8.3 Asthma
Learning Outcomes
Be able to:
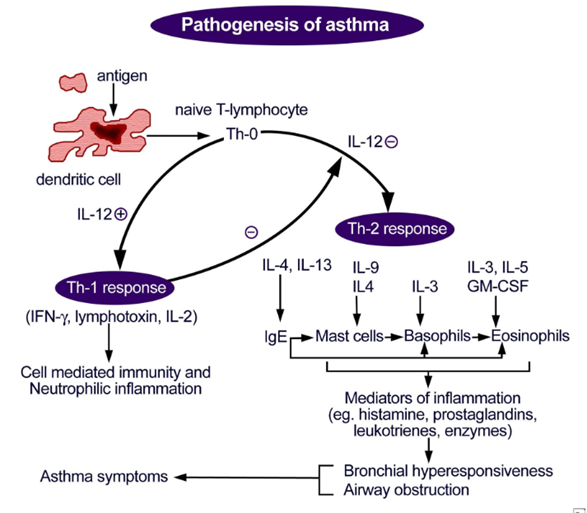
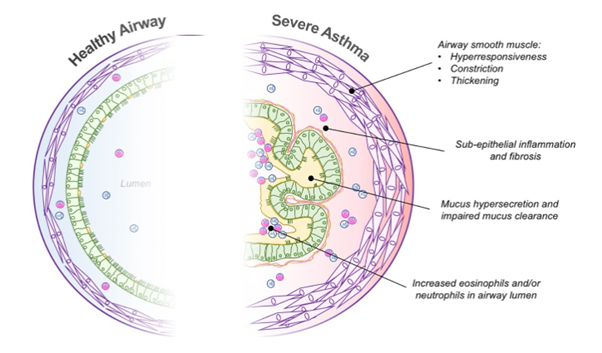
- Explain the pathophysiology and clinical presentation of asthma
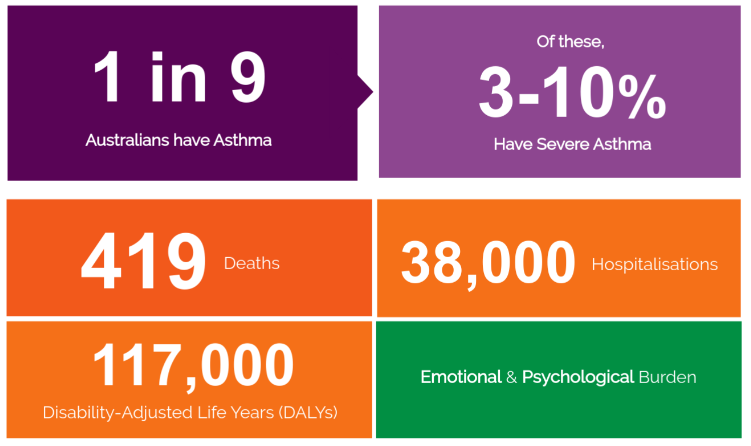
- Describe the prevalence of asthma and its impact on the Australian population
