5.4 Atrial Fibrillation
Atrial Fibrillation
Learning Outcomes
Be able to:
- Define what atrial fibrillation is and the different types
- List the possible symptoms / clinical manifestations
- Describe the epidemiology and risk factors
- Explain the approach to screening and diagnosis
- Describe the sequelae / prognosis
- Explain the approach to management of atrial fibrillation
- Compare and contrast options for the treatment of the dysrhythmia itself (i.e., rate vs rhythm control)
- Provide individualised advice as to whether or not therapeutic anticoagulation is required for prevention of thromboembolic complications
- Outline the option(s) and justify your recommendations If anticoagulation is indicated, list the special considerations associated with triple therapy (i.e., DAPT plus anticoagulation in AF).
 |
 |
Introduction
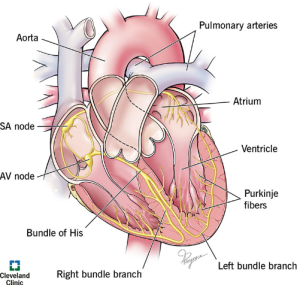
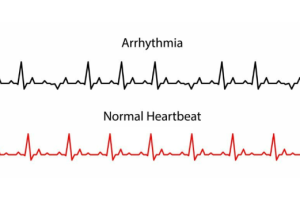
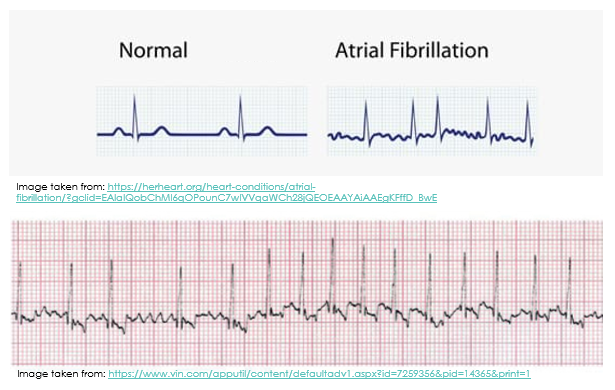
Atrial fibrillation (AF) can be defined as “a supraventricular tachyarrhythmia with uncoordinated atrial electrical activation and consequently ineffective atrial contraction”
📺 Watch the following video on a depiction of atrial fibrillation.
When the atria contract and twitch randomly and out of rhythm, sometimes the P wave on the ECG is not discernible at all. Other times, like you can see in the diagram below, it appears as though there are multiple P waves before any given QRS complex (you will remember that the QRS complex indicates ventricular depolarisation).
Types of Atrial Fibrillation (AF)
When considering the different types of atrial fibrillation, as pharmacists, it is most important that we know whether the patient has valvular atrial fibrillation OR non-valvular atrial fibrillation.
- Valvular atrial fibrillation
- Atrial fibrillation affecting a patient with moderate to severe mitral stenosis or a prosthetic heart valve
- Necessitates therapeutic anticoagulation with warfarin (see later)
- Non-valvular atrial fibrillation
- Atrial fibrillation that is not associated with moderate to severe mitral stenosis or a prosthetic heart valve
Clinical Manifestation
- AF is commonly asymptomatic. It has been estimated that 1.4% of patients in our communities aged 65 years or more will have unknown/undiagnosed, asymptomatic AF at a single point in time random screening of their ECG trace.
- For patients who do experience symptoms associated with their AF, examples of such symptoms include palpitations, dyspnoea, symptomatic hypotension (e.g., dizziness, fatigue, confusion), and/or chest pain or discomfort.
Epidemiology
AF is the most common recurrent arrhythmia encountered in clinical practice. The prevalence of AF in Australia is estimated to be 2-4% but this is likely to be an underestimation since AF commonly exists undiagnosed.
Complications of AF
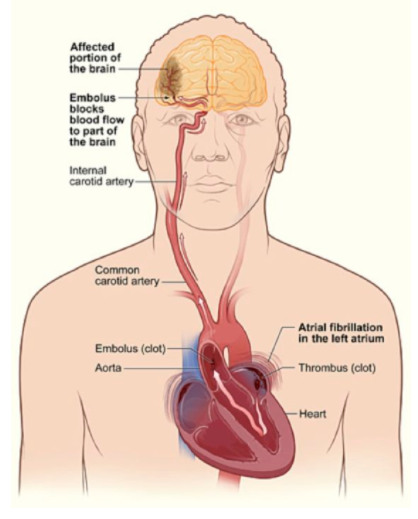
Thromboembolic consequences of AF are a cause of substantial morbidity and mortality. These include embolic stroke and pulmonary embolism. When the heart is not pumping blood in a coordinated manner from the atria to the ventricles, there is an increased chance of blood pooling and subsequently clotting within the heart.
