8.6 Common Respiratory Conditions in Children
Learning Outcomes
- Describe the pathophysiology of bronchitis, bronchiolitis, croup and epiglottitis.
- Recognise the cardinal symptoms of croup and describe the pharmacological rationale for steroid therapy.
- Provide relevant evidence based education to patients and carers regarding the pathophysiology and treatment of bronchitis and bronchiolitis.
- Describe the appropriate signs and symptoms and referral of a patient with suspected epiglottitis
- Describe typical antibiotic and corticosteroid therapy for patients with epiglottitis.
Croup
📺 Watch the “Introduction to the Basics of Croup” (4:16 mins)
Croup is also known as laryngotrachoebronchitis. It is a common childhood disease that is characterised by brassy or barking cough accompanied by:
- a high-pitched inspiratory breathing sound called Stridor
- hoarse voice
- upper airway obstruction causing respiratory distress
- fever and
- inflammation of the mucous membrane of the nose.
The croup cough is distinctive – it has a brassy or bark-like sound that once heard is difficult to forget. The following two links will take you to a series of YouTube videos so you can listen to the sounds of croup:
Note the barking / brassy sound of the cough in both. The third link takes you to the sound of stridor (a high pitched inspiratory wheeze). The duration of symptoms is short – around 2-5 days untreated but a persistent post-viral cough can be experienced for some weeks after the symptoms of croup cease. Mortality rates for croup have declined and death is now relatively uncommon.
The cough and stridor more commonly are experienced late in the evening or early in the morning. Croup is most common in children under the age of 3 years but can occur at any age.
The most common cause of croup is viral, parainfluenza being the most common cause. Other causes include RSV (Respiratory syncytial virus), influenza, adenoviruses, or enteroviruses. Parainfluenza (and the other less common causes of croup) is transferred by inhaling respiratory droplets expelled in the air when an infected individual coughs or sneezes. Residual virus on surfaces such as table tops and door knobs is another common mechanism of spread. This is why parents are commonly asked to isolate their child for 3-4 days(or until they are feeling well) – it prevents the spread of virus (and therefore croup) to other children.
Croup is a self-limiting disease that is relatively easily treated with corticosteroids (usually medium to long acting such as prednisolone, prednisone, dexaethasone or nebulised budesonide). It is useful to remember the relative duration of action of the different steroids
- Hydrocortisone and cortisone – short acting (8-12 hours) and relatively lower glucocorticoid activity
- Prednis(ol)one, methylprednisolone, nebulised budesonide and triamcinolone – intermediate acting (12-36 hours) and relatively potent glucocorticoid activity.
- Dexamethasone and betamethasone – long acting (36-72 hours) and very potent glucocorticoid activity
The corticosteroids in bold are the ones commonly used in the management of childhood croup. Of these, prednisone or prednisolone are the most commonly prescribed corticosteroid probably due to cost, experience in prescribing and availability in a oral liquid dosage form.
In severe cases of croup, children may be given nebulised adrenaline (1:1000 x 5 ml) then corticosteroids as per mild to moderate croup. It is important to remember the benefit of adrenaline may only last for 2 hours and so these children will require observation to identify rebound airway obstruction.
📺 Watch the video on “The signs and symptoms, pathophysiology and treatment of children with croup (16:49 minutes).
Bronchitis and Bronchiolitis
Both bronchitis and bronchiolitis are acute self limiting conditions of the bronchus and bronchioles. They are both most commonly caused by viral infections such as:
- Influenza
- Respiratory syncytial virus (RSV)
- Parainfluenza virus
- Adenoviruses
(wow, those causes have much overlap with the cause of croup eh!) In the case of bronchitis, is it less commonly caused by bacteria such as Mycoplasma peumoniae and Chlamydophila pneumonia. Due to this there is no need for antibiotic therapy in either bronchitis or bronchiolitis unless there is a suspected secondary bacterial lung infection.
Patients experiencing bronchitis or bronchiolitis experience weeks of cough, which is anxiety provoking and frustrating. This often leads to (often inappropriate) requests for antibiotic therapy as the patient is just sick of coughing (or listening to their child coughing). This leads to pressure to inappropriately prescribe antibiotics or dissatisfaction with the outcome after the doctors consult where antibiotics are not . In these cases, it is useful for the pharmacist to communicate the risks of inappropriate antibiotic prescribing to educate the patient and support the prescribers usually correct decision.