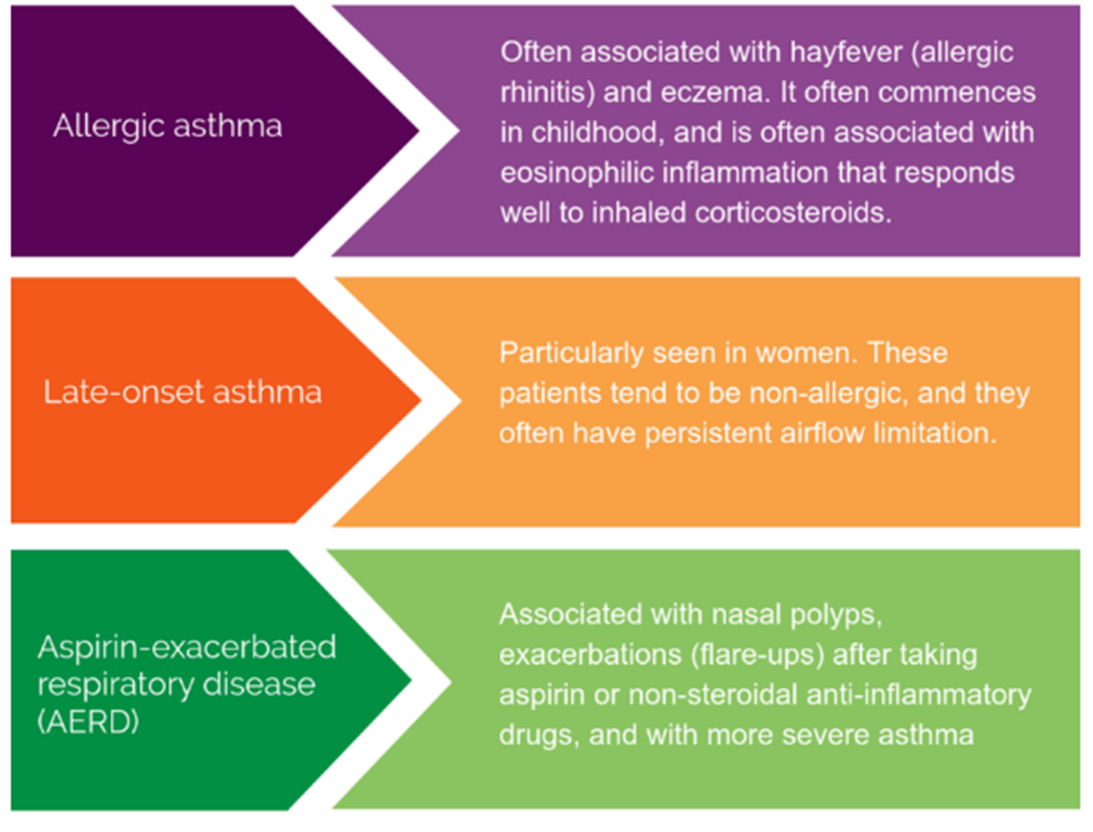
- Differentiate between the different forms of asthma
- Recognise the risk factors for asthma
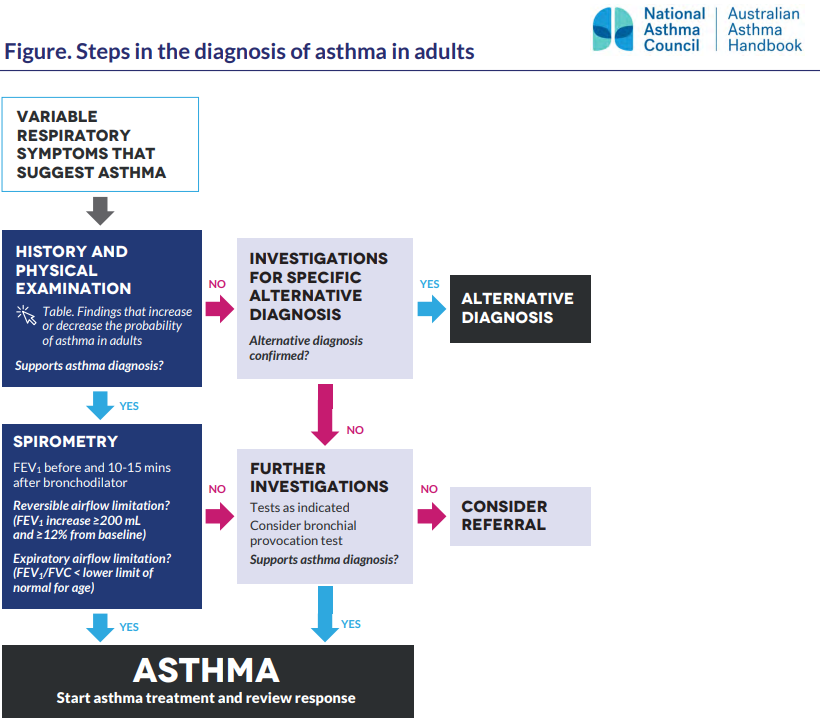
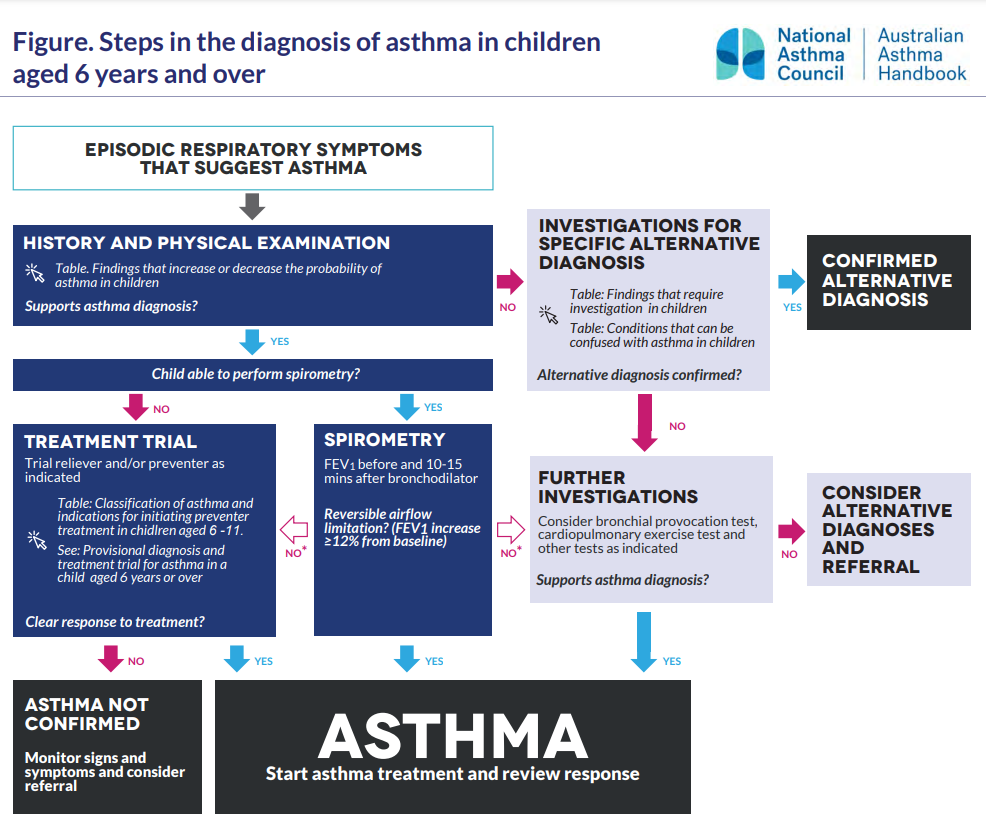
- Relate the diagnostic criteria and investigations to