- If a clot is ejected from the left side of the heart, this can cause an embolic stroke.
- If a clot is ejected from the right side of the heart, this can cause a pulmonary embolism.
Other possible complications of AF include myocardial infarction and heart failure.
📺Watch the following lecture video (22.46 min) for a more comprehensive introduction to atrial fibrillation.
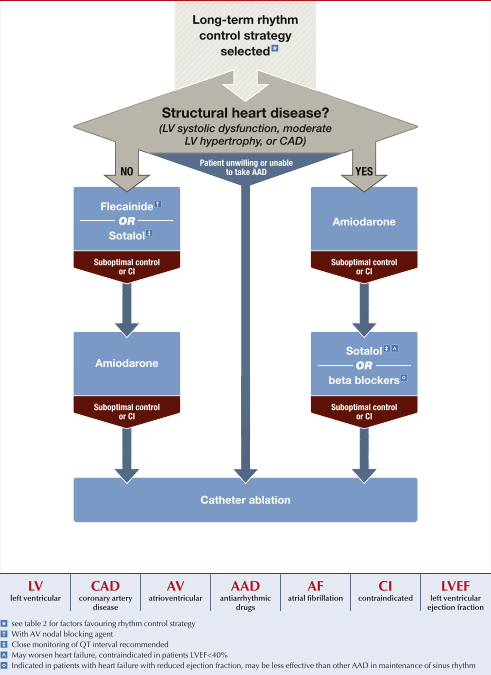
Approach to Treatment of AF
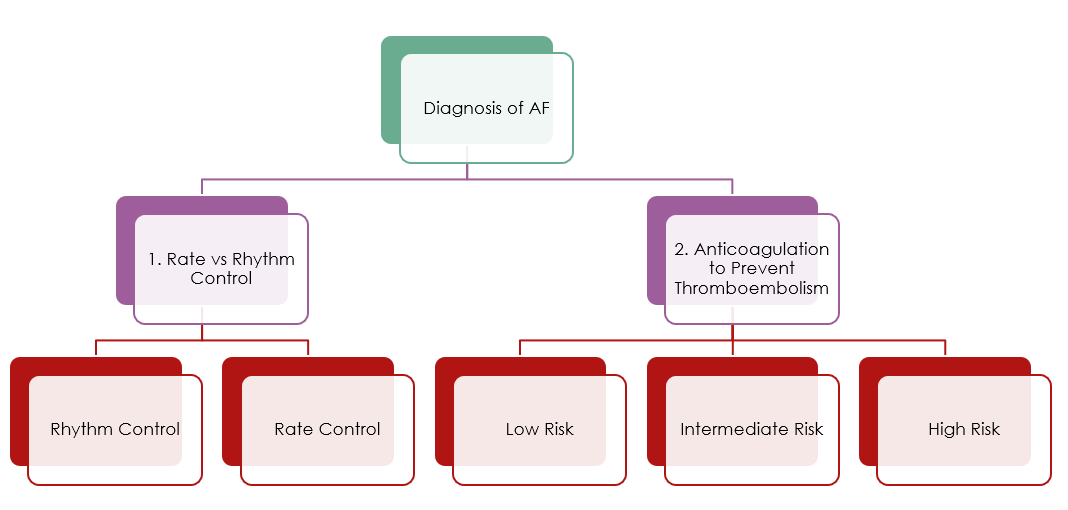
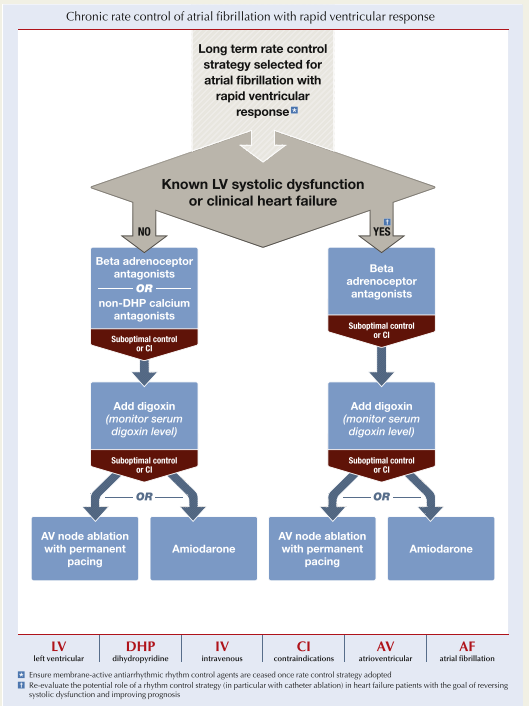
- The first decision is whether or not to try to revert the patient back into sinus rhythm using a rhythm control approach as opposed to rate control. The decision (and chosen pharmacological agents) will heavily depend on whether or not the patient has concomitant heart failure. In general, rhythm control can be achieved using electrical cardioversion or pharmacological cardioversion with drugs like flecainide or amiodarone. Rate control may be achieved using drugs like beta blockers or non-dihydropyridine calcium channel blockers (verapamil or diltiazem).