Much like bronchitis, bronchiolitis is self limiting and typically caused by a viral infection that starts as a upper respiratory tract infection. Bronchiolitis is more common in children 1-year of age or younger. It tends to peak in severity around day 2 or 3 and resolved within 7-10 days. Most cases of bronchiolitis are managed in the home environment, but admission may be required in more severe cases where oxygen, hydration and feeding support is necessary.
📺 Watch the video on “Bronchitis and Bronchiolitis” (7:41 mins)
Epiglottitis
Epiglottitis is a medical emergency.
Epiglottitis is uncommon but severe inflammation of the epiglottis and surrounding tissue that has the potential to cause occlusion of the larynx and respiratory obstruction. It is commonly caused by a bacterial infection such as Haemophilus influenza type B or Streptococcus pneumoniae, and the incidence has declined (particularly in children) since the universally adopted immunization schedule against Haemophilus influenza type B with the Hib vaccine at 2, 4, 6 and 18 months of age.
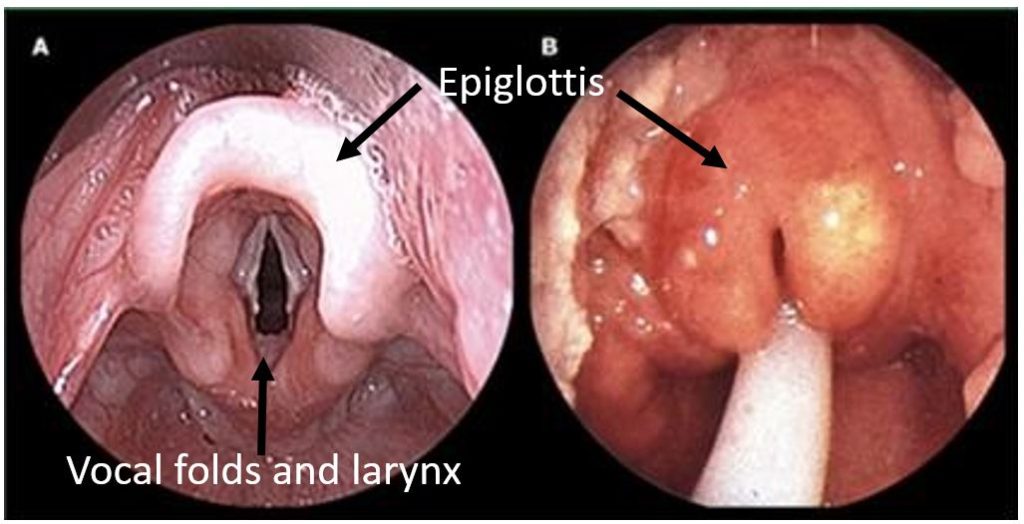
The figure below shows (A) the normal epiglottis and vocal folds and (B) epiglottitis with an endotracheal tube inserted. You can see the potential occlusion of the larynx caused by the inflamed epiglottis and surrounding tissue.
The symptoms of epiglottitis typically appear suddenly and include:
- Severe throat pain
- Difficulty / pain swallowing
- Fever
- Drooling
- Change in voice – sounds muffled.
If a patient presents with symptoms suggestive of epiglottitis, it is critical no one attempts to look in their throat at all – this risks an immediate airway occlusion. The patient should be kept calm and transported to hospital by ambulance immediately.
Treatment of epiglottitis is relatively straight forward. The mainstay of therapy is airway support (intubation or tracheotomy if airway is lost), IV antibiotics and maybe IV steroids. As patients improve they are often transitioned to oral therapy. Common IV antibiotic therapy that cover the typical infective agents (Haemophilus influenza type B or Streptococcus pneumoniae) are:
- ceftriaxone or
- cefotaximine or
- moxifloxacin
The IV corticosteroid of choice is dexamethasone – it is both potent in terms of its glucocorticoid action and has a long duration of action. It is also available in a parental form avoiding oral administration. It is important to note patients with epiglottitis may also have septicemia.
📚 Read/Explore
- Review the Australasian Bronchiolitis Guidelines – read the Summary of pages 1-8 (this will take you about 10 minutes – it is quick).
- Australasian-bronchiolitis-guideline