new presentations and ongoing asthma control
- Relate the mechanism of action of medications commonly used to the treatment of asthma
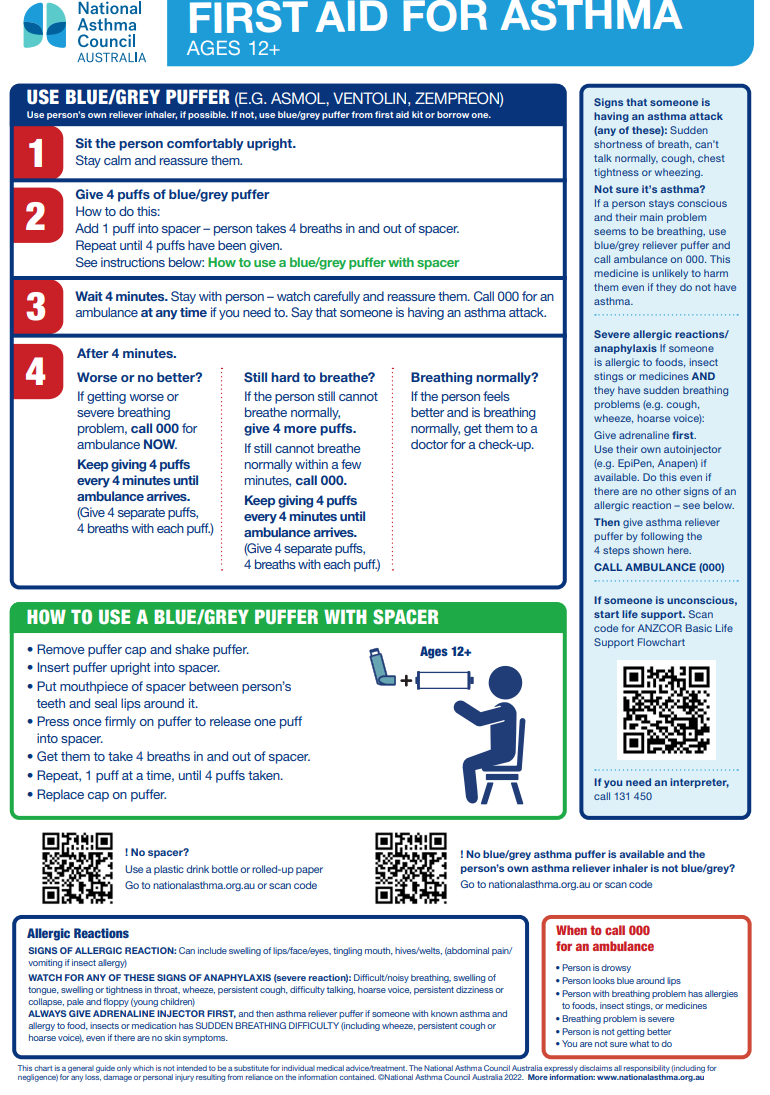
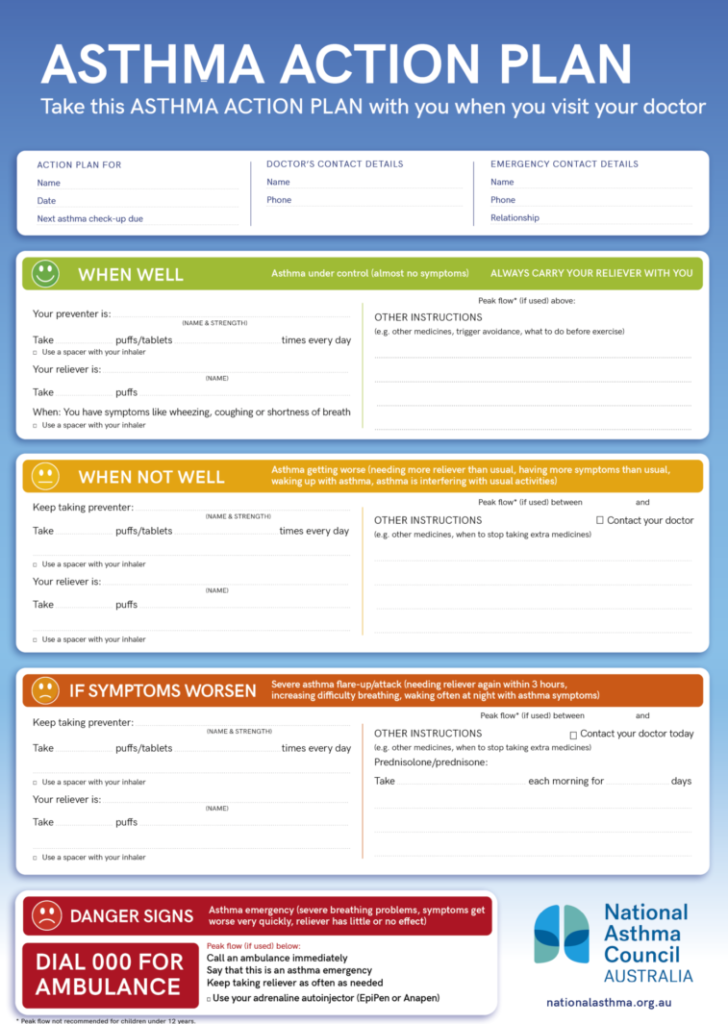
- Provide basic advice and clinical management for presentations of asthma.