- The second decision is whether or not to use anticoagulation to prevent thromboembolism. This will be a decision that the doctor should make in consultation with the patient (and ideally the pharmacist!) using a shared decision making approach with an overall assessment of the relative risks of clotting vs bleeding.
📚Read/Explore:
- Read the NHF Patient Information Brochure attached below to help to solidify your understanding of AF and your ability to communicate your knowledge to patients. You might notice some of the drugs are spelt incorrectly! But we’ll talk a closer look at the available treatment options for AF soon.
- Review National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand. Australian Clinical Guidelines for the Diagnosis and Management of Atrial Fibrillation 2018. National Heart Foundation website. https://www.heartlungcirc.org/action/showPdf?pii=S1443-9506%2818%2931778-5.
- Read Atrial Fibrillation. In: eTG complete (Cardiovascular). Therapeutic Guidelines. Updated August 2022.
Management of AF
The pharmacological treatment of AF will follow either a rate control strategy or a rhythm control strategy.
Rate control will aim to slow conduction through the AV node and control the ventricular rate, thereby preventing irregular atrial signals from impacting on the ability of the ventricles to contract effectively. As such, rate control will help to maintain cardiac output. In contrast, rhythm control aims to treat the atrial fibrillation by reverting cardiac conduction back into a normal sinus rhythm.
- There is no significant difference in morbidity and mortality outcomes associated with one approach over another. Either rate control or rhythm control are generally acceptable approaches to the treatment of AF. In practice, rate control is often favoured because the antiarrhythmic agents used to achieve rhythm control are not as well tolerated as the agents used for rate control.
However, some factors make rhythm control more likely to be effective and perhaps a bit better tolerated too. For example, rhythm control may be more likely to be the chosen approach to treatment of AF for patients who are younger, and more physically active. Also, if a person with both AF and heart failure can tolerate a rhythm control approach, then rhythm control could have more benefits for them.
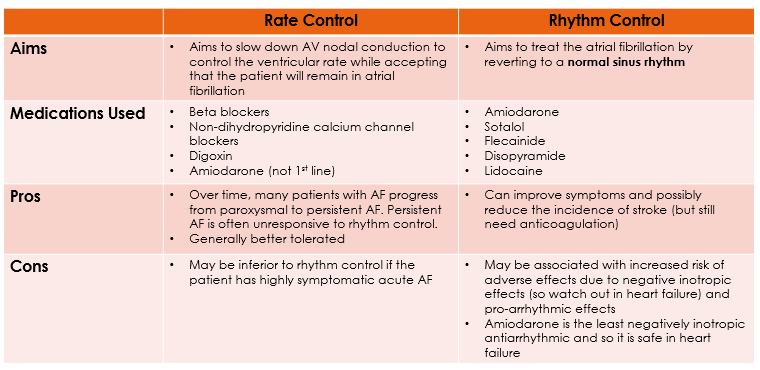
Rate Control in AF/Rhythm Control in AF
Anticoagulation in AF
member that AF itself rarely causes death. Rather, mortality is associated with thromboembolic complications of AF. Hence, why AF is an important indication for anticoagulants. The anticoagulants that we’ll talk about have proven morbidity and mortality benefits. But they are also associated with a risk of major bleeding.
