bicuspid valve of the popliteal vein of the right leg. It also shows a embolus forming and moving along the deep vein.
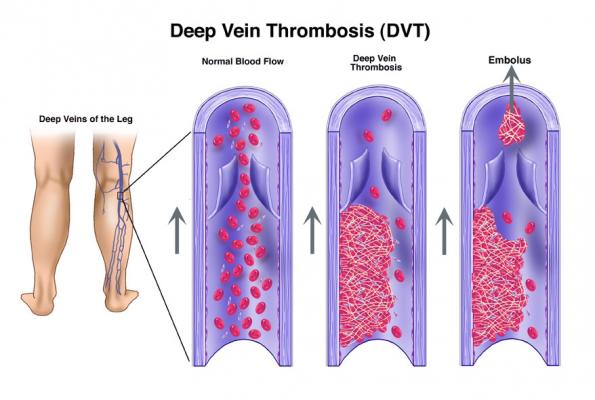
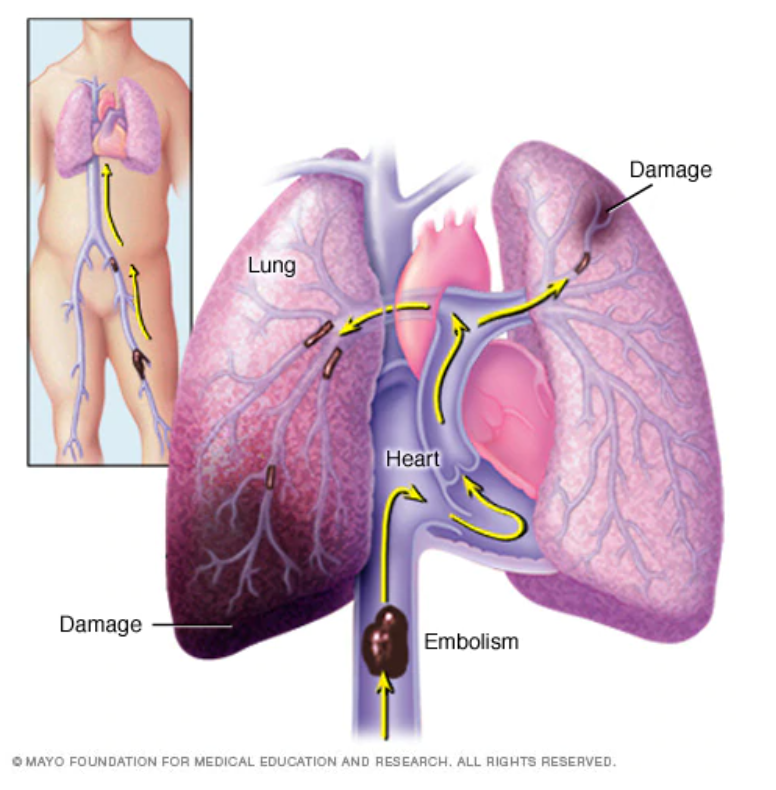
The destination of this embolus is likely the heart and eventually the lungs where it will lodge causing a pulmonary embolism. The following image shows the movement of a proximal DVT and the lodging of a embolic clot in the right lung causing a potentially fatal PE.
Signs and Symptoms of DVT
DVT may be asymptomatic or may manifest as a feeling of tenderness, pain, oedema, warmth, skin discolouration and prominent superficial veins over the affected area. The next image shows the swelling that is sometimes related to the formation of a DVT.
 While swelling of the affected limb can occur, as there are 3 veins that drain the lower leg, if only one is obstructed by thrombosis the return flow may be sufficient to prevent swelling to occur so swelling is not always present during DVT. DVT can be benign but can be lethal if a large enough pulmonary emboli occurs.
While swelling of the affected limb can occur, as there are 3 veins that drain the lower leg, if only one is obstructed by thrombosis the return flow may be sufficient to prevent swelling to occur so swelling is not always present during DVT. DVT can be benign but can be lethal if a large enough pulmonary emboli occurs.
Risk Factors for DVT
DVT is a common complication of hospital admission but simple interventions can dramatically reduce the risk of a patient suffering a DVT of PE. The risk of developing a DVT depends on:
- patient related factors (age, etc.)