Lifestyle Advice for Asthma
The mainstay of non-pharmacological management and lifestyle advice for asthma is the avoidance or management of triggers, adoption of healthy lifestyle, self management and ongoing review. Use the accordion below to find out more.
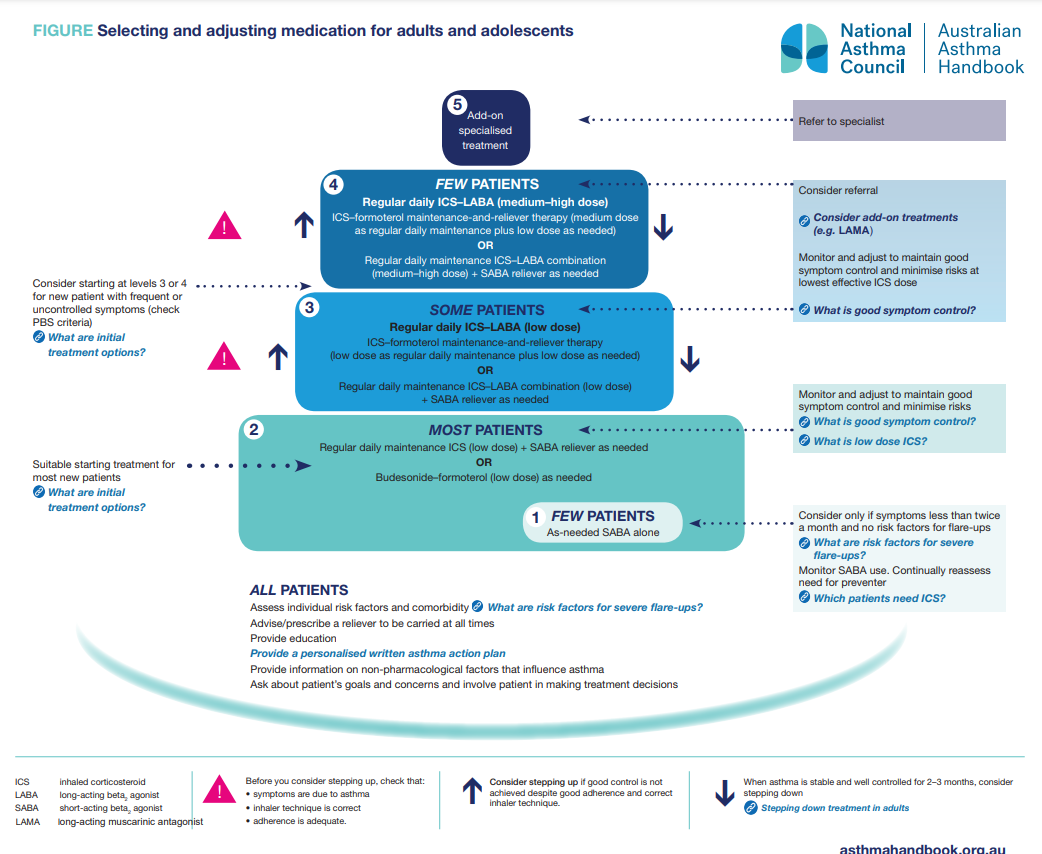
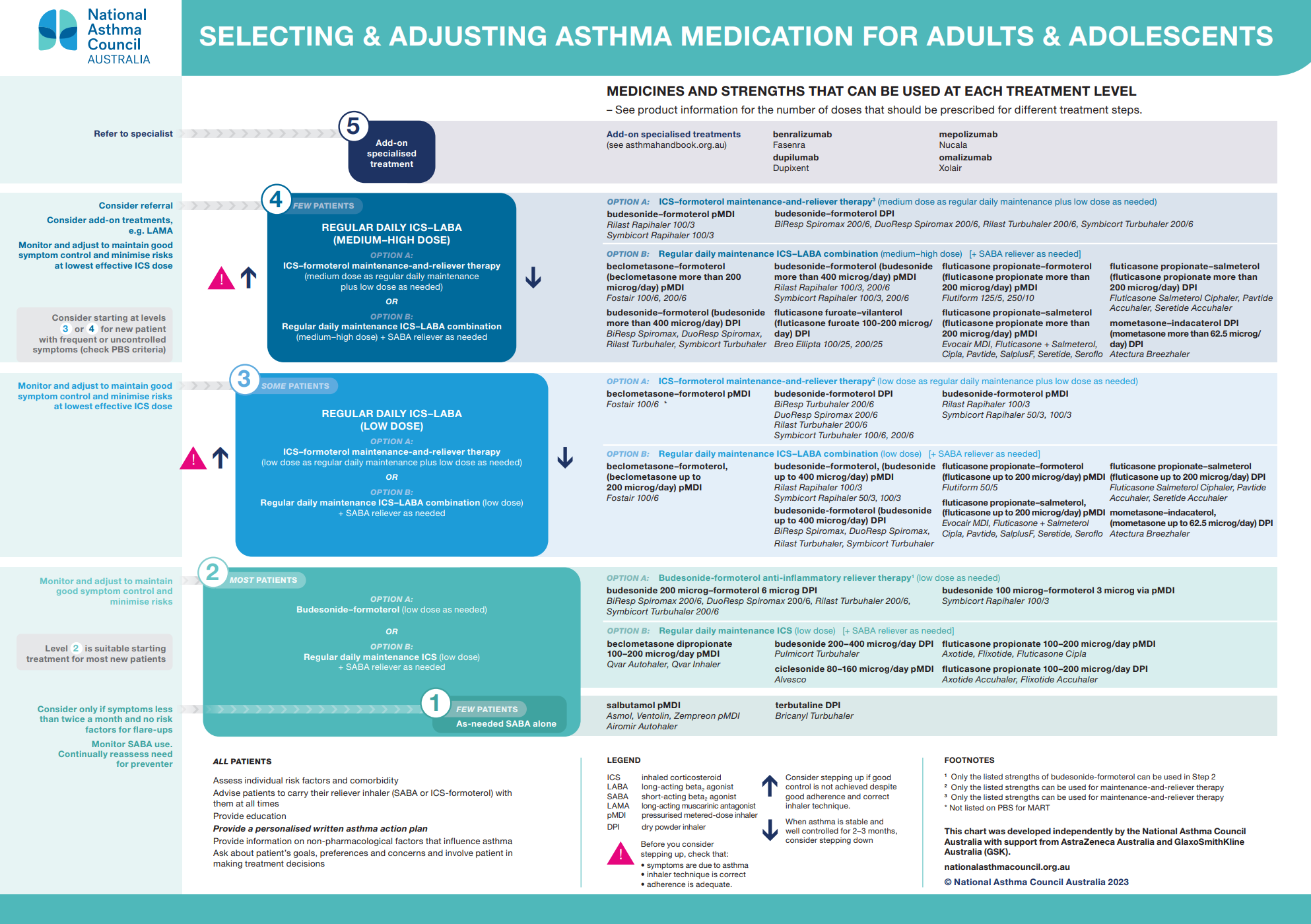
Stepping Up
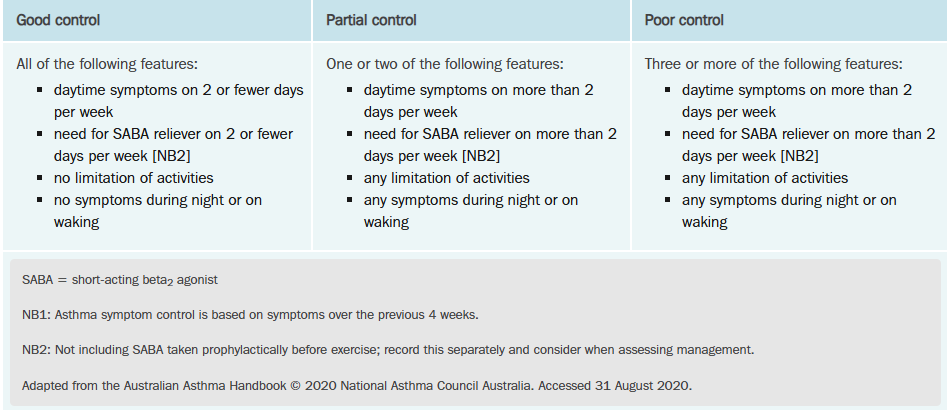
The aim of management of asthma in adults and adolescents is to maintain a normal quality of life, free of asthma symptoms and exacerbations, and without adverse effects of asthma treatment. It also aims to prevent long-term lung damage. Drug treatment for asthma in adults and adolescents is introduced in a stepwise manner. Most patients start at Step 2 and initial treatment options include either regular daily low dose ICS + SABA as needed, or, low dose budesonide-formoterol as needed. The patient should be monitored and pharmacotherapy adjusted to maintain good symptom control whilst minismising adverse effects. What is considered “good” symptom control? We discuss this later in the module. If after 4-6 weeks the patient does not have good asthma control and the symptoms are due to asthma, inhaler technique is correct and adherence is adequate, the prescriber can consider stepping up the regimen.