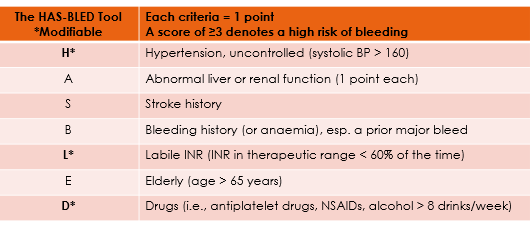
The CHA2DS2-VA score is recommended to assess stroke risk in non-valvular AF.
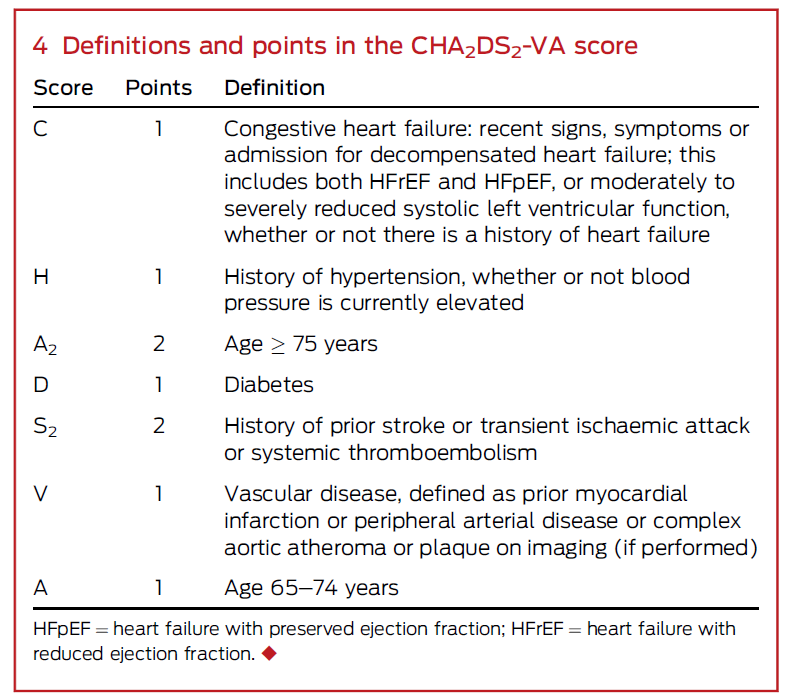
- Anticoagulation is not recommended if the CHA2DS2-VA score is 0
- Anticoagulation is recommended if the CHA2DS2-VA score is ≥ 2
- Unless there are contraindications to anticoagulation
- Anticoagulation should be considered if the CHA2DS2-VA score is 1
- Decision is made by the doctor and patient together with careful evaluation of risk/benefit
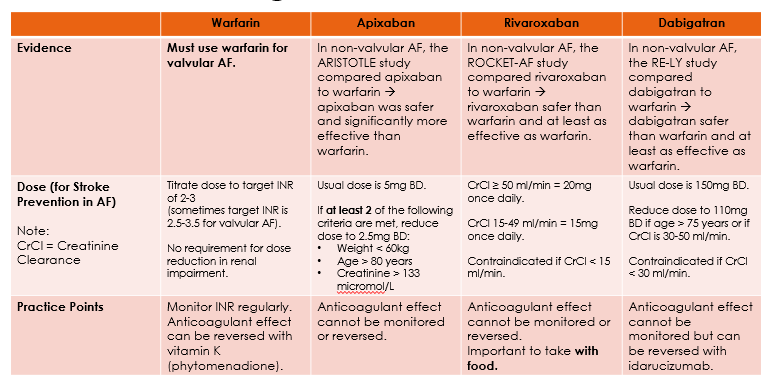
- Anticoagulant options include warfarin and the non-vitamin K antagonist oral anticoagulants (NOACS)
- NOACs include apixaban, rivaroxaban, and dabigatran
- NOACs are preferred over warfarin in non-valvular AF
For patients with valvular AF (that is AF with moderate to severe mitral stenosis or a mechanical heart valve), we already know that they are at high risk of thromboembolism and so these patients should be anticoagulated with warfarin. Other anticoagulants besides warfarin must not be used to prevent thromboembolic complications of valvular AF.
📺Watch the following lecture video (22.46 min) for atrial fibrillation Part 2.
COMMONWEALTH OF AUSTRALIA Copyright Regulations 1969 WARNING
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.