- features of predisposing medical condition or
- the actual surgical procedure and it’s aftercare
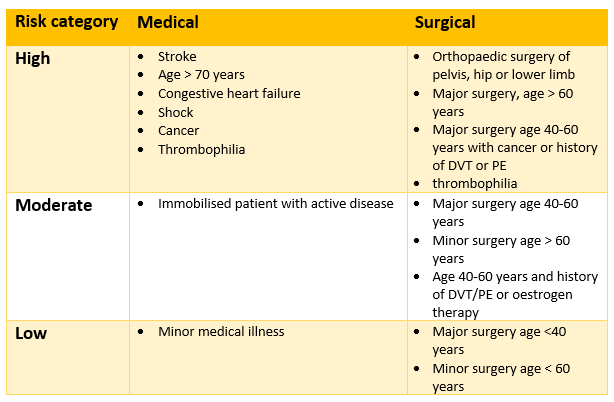
The table below stratifies risk based upon the patients characteristics and medical/surgical presentation. Individual patient risk can be assessed using a stratification tool and these tools are used to predict risk and ensure adequate prophylactic therapy is initiated during the admission.
DVT Prevention (Prophylaxis) in Hospital
There are a range of antiplatelet and anticoagulants used for the prevention of DVT during admission to hospital. In addition to the use of anticoagulants and antiplatelets, other mechanical measures such as compression stockings, adequate hydration and calf and leg movement exercises provide protection against the formation of DVT. Despite this, pharmacological prophylaxis is preferred in addition to mechanical prophylaxis as it is more effective. Selection of drug class to prevent the formation of a DVT during hospital admission in susceptible patients depends upon the individual patient risks, contraindications and reason for admission. This means the most appropriate prevention strategy will be selected based on an individual assessment of the patients’ situation and risks.
The drug classes that may be used include:
- Low-dose heparin. It is safe, cheap and effective. For prevention regimens there is no need for monitoring of APTT. While it is less expensive, it requires multiple injections a day and is less effective than LMWHs in some high risk situations (e.g. orthopedics).
- LMWHs. For example, enoxaparin.
- Factor Xa inhibitors. These include apixaban and rivaroxaban which are useful as oral anticoagulants for VTE prophylaxis after hip of knee replacement. They are more effective than enoxaparin 40mg (LMWH) with similar risk of bleeding. Fondaparinux is also ore effective than LMWHs in reducing VTE in orthopedics.
- Direct Thrombin Inhibitors. For example, dabigatran which is useful oral prophylactics for VTE prophylaxis after elective total hip or knee replacement. They have a similar efficacy and bleeding rates compared with enoxaparin (LMWH).
Treatment of DVT and PE Without Haemodynamic Compromise
The purpose of treating established DVT is to prevent thrombus enlargement or extension, PE and recurrent venous thromboembolism. Where there is no haemodynamic compromise associated with the pulmonary embolism, thrombolysis is not always necessary as the lung will begin to break the clot down naturally. In these cases the following anticoagulants alone without thrombolysis may be considered:
- Oral factor Xa inhibitors such as apixaban 10mg orally, BD for 7 days then decrease to 5mg BD Or rivaroxaban 15mg orally BD for 21 days then reduce to 20mg once daily
OR
- Direct Thrombin Inhibitors where parenteral anticoagulant (heparin/LMWH) is administered for 5 days then dabigatran is started.
OR
- Vitamin K antagonist such as warfarin which is commenced with a parenteral anticoagulant (heparin/LMWH). The heparin is ceased once INR in range (target INR 2-3).
Treatment of DVT and PE With Haemodynamic Compromise
For patients with PE and shock or hypotension, a combination of thrombolytic therapy with alteplase bolus + infusion or tenecteplase bolus followed by a LMWH or unfractionated heparin is recommended. The duration of continued treatment with the anticoagulant will depend upon the provoking factors.
 Watch the following brief vodcast on DVT and PE prevention and treatment. (26.44 minutes)
Watch the following brief vodcast on DVT and PE prevention and treatment. (26.44 minutes)
In Summary
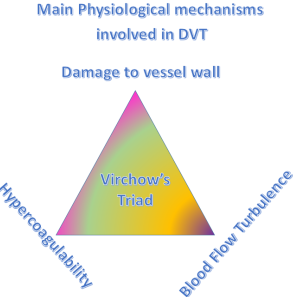
- The formation of a DVT usually involves three factors (Virchow’s Triad) – Damage to the vessel wall, hypercoagulability and turbulent blood flow.
- DVT in form in the deep veins of the arm and leg. They are capable of throwing off a emboli which can lodge in the lungs causing a pulmonary embolism.
- Aside from injury and hypercoagulability, stasis and prolonged immobilization of the legs are associated with a higher risk of DVT.
- Drug classes used to prevent and treat DVT include low dose heparin and LMWH’s, Factor Xa inhibitors and direct thrombin inhibitors.
- Mechanical measures include compression stockings, hydration and calf and leg exercises.
- Where a pulmonary embolism causes haemodynamic compromise, thrombolytic therapy is used to rapidly dissolve the clot followed by treatment with an anticoagulant for 6-12 weeks.
Download the lecture notes here
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.