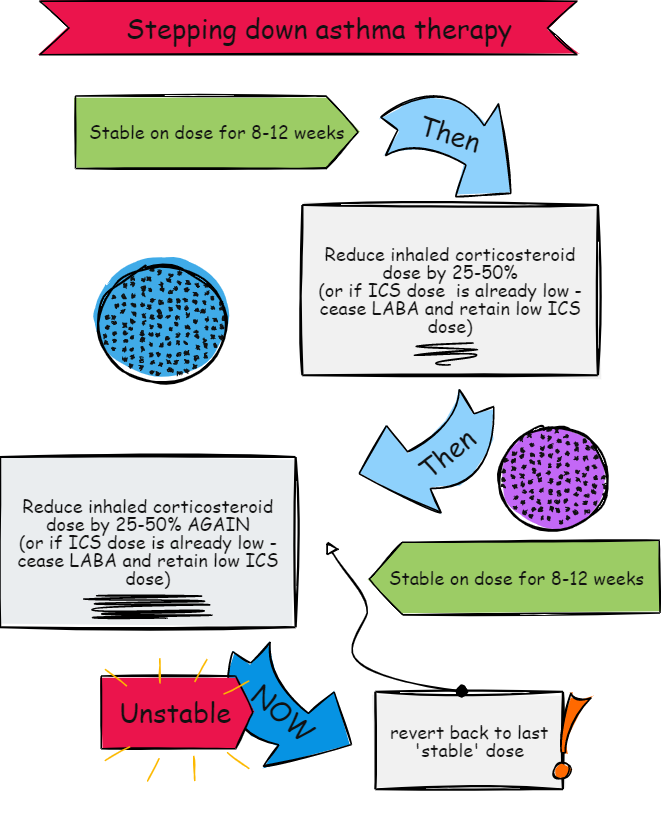
Stepping Down
📺 Watch this video on asthma management in adults. Please note that the video was created before the National Asthma Council Asthma Handbook was updated so the images of the algorithms look different. The premise of stepping up and stepping down is the same, however. Also note that LRTA (montelukast) is not used in adults anymore and that cromylons are no longer used.
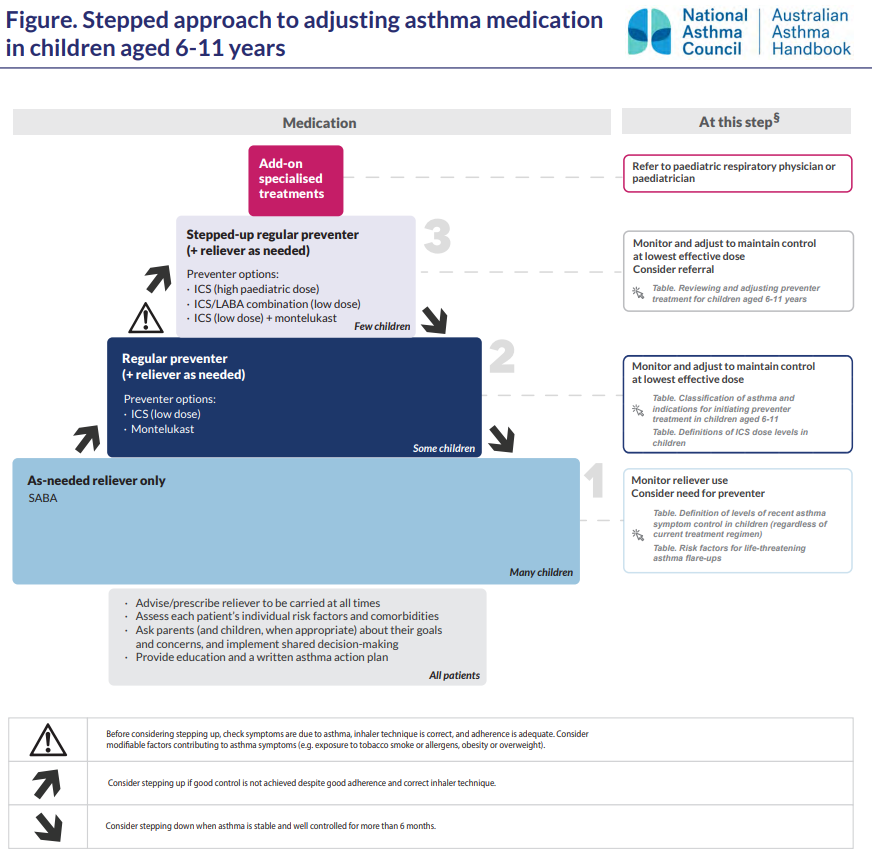
Pharmacological Management of Asthma In Children > 6 years
The following accordion may help to understand the diagram above:
Stepping Up
In children aged over 6 years, a diagnosis of asthma can be made with more certainty as school-aged children are likely to be able to perform spirometry. We have already discussed how the presence of reversible (variable) expiratory airflow limitation on spirometry supports the diagnosis of asthma after history and clinical findings increase the likeness of asthma. Most children aged 6-11 years are able to maintain good asthma control with use of a SABA as needed. Some children require preventer treatment with regular daily low dose lCS + SABA as needed or regular daily LTRA + SABA as needed. Indications for initiating preventor treatment in children aged 6-11 years include any of the following:
- Flare-ups every 6 weeks or more often
- Persistent asthma symptoms
- Daytime asthma symptoms > once per week or night-time symptoms > twice per month
- Severe flare-ups, irrespective of the frequency of flare-ups or symptoms between flare-ups
If symptom control is not maintained despite good adherence and inhaler technique, the dose of the ICS may be increased or a combination of regular daily low dose ICS-LABA or regular daily low dose ICS-LTRA + SABA as needed may be added.
Stepping Down
Consider stepping down when asthma is stable and well controlled for more than 6 months.
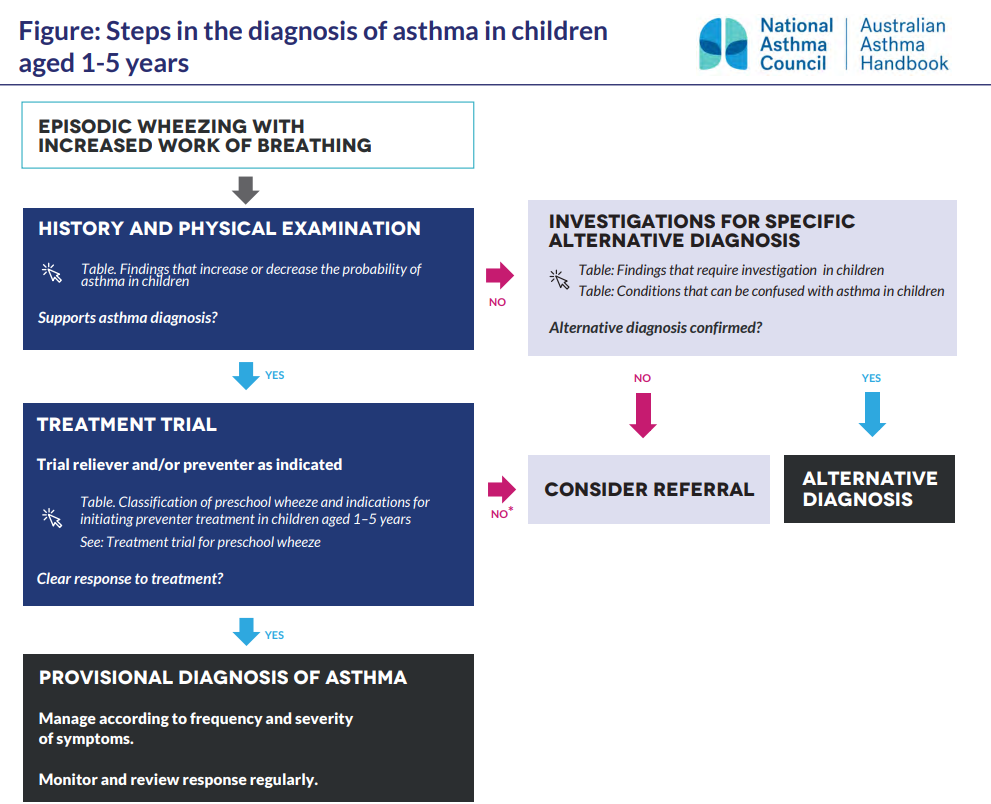
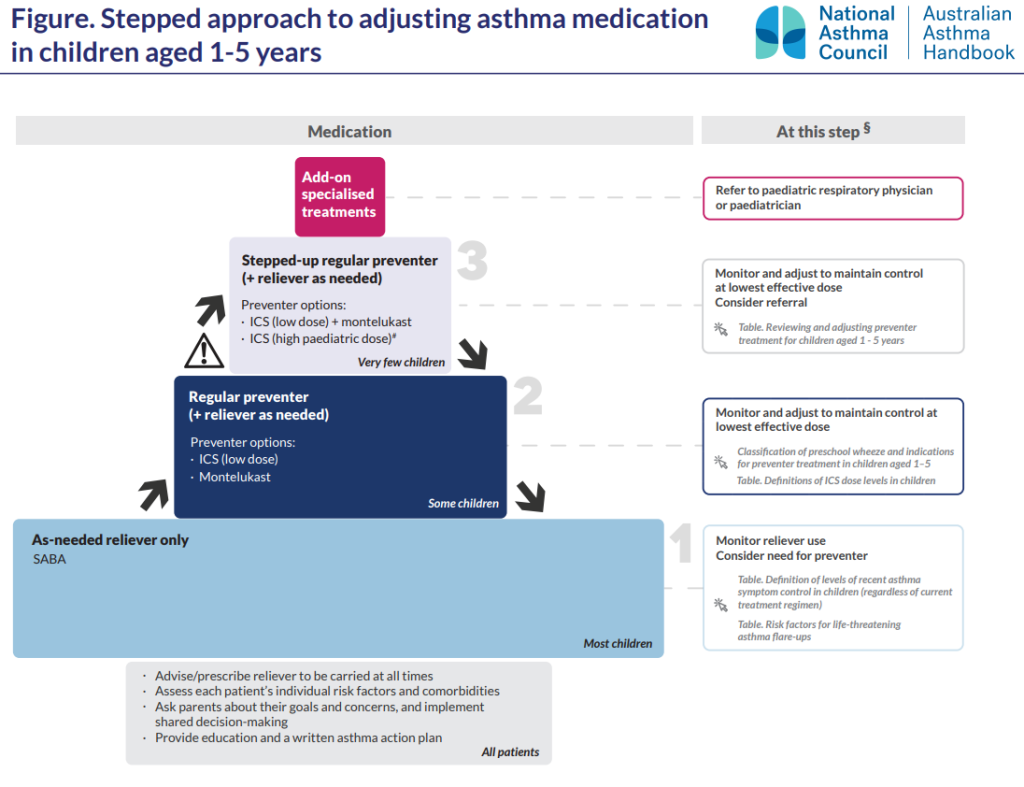
Pharmacological Management of Asthma In Children < 6 Years
The following accordion may help to understand the diagram above:
Stepping Up
For all children with asthma or salbutamol-responsive preschool wheeze, a reliever and inhaler device suitable for the child’s age is prescribed. Some children aged 2 years and older with frequent symptoms (e.g., wheeze, cough or breathlessness at least once per week) or a history of severe flare-ups (e.g. requiring emergency department visits, intensive care or hospitalisation) may require preventor treatment. A regular daily low dose ICS + SABA as needed or LTRA + SABA as needed can be used to maintain good asthma control. Very few children require regular daily low dose ICS+LTRA + SABA as needed or high paediatric dose ICS + SABA as needed which warrants specialised care.
Stepping Down
Stepping down can be considered by the prescriber when asthma has been well controlled for 6 months. This will help identify the minimal dose or regimen needed to maintain control and may minimise the risk of treatment-related adverse effects and help identify the minimal dose or regimen needed to maintain control.
📺 Watch this video on asthma management in children. Please note that the video was created before the National Asthma Council Asthma Handbook was updated so the images of the algorithms look different. The premise of stepping up and stepping down is the same, however. Also note that cromylons are no longer used.
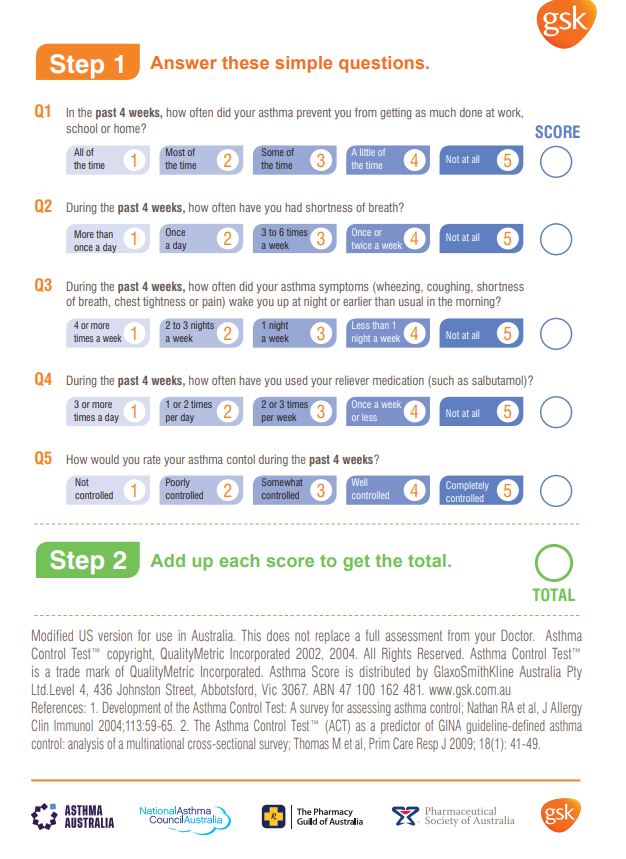
Asthma Control
This material has been reproduced and communicated to you by or on behalf of James Cook University in accordance with section 113P of the Copyright Act 1969 (Act).
The material in this communication may be subject to copyright under the Act. Any further reproduction or communication of this material by you may be the subject of copyright protection under the Act. Do not remove this notice.